Clin Endosc.
2023 Sep;56(5):604-612. 10.5946/ce.2022.163.
Usefulness of a new polyvinyl alcohol hydrogel (PVA-H)-based simulator for endoscopic submucosal dissection training: a pilot study
- Affiliations
-
- 1Department of Gastroenterology, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 2Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Gastroenterology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Gastroenterology, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2546139
- DOI: http://doi.org/10.5946/ce.2022.163
Abstract
- Background/Aims
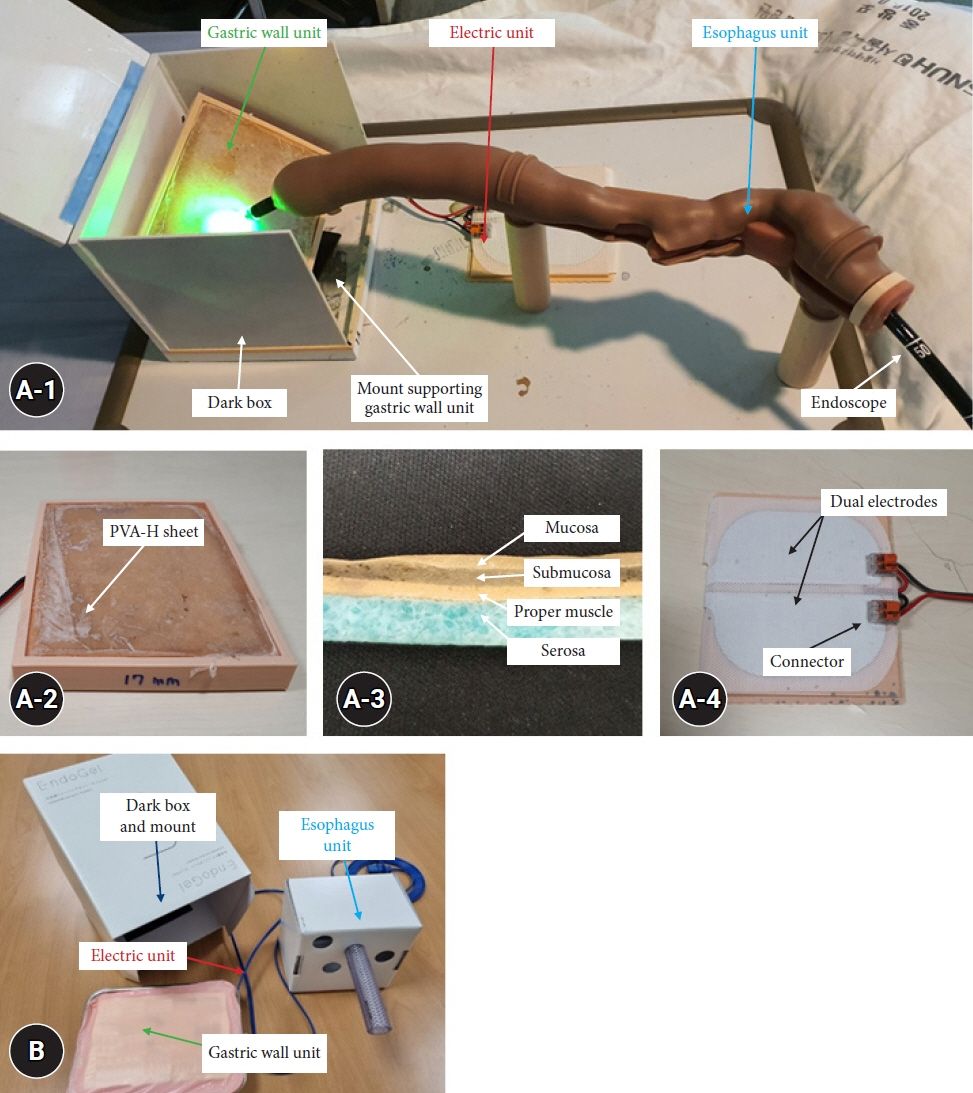
We developed a new endoscopic submucosal dissection (ESD) simulator and evaluated its efficacy and realism for use training endoscopists.
Methods
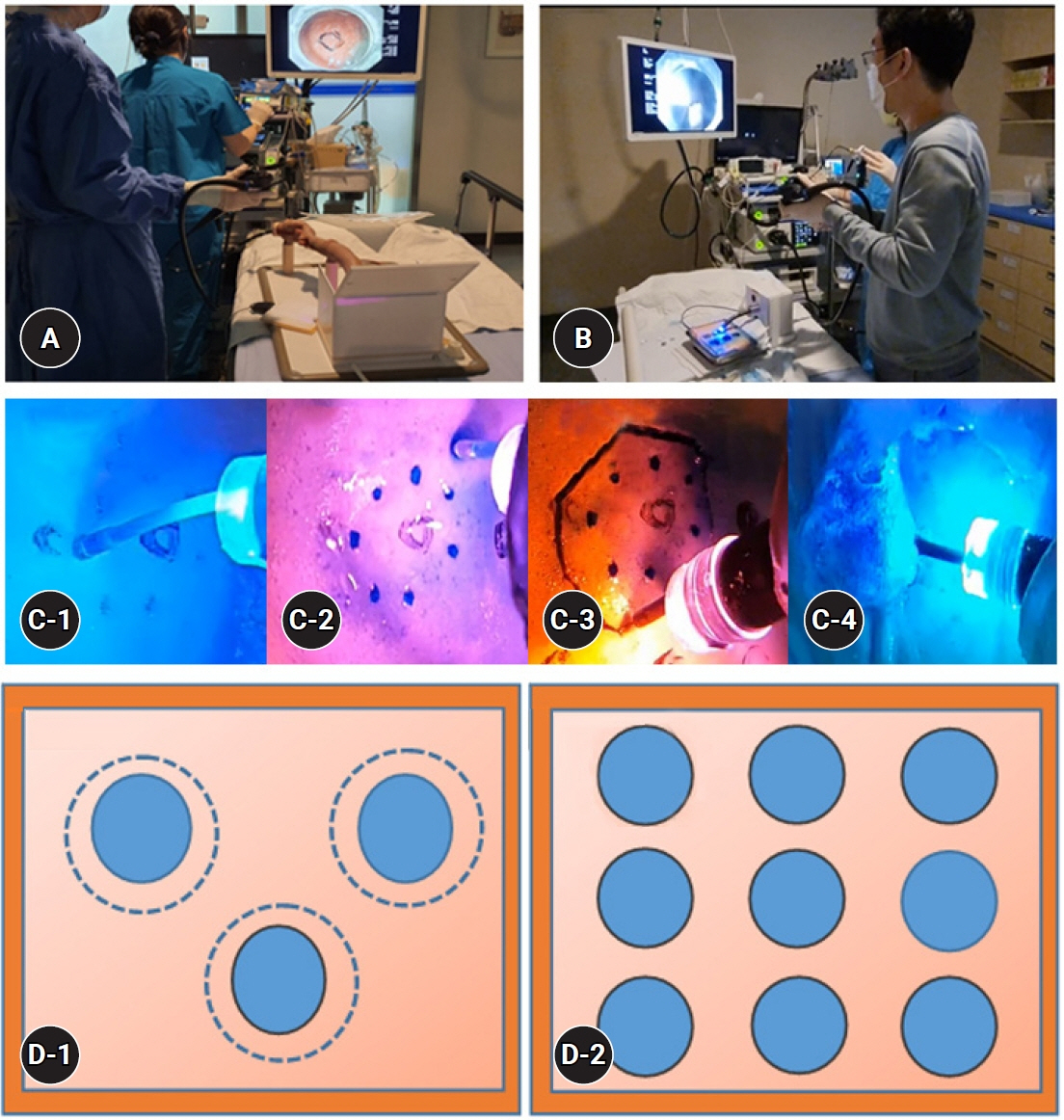
An ESD simulator was constructed using polyvinyl alcohol hydrogel sheets and compared to a previous ESD simulator. Between March 1, 2020, and December 30, 2021, eight expert endoscopists from three different centers analyzed the procedure-related factors of the simulator. Five trainees performed gastric ESD exercises under the guidance of these experts.
Results
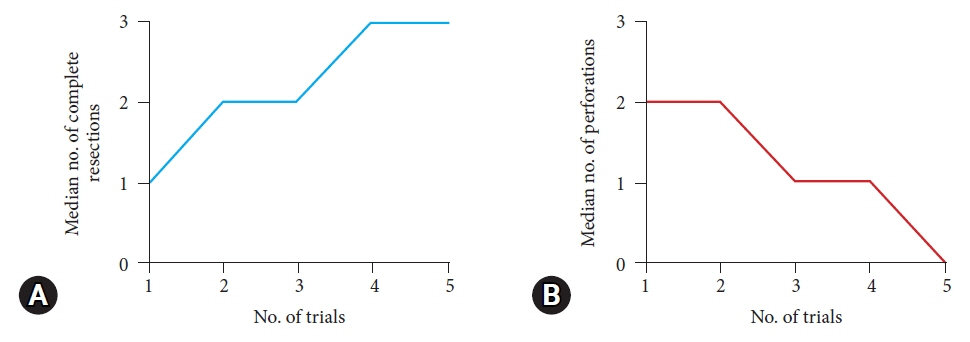
Although the two ESD simulators provided overall favorable outcomes in terms of ESD-related factors, the new simulator had several benefits, including better marking of the target lesion’s limits (p<0.001) and overall handling (p<0.001). Trainees tested the usefulness of the new ESD simulator. The complete resection rate improved after 3 ESD training sessions (9 procedures), and the perforation rate decreased after 4 sessions (12 procedures).
Conclusions
We have developed a new ESD simulator that can help beginners achieve a high level of technical experience before performing real-time ESD procedures in patients.
Keyword
Figure
Reference
-
1. Kang KJ, Kim KM, Min BH, et al. Endoscopic submucosal dissection of early gastric cancer. Gut Liver. 2011; 5:418–426.2. Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006; 41:929–942.3. Ohkura Y, Iizuka T, Kikuchi D, et al. Endoscopic submucosal dissection for early esophageal cancer associated with achalasia. Turk J Gastroenterol. 2013; 24:161–166.4. Holmstrom AL, Aadam AA, Hungness ES. Submucosal endoscopy. Tech Gastrointest Endosc. 2018; 20:211–217.5. Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007; 39:761–764.6. Odagiri H, Yasunaga H. Complications following endoscopic submucosal dissection for gastric, esophageal, and colorectal cancer: a review of studies based on nationwide large-scale databases. Ann Transl Med. 2017; 5:189.7. Toyokawa T, Inaba T, Omote S, et al. Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: analysis of 1123 lesions. J Gastroenterol Hepatol. 2012; 27:907–912.8. Lee EJ, Lee JB, Choi YS, et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc. 2012; 26:1587–1594.9. Toyonaga T, Man-i M, Fujita T, et al. Retrospective study of technical aspects and complications of endoscopic submucosal dissection for laterally spreading tumors of the colorectum. Endoscopy. 2010; 42:714–722.10. Mizuno K, Sato H, Hashimoto S, et al. A novel training model composed of nonbiological materials for endoscopic submucosal dissection. Gastrointest Endosc. 2016; 84:373–374.11. Ohata K, Nonaka K, Misumi Y, et al. Usefulness of training using animal models for colorectal endoscopic submucosal dissection: is experience performing gastric ESD really needed? Endosc Int Open. 2016; 4:E333–E339.12. Chen MJ, Wang HY, Chang CW, et al. A novel artificial tissue simulator for endoscopic submucosal resection training: a pilot study. BMC Gastroenterol. 2016; 16:112.13. Sato H, Mizuno KI, Sato Y, et al. Development and use of a non-biomaterial model for hands-on training of endoscopic procedures. Ann Transl Med. 2017; 5:182.14. Smooth-On Inc. Product brochure [Internet]. Macungie: Smooth-On Inc. [cited 2020 Dec 30]. Available from: https://www.smooth-on.com/products/ecoflex-00-30/.15. Parra-Blanco A, Gonzalez N, Arnau MR. Ex vivo and in vivo models for endoscopic submucosal dissection training. Clin Endosc. 2012; 45:350–357.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Box Simulator Is Useful for Training Novice Endoscopists in Basic Endoscopic Techniques
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Usefulness of Narrow-Band Imaging in Endoscopic Submucosal Dissection of the Stomach
- Prediction of Simulator Sickness in Virtual Environments
- Simulator-based training method in gastrointestinal endoscopy training and currently available simulators