Clin Endosc.
2023 Sep;56(5):658-665. 10.5946/ce.2023.006.
Anesthesia care provider sedation versus conscious sedation for endoscopic ultrasound–guided tissue acquisition: a retrospective cohort study
- Affiliations
-
- 1Department of Medicine, Loma Linda University Medical Center, Loma Linda, CA, USA
- 2Division of Gastroenterology and Hepatology, Loma Linda University Medical Center, Loma Linda, CA, USA
- 3Division of Gastroenterology and Hepatology, Department of Medicine, Baylor College of Medicine, Houston, TX, USA
- KMID: 2546144
- DOI: http://doi.org/10.5946/ce.2023.006
Abstract
- Background/Aims
We aimed to study the effects of sedation on endoscopic ultrasound–guided tissue acquisition.
Methods
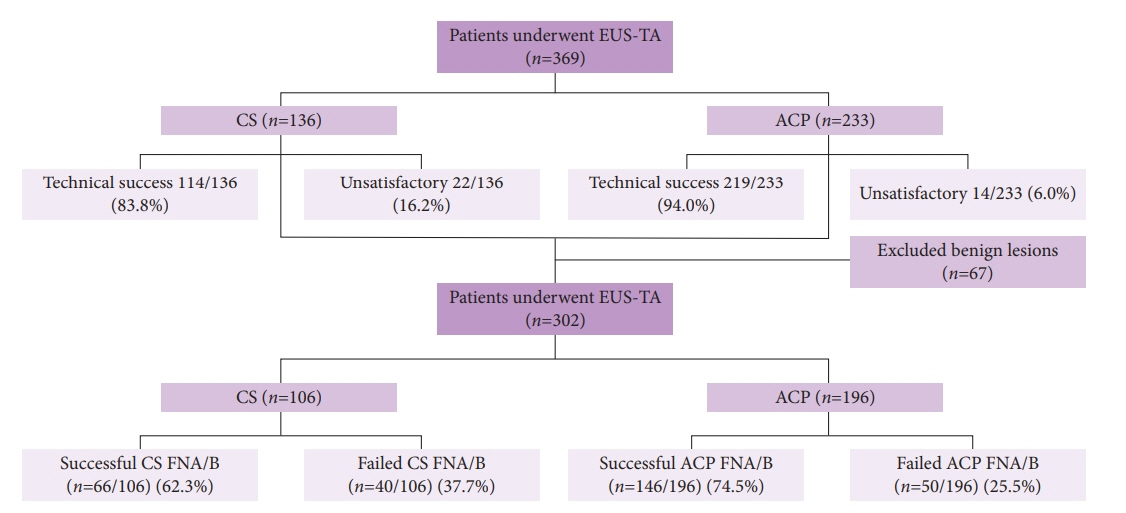
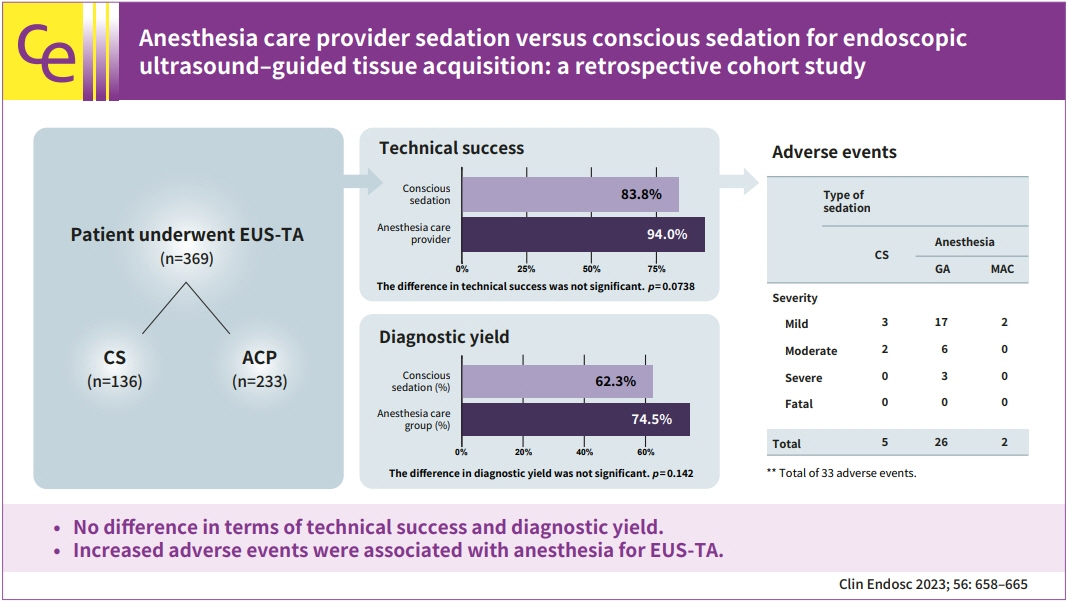
We conducted a retrospective study evaluating the role of sedation in endoscopic ultrasound–guided tissue acquisition by comparing two groups: anesthesia care provider (ACP) sedation and endoscopist-directed conscious sedation (CS).
Results
Technical success was achieved in 219/233 (94.0%) in the ACP group and 114/136 (83.8%) in the CS group (p=0.0086). In multivariate analysis, the difference in technical success between the two groups was not significant (adjusted odds ratio [aOR], 0.5; 95% confidence interval [CI], 0.234–1.069; p=0.0738). A successful diagnostic yield was present in 146/196 (74.5%) in the ACP group and 66/106 (62.3%) in the CS group, respectively (p=0.0274). In multivariate analysis, the difference in diagnostic yield between the two groups was not significant (aOR, 0.643; 95% CI, 0.356–1.159; p=0.142). A total of 33 adverse events (AEs) were observed. The incidence of AEs was significantly lower in the CS group (5/33 CS vs. 28/33 ACP; OR, 0.281; 95% CI, 0.095–0.833; p=0.022).
Conclusions
CS provided equivalent technical success and diagnostic yield for malignancy in endoscopic ultrasound–guided tissue acquisition. Increased AEs were associated with anesthesia for the endoscopic ultrasound–guided tissue acquisition.
Keyword
Figure
Reference
-
1. Wani S, Muthusamy VR, Komanduri S. EUS-guided tissue acquisition: an evidence-based approach (with videos). Gastrointest Endosc. 2014; 80:939–959.2. Chen G, Liu S, Zhao Y, et al. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer: a meta-analysis. Pancreatology. 2013; 13:298–304.3. Thornton GD, McPhail MJ, Nayagam S, et al. Endoscopic ultrasound guided fine needle aspiration for the diagnosis of pancreatic cystic neoplasms: a meta-analysis. Pancreatology. 2013; 13:48–57.4. Siddiqui AA, Brown LJ, Hong SK, et al. Relationship of pancreatic mass size and diagnostic yield of endoscopic ultrasound-guided fine needle aspiration. Dig Dis Sci. 2011; 56:3370–3375.5. Bang JY, Magee SH, Ramesh J, et al. Randomized trial comparing fanning with standard technique for endoscopic ultrasound-guided fine-needle aspiration of solid pancreatic mass lesions. Endoscopy. 2013; 45:445–450.6. Oppong KW, Bekkali NL, Leeds JS, et al. Fork-tip needle biopsy versus fine-needle aspiration in endoscopic ultrasound-guided sampling of solid pancreatic masses: a randomized crossover study. Endoscopy. 2020; 52:454–461.7. Di Leo M, Crinò SF, Bernardoni L, et al. EUS-guided core biopsies of pancreatic solid masses using a new fork-tip needle: a multicenter prospective study. Dig Liver Dis. 2019; 51:1275–1280.8. Madhoun MF, Wani SB, Rastogi A, et al. The diagnostic accuracy of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of solid pancreatic lesions: a meta-analysis. Endoscopy. 2013; 45:86–92.9. Iglesias-Garcia J, Dominguez-Munoz JE, Abdulkader I, et al. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of solid pancreatic masses. Am J Gastroenterol. 2011; 106:1705–1710.10. Ootaki C, Stevens T, Vargo J, et al. Does general anesthesia increase the diagnostic yield of endoscopic ultrasound-guided fine needle aspiration of pancreatic masses? Anesthesiology. 2012; 117:1044–1050.11. The Papanicolaou Society of Cytopathology Task Force on Standards of Practice. Guidelines of the Papanicolaou Society of Cytopathology for fine-needle aspiration procedure and reporting. Mod Pathol. 1997; 10:739–747.12. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE Workshop. Gastrointest Endosc. 2010; 71:446–454.13. Facciorusso A, Del Prete V, Buccino VR, et al. Diagnostic yield of Franseen and fork-tip biopsy needles for endoscopic ultrasound-guided tissue acquisition: a meta-analysis. Endosc Int Open. 2019; 7:E1221–E1230.14. Wani S, Muthusamy VR, McGrath CM, et al. AGA white paper: optimizing endoscopic ultrasound-guided tissue acquisition and future directions. Clin Gastroenterol Hepatol. 2018; 16:318–327.15. Mohamadnejad M, Mullady D, Early DS, et al. Increasing number of passes beyond 4 does not increase sensitivity of detection of pancreatic malignancy by endoscopic ultrasound-guided fine-needle aspiration. Clin Gastroenterol Hepatol. 2017; 15:1071–1078.16. Chung MJ, Park SW, Kim SH, et al. Clinical and technical guideline for endoscopic ultrasound (EUS)-guided tissue acquisition of pancreatic solid tumor: Korean Society of Gastrointestinal Endoscopy (KSGE). Clin Endosc. 2021; 54:161–181.17. Vargo JJ, Niklewski PJ, Williams JL, et al. Patient safety during sedation by anesthesia professionals during routine upper endoscopy and colonoscopy: an analysis of 1.38 million procedures. Gastrointest Endosc. 2017; 85:101–108.18. Smith ZL, Mullady DK, Lang GD, et al. A randomized controlled trial evaluating general endotracheal anesthesia versus monitored anesthesia care and the incidence of sedation-related adverse events during ERCP in high-risk patients. Gastrointest Endosc. 2019; 89:855–862.19. Park HJ, Kim BW, Lee JK, et al. 2021 Korean Society of Gastrointestinal Endoscopy clinical practice guidelines for endoscopic sedation. Clin Endosc. 2022; 55:167–182.20. Allen ML. Safety of deep sedation in the endoscopy suite. Curr Opin Anaesthesiol. 2017; 30:501–506.21. Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol. 2006; 101:967–974.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation for routine gastrointestinal endoscopic procedures: a review on efficacy, safety, efficiency, cost and satisfaction
- Anesthesia and Sedation
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)
- Current trends in intravenous sedative drugs for dental procedures
- Application of sevoflurane inhalation sedation in dental treatment: a mini review