Pediatr Emerg Med J.
2023 Oct;10(4):124-131. 10.22470/pemj.2023.00794.
Characteristics of children hospitalized through the pediatric emergency department and effects of pediatric emergency ward hospitalization
- Affiliations
-
- 1Department of Emergency Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Republic of Korea
- KMID: 2546286
- DOI: http://doi.org/10.22470/pemj.2023.00794
Abstract
- Purpose
To evaluate the efficiency of the pediatric emergency ward (PEW) through the outcomes of children hospitalized to the ward by the department of pediatric emergency medicine (PEM).
Methods
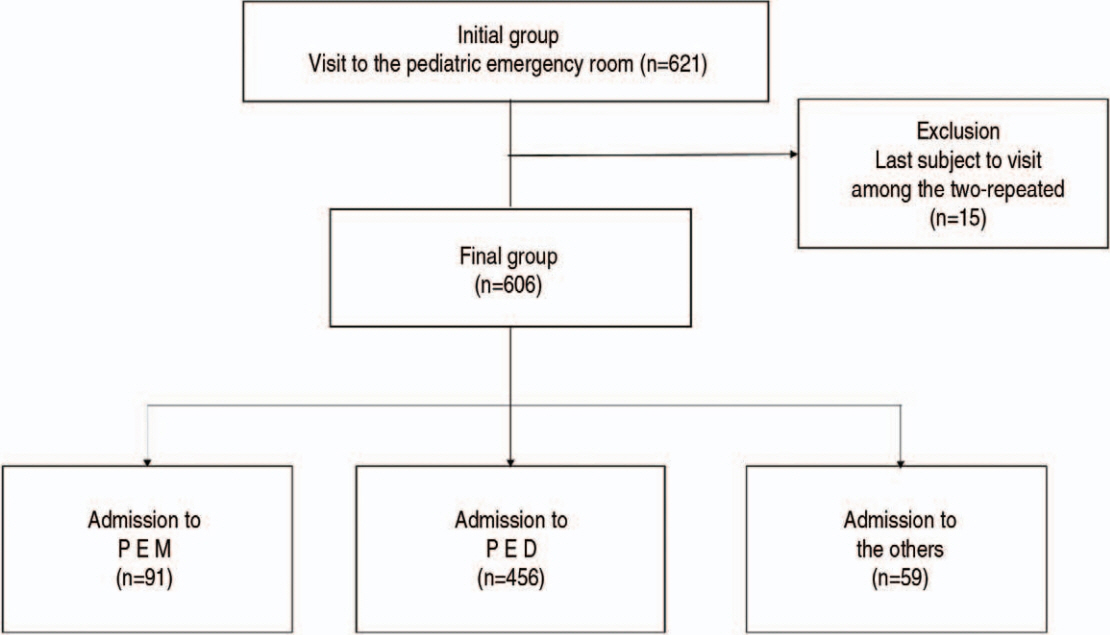
A chart review was completed for children (< 15 years) who were hospitalized to the PEW via the pediatric emergency center from March through May 2021. We compared the general characteristics and details regarding the outcomes depending on the departments they were hospitalized to, namely PEM, pediatrics (PED), and others.
Results
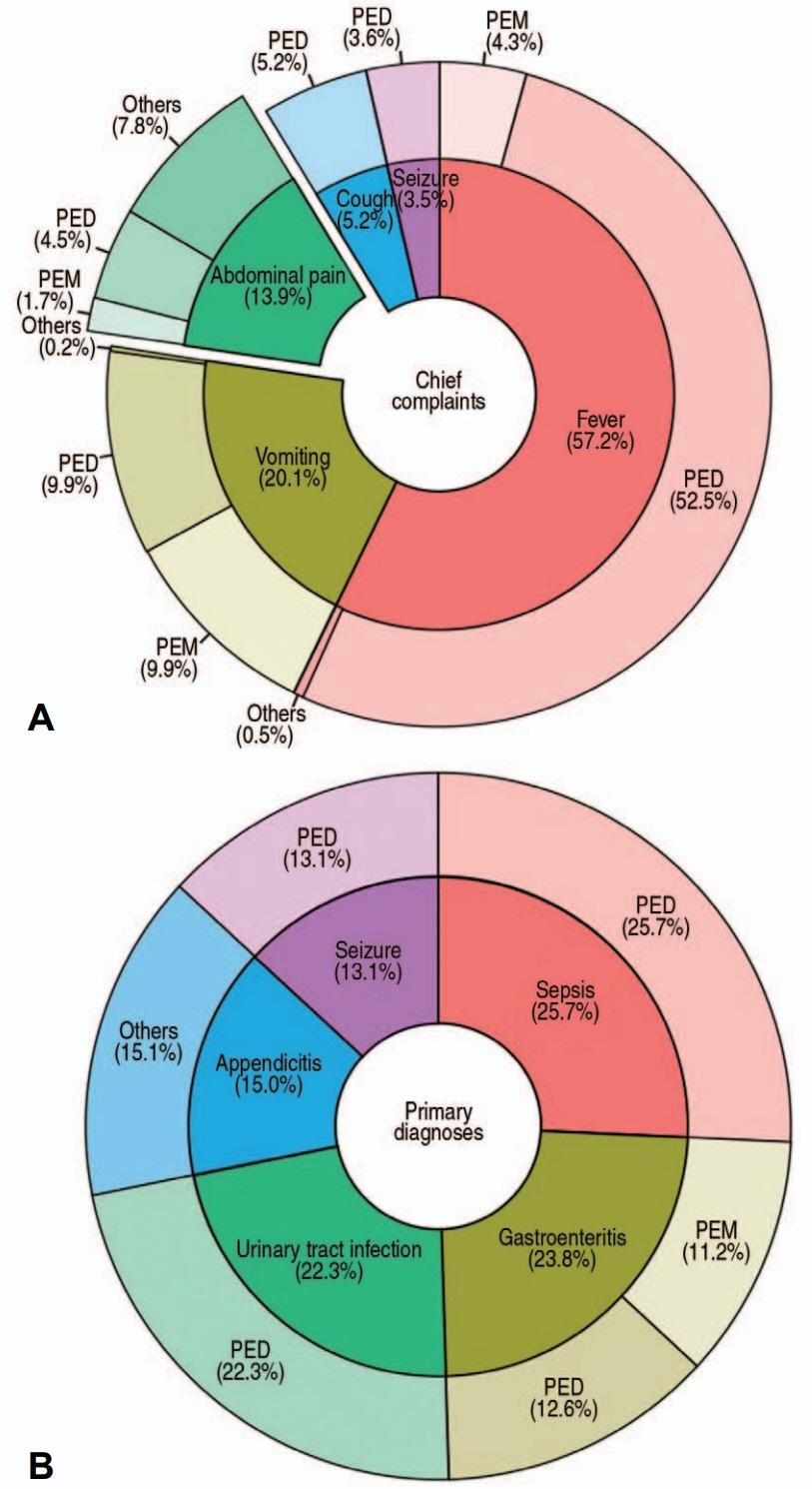
We analyzed a total of 606 hospitalized children: PEM, 91; PED, 456; and others, 59. In the order listed above, their median ages were 2 years (interquartile range, 1-6), 1 year (0-4), and 9 years (7-14) (P < 0.001). The numbers of children with Korean Triage and Acuity Scale of 1-3 were 71 (78.0%), 400 (87.7%), and 33 (55.9%) (P < 0.001). Median length of stay (LOS) in the emergency department (ED) and hospital tended to be shorter in PEM (ED LOS: PEM, 4.3 hours vs. PED and others, 4.0-6.3 hours; hospital LOS: PEM, 19.0 hours vs. PED and others, 58.5-63.8 hours; all Ps < 0.001). The differences in the LOS were prominent between others and PEM (ED LOS, 1.538 [95% confidence interval, 1.353-1.749]; hospital LOS, 3.375 [2.741-4.157]). Transfers to other departments occurred only in PEM (4.4%) and PED (3.9%) whereas intensive care was performed only in others (27.1%). Return visits showed no difference among the 3 departments. Top 5 chief complaints and primary diagnoses of the children hospitalized to PEM were vomiting, fever, abdominal pain, head injury, and poisoning, and gastroenteritis, concussion, syncope, poisoning, and upper respiratory infection, respectively.
Conclusion
Hospitalization to PEWs for short-term treatment or observation may relieve overcrowding in EDs or in hospitals, with comparable frequency of return visits.
Figure
Reference
-
References
1. Ministry of the Interior and Safety. Population statistics of Korea [Internet]. Ministry of the Interior and Safety; 2008-2023 [cited 2023 Mar 31]. Available from: https://jumin.mois.go.kr. Korean.2. Noh H. Prehospital transport of critically ill children via 119 emergency medical service providers: problems and improvement plan. Pediatr Emerg Med J. 2017; 4:34–7. Korean.3. Kim HM, Ha SO, Yang WS, Park YS, Kim JH. Effect of coronavirus disease 2019 pandemic on children’s visits to the emergency department. Pediatr Emerg Med J. 2022; 9:10–6.4. Song WM, Noh H, Ahn KO, Jeong SY, Suh J. Utilization of pediatric emergency medical center depending on visiting time. J Korean Soc Emerg Med. 2016; 27:182–8. Korean.5. Division of Emergency Healthcare, Ministry of Health and Welfare. Additional selection of 3 pediatric emergency centers for pediatric emergency patients [Internet]. Ministry of Health and Welfare; 2022 [cited 2022 Dec 17]. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=368190. Korean.6. Kim EY. Policy direction for the development of pediatric emergency care in Korea. Pediatr Emerg Med J. 2023; 10:1–2. Korean.7. Noh H, Kim DK, Lee JH, Kwak YH, Jung JH, Jang HY, et al. Comparisons of pediatric patients who visited to the pediatric emergency department and the general emergency department. Pediatr Emerg Med J. 2015; 2:29–34. Korean.8. Harper A, Jones P, Wimsett J, Stewart J, Le Fevre J, Wells S, et al. The effect of the shorter stays in emergency departments health target on the quality of ED discharge summaries. Emerg Med J. 2016; 33:860–4.9. McKenna P, Heslin SM, Viccellio P, Mallon WK, Hernandez C, Morley EJ. Emergency department and hospital crowding: causes, consequences, and cures. Clin Exp Emerg Med. 2019; 6:189–95.10. Shin S, Choi H, Choi B. Utilization characteristics of an advanced pediatric emergency center: a single center study over 2 years. Pediatr Emerg Med J. 2020; 7:16–22. Korean.11. Kim JY, Choi SH, Yoon YH, Cho YD, Park S. Characteristics of recurrent visit of emergency department by pediatric patients. Pediatr Emerg Med J. 2014; 1:24–8. Korean.12. Chai HS, Park GJ, Kim YM, Kim SC, Lee JH, Kim H, et al. Characteristics of frequent pediatric emergency department users at a tertiary university hospital. J Korean Soc Emerg Med. 2022; 33:421–8. Korean.13. van der Veen D, Remeijer C, Fogteloo AJ, Heringhaus C, de Groot B. Independent determinants of prolonged emergency department length of stay in a tertiary care centre: a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2018; 26:81.14. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008; 52:126–36.15. Gururaj VJ, Allen JE, Russo RM. Short stay in an outpatient department. An alternative to hospitalization. Am J Dis Child. 1972; 123:128–32.16. Macy ML, Kim CS, Sasson C, Lozon MM, Davis MM. Pediatric observation units in the United States: a systematic review. J Hosp Med. 2010; 5:172–82.17. Conners GP, Melzer SM; Committee on Hospital Care; Committee on Pediatric Emergency Medicine, Betts JM, Chitkara MB, et al. Pediatric observation units. Pediatrics. 2012; 130:172–9.18. Macy ML, Stanley RM, Lozon MM, Sasson C, Gebremariam A, Davis MM. Trends in highturnover stays among children hospitalized in the United States, 1993-2003. Pediatrics. 2009; 123:996–1002.19. Zebrack M, Kadish H, Nelson D. The pediatric hybrid observation unit: an analysis of 6477 consecutive patient encounters. Pediatrics. 2005; 115:e535–42.20. Gatto A, Rivetti S, Capossela L, Pata D, Covino M, Chiaretti A. Utility of a pediatric observation unit for the management of children admitted to the emergency department. Ital J Pediatr. 2021; 47:11.21. Ok M, Choi A, Kim MJ, Roh YH, Park I, Chung SP, et al. Emergency short-stay wards and boarding time in emergency departments: a propensity-score matching study. Am J Emerg Med. 2020; 38:2495–9.22. Moon S, Kim T, Park H, Kim H, Shin J, Park YS, et al. Effect of emergency physician-operated emergency short-stay ward on emergency department stay length and clinical outcomes: a case-control study. BMC Emerg Med. 2023; 23:47.23. Rentz AC, Kadish HA, Nelson DS. Physician satisfaction with a pediatric observation unit administered by pediatric emergency medicine physicians. Pediatr Emerg Care. 2004; 20:430–2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
- Utilization characteristics of an advanced pediatric emergency center: a single center study over 2 years
- National Patterns and Characteristics in Pediatric Dental Emergency Visits for Dental Conditions
- Impact of Maternal Uncertainty on Coping: Experiences from a General Hospital Pediatric Ward
- Correlation between the occurrence of acute gastroenteritis in children and regional temperature at a tertiary hospital emergency department in Korea