J Korean Assoc Oral Maxillofac Surg.
2023 Aug;49(4):184-191. 10.5125/jkaoms.2023.49.4.184.
Surgical removal of third molars in a young adult: review of indications and surgical techniques
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University, Bangkok, Thailand
- KMID: 2545583
- DOI: http://doi.org/10.5125/jkaoms.2023.49.4.184
Abstract
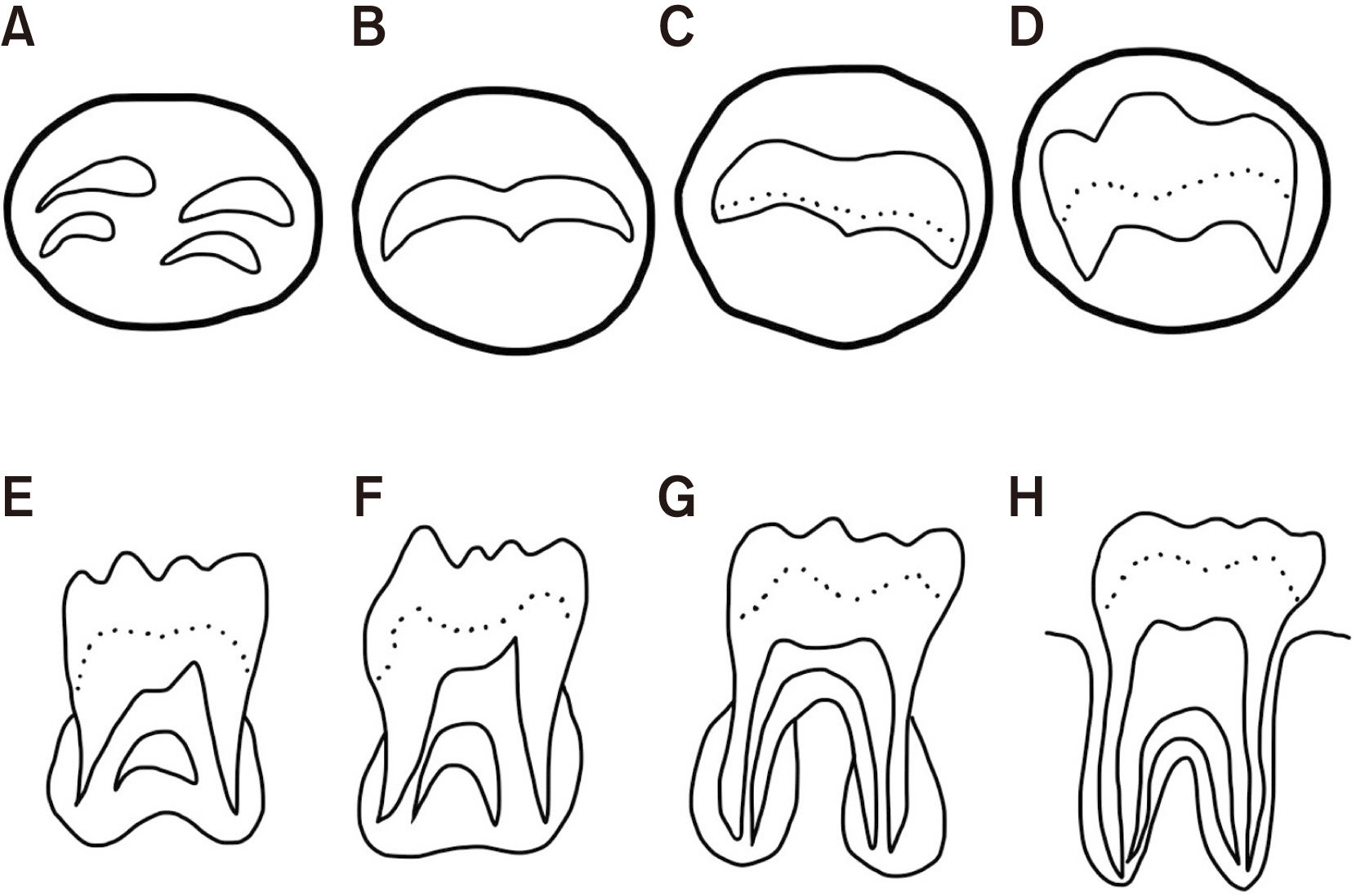
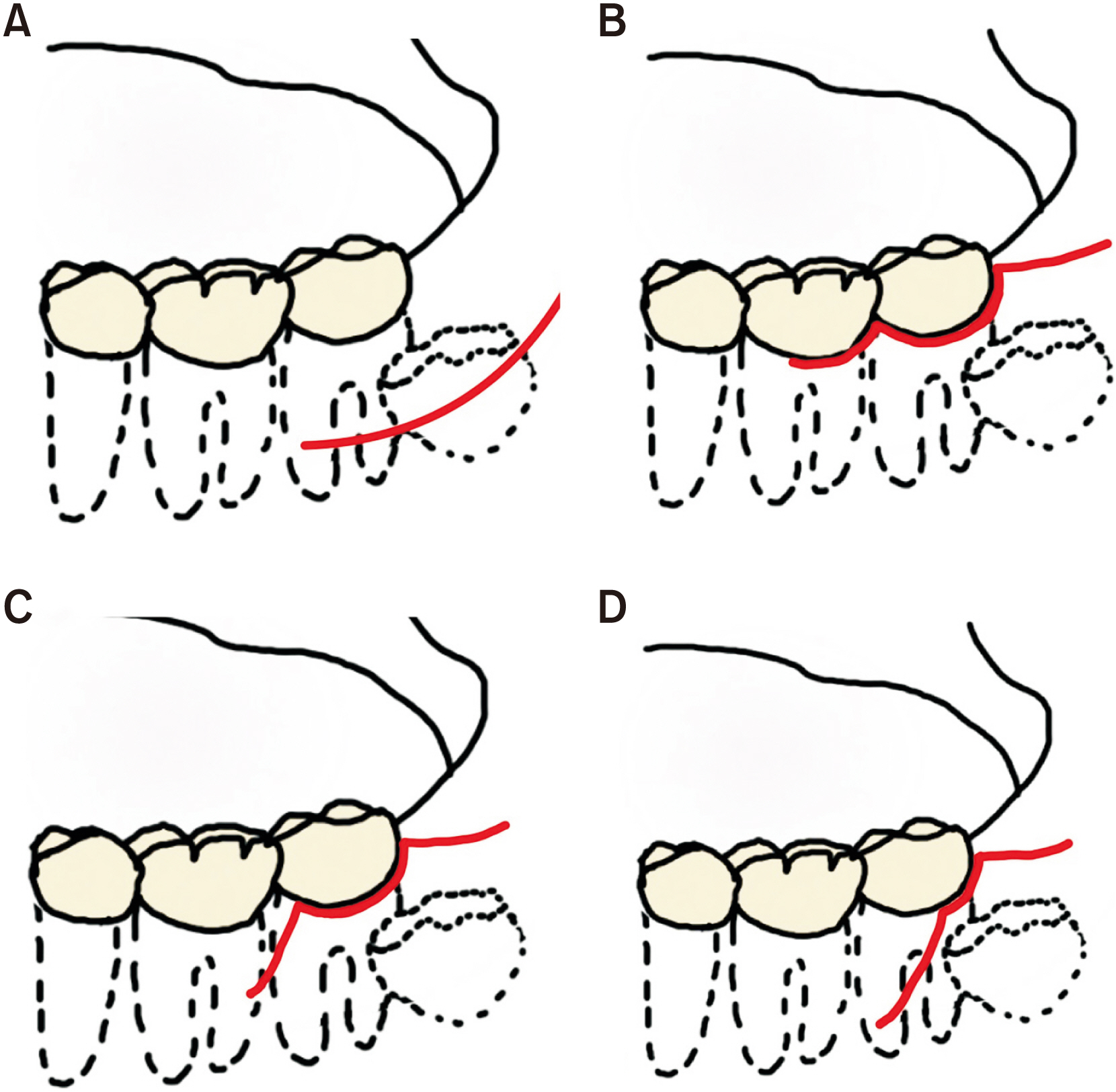
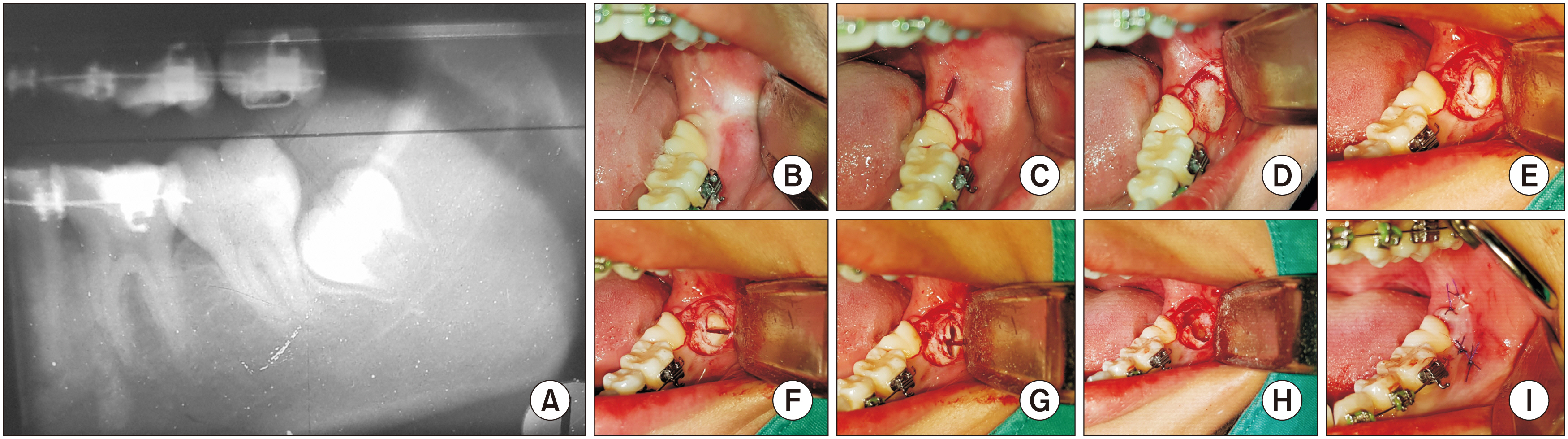
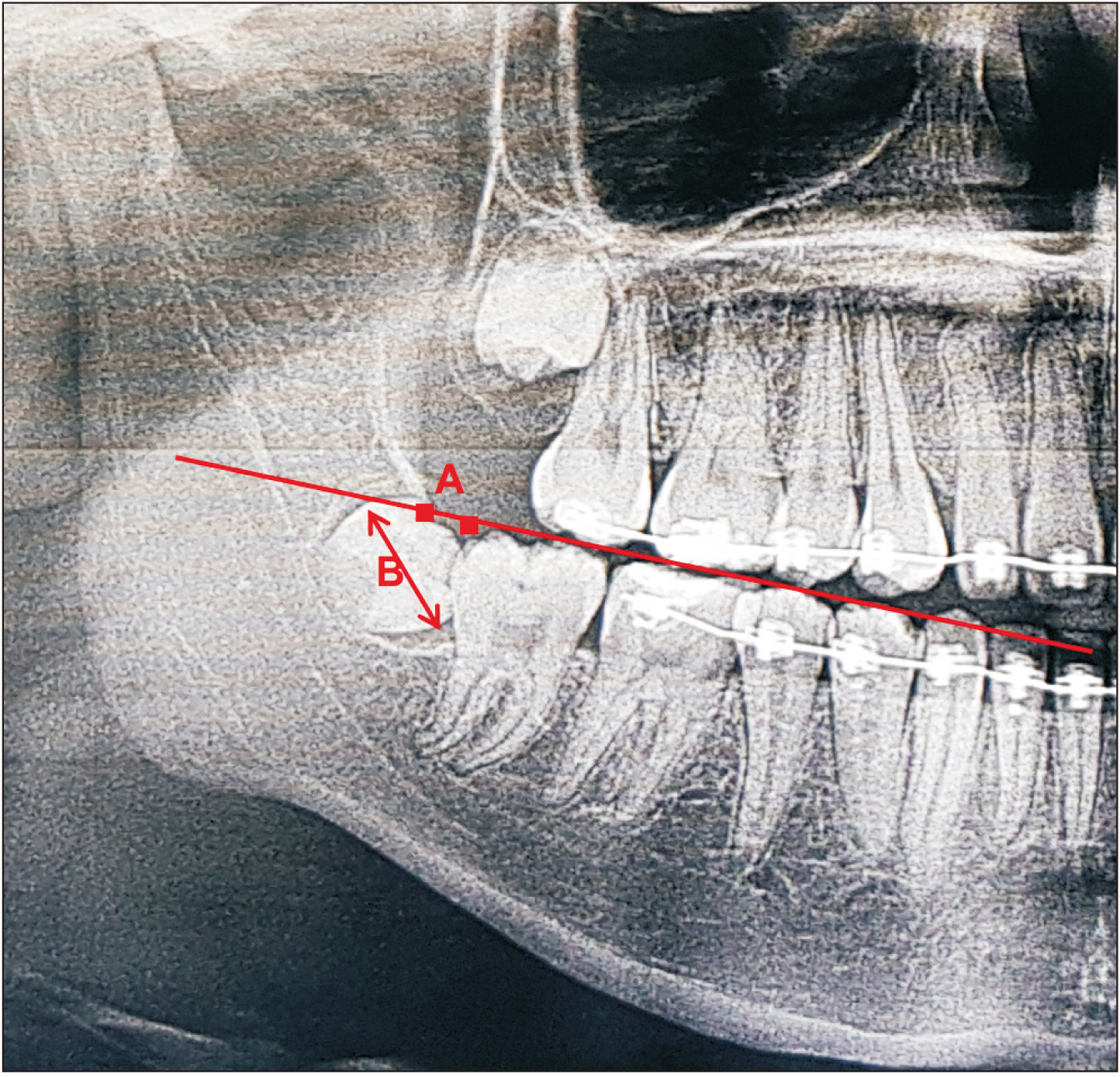
- Germectomy is a surgical method most typically performed in young adults. The indications for treatment are controversial. The purpose of this review was to determine the correct indications for germectomy and to discuss the advantages and disadvantages of the procedure. We reviewed the surgical techniques (anesthetic methods, patient preparation, and flap designs) and complications. Germectomy for orthodontic purposes is a common indication for surgical removal of tooth germ among young patients. Several studies have supported removal at an earlier age to produce fewer surgical complications. Several surgical techniques have been described in the literature.
Keyword
Figure
Reference
-
References
1. Eklund SA, Pittman JL. 2001; Third-molar removal patterns in an insured population. J Am Dent Assoc. 132:469–75. https://doi.org/10.14219/jada.archive.2001.0209. DOI: 10.14219/jada.archive.2001.0209. PMID: 11315377.2. Cunha-Cruz J, Rothen M, Spiekerman C, Drangsholt M, McClellan L. Huang GJ; Northwest Practice-Based Research Collaborative in Evidence-Based Dentistry. 2014; Recommendations for third molar removal: a practice-based cohort study. Am J Public Health. 104:735–43. https://doi.org/10.2105/ajph.2013.301652. DOI: 10.2105/AJPH.2013.301652. PMID: 24524519. PMCID: PMC4025689.3. Knutsson K, Brehmer B, Lysell L, Rohlin M. 1992; General dental practitioners' evaluation of the need for extraction of asymptomatic mandibular third molars. Community Dent Oral Epidemiol. 20:347–50. DOI: 10.1111/j.1600-0528.1992.tb00696.x. PMID: 1343819.4. Massler M, Schour I, Poncher HG. 1941; Developmental pattern of the child as reflected in the calcification pattern of the teeth. Am J Dis Child. 62:33–67. https://doi.org/10.1001/archpedi.1941.02000130042004. DOI: 10.1001/archpedi.1941.02000130042004.
Article5. Chiapasco M, Crescentini M, Romanoni G. 1995; Germectomy or delayed removal of mandibular impacted third molars: the relationship between age and incidence of complications. J Oral Maxillofac Surg. 53:418–22. discussion 422–3. https://doi.org/10.1016/0278-2391(95)90715-7. DOI: 10.1016/0278-2391(95)90715-7. PMID: 7699496.
Article6. Finne K, Klämfeldt A. 1981; Removal of lower third molar germs by lateral trepanation and conventional technique. A comparative study. Int J Oral Surg. 10:251–4. https://doi.org/10.1016/s0300-9785(81)80067-1. DOI: 10.1016/S0300-9785(81)80067-1. PMID: 6809654.
Article7. Pogrel MA, Dodson TB, Swift JQ, Bonine FL, Rafetto LK, Kennedy JE, et al. 2007; White paper on third molar data. American Association of Oral and Maxillofacial Surgeons.8. Sivolella S, Berengo M, Bressan E, Di Fiore A, Stellini E. 2011; Osteotomy for lower third molar germectomy: randomized prospective crossover clinical study comparing piezosurgery and conventional rotatory osteotomy. J Oral Maxillofac Surg. 69:e15–23. https://doi.org/10.1016/j.joms.2010.12.036. DOI: 10.1016/j.joms.2010.12.036. PMID: 21419542.9. Ling XF, Heng TL, Mohamad AF. 2017; Which procedure is better: germectomy or surgical removal of mandibular third molar? Int J Oral Maxillofac Surg. 46 Suppl 1(Suppl 1):110–1. https://doi.org/10.1016/j.ijom.2017.02.390. DOI: 10.1016/j.ijom.2017.02.390.
Article10. Haddad J. 2020. Management of third molars. Dental Economics. https://dentalacademyofce.com/courses/management-of-third-molars.11. Chossegros C, Guyot L, Cheynet F, Belloni D, Blanc JL. 2002; Is lingual nerve protection necessary for lower third molar germectomy? A prospective study of 300 procedures. Int J Oral Maxillofac Surg. 31:620–4. https://doi.org/10.1054/ijom.2002.0236. DOI: 10.1054/ijom.2002.0236. PMID: 12521318.
Article12. Monaco G, Daprile G, Tavernese L, Corinaldesi G, Marchetti C. 2009; Mandibular third molar removal in young patients: an evaluation of 2 different flap designs. J Oral Maxillofac Surg. 67:15–21. https://doi.org/10.1016/j.joms.2007.05.032. DOI: 10.1016/j.joms.2007.05.032. PMID: 19070743.
Article13. Mazur M, Ndokaj A, Marasca B, Sfasciotti GL, Marasca R, Bossù M, et al. 2022; Clinical indications to germectomy in pediatric dentistry: a systematic review. Int J Environ Res Public Health. 19:740. https://doi.org/10.3390/ijerph19020740. DOI: 10.3390/ijerph19020740. PMID: 35055565. PMCID: PMC8775662.
Article14. Monaco G, Tavernese L, Agostini R, Marchetti C. 2009; Evaluation of antibiotic prophylaxis in reducing postoperative infection after mandibular third molar extraction in young patients. J Oral Maxillofac Surg. 67:1467–72. https://doi.org/10.1016/j.joms.2008.12.066. DOI: 10.1016/j.joms.2008.12.066. PMID: 19531419.
Article15. Demirjian A, Goldstein H, Tanner JM. 1973; A new system of dental age assessment. Hum Biol. 45:211–27. PMID: 4714564.16. Melo M, Ata-Ali F, Ata-Ali J, Martinez Gonzalez JM, Cobo T. 2022; Demirjian and Cameriere methods for age estimation in a Spanish sample of 1386 living subjects. Sci Rep. 12:2838. https://doi.org/10.1038/s41598-022-06917-x. DOI: 10.1038/s41598-022-06917-x. PMID: 35181746. PMCID: PMC8857188.
Article17. Bjørnland T, Haanaes HR, Lind PO, Zachrisson B. 1987; Removal of third molar germs. Study of complications. Int J Oral Maxillofac Surg. 16:385–90. https://doi.org/10.1016/s0901-5027(87)80072-3. DOI: 10.1016/S0901-5027(87)80072-3. PMID: 3117908.
Article18. Bartuli FN, Piva P, Savo A, Di Dio M, Luciani F, Arcuri C. 2014; Lower third molar germectomy: the flap recovery on the lower second molar. A clinical study. Int J Clin Dent. 7:289–94.19. Zhang QB, Zhang ZQ. 2012; Early extraction: a silver bullet to avoid nerve injury in lower third molar removal? Int J Oral Maxillofac Surg. 41:1280–3. https://doi.org/10.1016/j.ijom.2012.03.030. DOI: 10.1016/j.ijom.2012.03.030. PMID: 22608199.
Article20. Laskin DM. 1971; Evaluation of the third molar problem. J Am Dent Assoc. 82:824–8. https://doi.org/10.14219/jada.archive.1971.0130. DOI: 10.14219/jada.archive.1971.0130. PMID: 5278781.
Article21. Richardson ME. 1989; The role of the third molar in the cause of late lower arch crowding: a review. Am J Orthod Dentofacial Orthop. 95:79–83. https://doi.org/10.1016/0889-5406(89)90139-x. DOI: 10.1016/0889-5406(89)90139-X. PMID: 2642642.
Article22. Staderini E, Patini R, Guglielmi F, Camodeca A, Gallenzi P. 2019; How to manage impacted third molars: germectomy or delayed removal? A systematic literature review. Medicina (Kaunas). 55:79. https://doi.org/10.3390/medicina55030079. DOI: 10.3390/medicina55030079. PMID: 30917605. PMCID: PMC6473914.
Article23. Sverzut CE, Trivellato AE, Sverzut AT, de Matos FP, Kato RB. 2009; Removal of a maxillary third molar accidentally displaced into the infratemporal fossa via intraoral approach under local anesthesia: report of a case. J Oral Maxillofac Surg. 67:1316–20. https://doi.org/10.1016/j.joms.2008.09.018. DOI: 10.1016/j.joms.2008.09.018. PMID: 19446223.
Article24. Primo BT, Stringhini DJ, da Costa DJ, Rebellato NLB, Scariot R. 2016; Delayed removal of maxillary third molar displaced into the maxillary sinus. Stomatologija. 18:128–32. PMID: 28980543.25. Roshanghias K, Peisker A, Zieron JO. 2016; Maxillary tooth displacement in the infratemporal fossa. Dent Res J (Isfahan). 13:373–5. https://doi.org/10.4103/1735-3327.187881. DOI: 10.4103/1735-3327.187881. PMID: 27605997. PMCID: PMC4993067.
Article26. Nogueira EFC, Almeida RAC, Catunda IS, Vasconcelos BCDE, Leite Segundo AV. 2019; Impacted maxillary third molar displaced to the infratemporal space: a critical review and case report. Gen Dent. 67:16–20. PMID: 30644825.27. Dodson TB. 2017; The trouble with exact change. J Oral Maxillofac Surg. 75:445–6. https://doi.org/10.1016/j.joms.2016.12.033. DOI: 10.1016/j.joms.2016.12.033. PMID: 28235455.
Article28. Lee YJ, Kook YA, Park JH, Park J, Bayome M, Vaid NR, et al. 2019; Short-term cone-beam computed tomography evaluation of maxillary third molar changes after total arch distalization in adolescents. Am J Orthod Dentofacial Orthop. 155:191–7. https://doi.org/10.1016/j.ajodo.2018.04.023. DOI: 10.1016/j.ajodo.2018.04.023. PMID: 30712690.
Article29. Flores-Mir C, McGrath L, Heo G, Major PW. 2013; Efficiency of molar distalization associated with second and third molar eruption stage. Angle Orthod. 83:735–42. https://doi.org/10.2319/081612-658.1. DOI: 10.2319/081612-658.1. PMID: 23167519. PMCID: PMC8754030.
Article30. Chaparro-Avendaño AV, Pérez-García S, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. 2005; Morbidity of third molar extraction in patients between 12 and 18 years of age. Med Oral Patol Oral Cir Bucal. 10:422–31. PMID: 16264374.31. Harradine NW, Pearson MH, Toth B. 1998; The effect of extraction of third molars on late lower incisor crowding: a randomized controlled trial. Br J Orthod. 25:117–22. https://doi.org/10.1093/ortho/25.2.117. DOI: 10.1093/ortho/25.2.117. PMID: 9668994.
Article32. Cassetta M, Altieri F. 2017; The influence of mandibular third molar germectomy on the treatment time of impacted mandibular second molars using brass wire: a prospective clinical pilot study. Int J Oral Maxillofac Surg. 46:905–11. https://doi.org/10.1016/j.ijom.2017.03.027. DOI: 10.1016/j.ijom.2017.03.027. PMID: 28408148.
Article33. Bisconte P, Matarrese L, Del Rosso E, Farronato . 2017; Germectomy of third molars in orthodontic therapy: usefulness of volumetric analysis with TC cone beam. Austin J Radiol. 4:1072. https://doi.org/10.26420/austinjradiol.2018.1072. DOI: 10.26420/austinjradiol.2018.1072.
Article34. Monaco G, Cecchini S, Gatto MR, Pelliccioni GA. 2017; Delayed onset infections after lower third molar germectomy could be related to the space distal to the second molar. Int J Oral Maxillofac Surg. 46:373–8. https://doi.org/10.1016/j.ijom.2016.09.011. DOI: 10.1016/j.ijom.2016.09.011. PMID: 27746008.
Article35. Maria A, Malik M, Virang P. 2012; Comparison of primary and secondary closure of the surgical wound after removal of impacted mandibular third molars. J Maxillofac Oral Surg. 11:276–83. https://doi.org/10.1007/s12663-011-0287-9. DOI: 10.1007/s12663-011-0287-9. PMID: 23997477. PMCID: PMC3428443.
Article36. Chaudhary M, Singh M, Singh S, Singh SP, Kaur G. 2012; Primary and secondary closure technique following removal of impacted mandibular third molars: a comparative study. Natl J Maxillofac Surg. 3:10–4. https://doi.org/10.4103/0975-5950.102141. DOI: 10.4103/0975-5950.102141. PMID: 23251051. PMCID: PMC3513800.
Article37. Cardarelli A, Pecora CN, Arun KG. 2020; Early third molar extraction: when germectomy is the best choise. IPDOAJ. 4:350–3. https://doi.org/10.32474/IPDOAJ.2020.04.000192. DOI: 10.32474/IPDOAJ.2020.04.000192.
Article38. Nolla CM. 1960; The development of the permanent teeth. J Dent Child. 27:254–66.39. Øyri H, Jensen JL, Barkvoll P, Jonsdottir OH, Reseland J, Bjørnland T. 2021; Incidence of alveolar osteitis after mandibular third molar surgery. Can inflammatory cytokines be identified locally? Acta Odontol Scand. 79:205–11. https://doi.org/10.1080/00016357.2020.1817546. DOI: 10.1080/00016357.2020.1817546. PMID: 32898447.
Article40. Kaposvári I, Körmöczi K, Csurgay K, Horváth F, Ashourioun AH, Buglyó A, et al. 2021; Delayed-onset infections after lower third molar surgery: a Hungarian case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol. 132:641–7. https://doi.org/10.1016/j.oooo.2021.04.052. DOI: 10.1016/j.oooo.2021.04.052. PMID: 34518142.
Article41. Ganss C, Hochban W, Kielbassa AM, Umstadt HE. 1993; Prognosis of third molar eruption. Oral Surg Oral Med Oral Pathol. 76:688–93. https://doi.org/10.1016/0030-4220(93)90035-3. DOI: 10.1016/0030-4220(93)90035-3. PMID: 8284071.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Superciliary Keyhole Approach for Unruptured Anterior Circulation Aneurysms: Surgical Technique, Indications, and Contraindications
- Recent Updates on Minimally Invasive Spine Surgery: Techniques, Technologies, and Indications
- Completion Thyroidectomy
- Third molar changes following lower second molar extractions
- Current concepts in genioplasty: surgical techniques, indications, and future perspectives