Arch Hand Microsurg.
2023 Sep;28(3):188-193. 10.12790/ahm.23.0020.
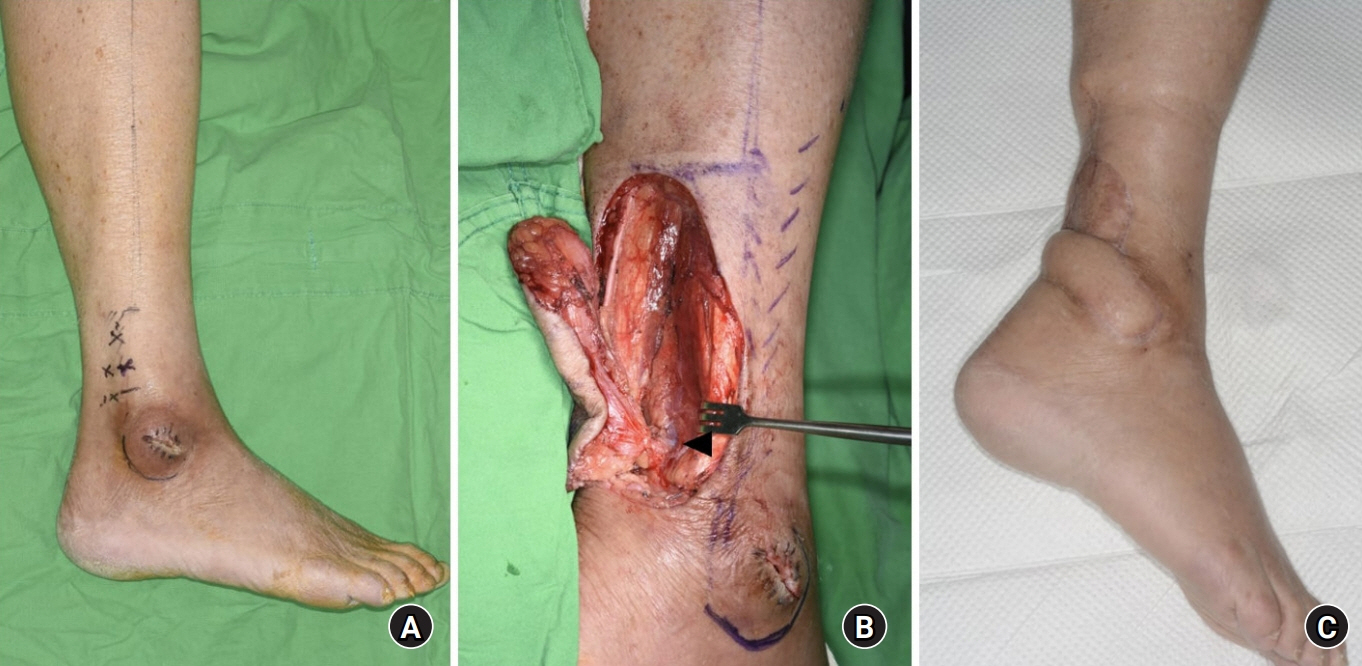
The outcomes of peroneal artery perforator-based propeller flaps for the treatment of infected lateral malleolar bursitis
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Plastic and Reconstructive Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- KMID: 2545529
- DOI: http://doi.org/10.12790/ahm.23.0020
Abstract
- Purpose
Infected malleolar bursitis sometimes requires multiple debridements, followed by soft tissue reconstruction with a flap. The purpose of this study was to evaluate the clinical outcomes of patients with infected lateral malleolar bursitis who were treated using peroneal artery perforator-based propeller flaps.
Methods
We retrospectively included 10 patients who underwent reconstruction of the lateral malleolus with a peroneal artery perforator-based propeller flap due to infected lateral malleolar bursitis between 2014 and 2022.
Results
The average follow-up time was 77.2 weeks. Six patients experienced complete healing; three developed partial flap necrosis, and one had a long-lasting seroma. All patients with complications had long-term diabetes.
Conclusion
Partial flap necrosis in patients with diabetes may occur because of impaired microcirculation. A peroneal artery perforator-based propeller flap could be useful for soft tissue reconstruction in select patients without diabetes or in patients with diabetes who have infected lateral malleolar bursitis.
Keyword
Figure
Reference
-
References
1. Park CH, Park JJ, Woo IH, Yan H, Lee WC. Characteristics of synovial fistula of the ankle joint: a case series. J Clin Med. 2022; 11:6215.
Article2. Kim KJ, Ahn JT, Yoon KT, Lee JH. A comparison of fasciocutaneous and adipofascial methods in the reverse sural artery flap for treatment of diabetic infected lateral malleolar bursitis. J Orthop Surg (Hong Kong). 2019; 27:2309499019828546.
Article3. Parrett BM, Pribaz JJ, Matros E, Przylecki W, Sampson CE, Orgill DP. Risk analysis for the reverse sural fasciocutaneous flap in distal leg reconstruction. Plast Reconstr Surg. 2009; 123:1499–504.
Article4. Bamba R, Loewenstein SN, Adkinson JM. Donor site morbidity after sural nerve grafting: a systematic review. J Plast Reconstr Aesthet Surg. 2021; 74:3055–60.
Article5. Hashimoto I, Yoshinaga R, Toda M, Nakanishi H. Intractable malleolar bursitis treated with lateral calcaneal artery adipofascial flap. Br J Plast Surg. 2003; 56:701–3.
Article6. Barnett CH, Napier JR. The axis of rotation at the ankle joint in man: its influence upon the form of the talus and the mobility of the fibula. J Anat. 1952; 86:1–9.7. Pignatti M, Ogawa R, Hallock GG, et al. The "Tokyo" consensus on propeller flaps. Plast Reconstr Surg. 2011; 127:716–22.
Article8. Mojallal A, Wong C, Shipkov C, et al. Vascular supply of the distally based superficial sural artery flap: surgical safe zones based on component analysis using three-dimensional computed tomographic angiography. Plast Reconstr Surg. 2010; 126:1240–52.
Article9. Kim K, Kim J, Jeong W, Jo T, Park SW, Choi J. Outcome of distal lower leg reconstruction with the propeller perforator flap in diabetic patients. J Plast Surg Hand Surg. 2021; 55:242–8.
Article10. Hong JP. The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009; 123:230–5.
Article11. Brown TD, Varney TE, Micheli LJ. Malleolar bursitis in figure skaters. Indications for operative and nonoperative treatment. Am J Sports Med. 2000; 28:109–11.12. Mehrotra S. Perforator-plus flaps: a new concept in traditional flap design. Plast Reconstr Surg. 2007; 119:590–8.
Article13. Taeger CD, Horch RE, Dragu A, Beier JP, Kneser U. Perforator flaps. A new era in reconstructive surgery. Chirurg. 2012; 83:163–71.14. Eren S, Rübben A, Krein R, Larkin G, Hettich R. Assessment of microcirculation of an axial skin flap using indocyanine green fluorescence angiography. Plast Reconstr Surg. 1995; 96:1636–49.
Article15. Cajozzo M, Jiga LP, Jandali Z, et al. Complications and solutions in propeller flap surgery. Semin Plast Surg. 2020; 34:210–20.
Article16. Lee HW, Yang I, Liu Y, Lee JH, Kim HN. Saline load test and quilting sutures to treat intractable lateral malleolar bursitis. J Foot Ankle Surg. 2021; 60:345–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perforator-Based Propeller Flap for Lower Extremity Reconstruction
- Peroneal Artery Perforator-Based Propeller Flaps for Reconstruction of Soft Tissue Defect around the Ankle Joint: A Report of Four Cases
- Reconstruction of Lateral Malleolar Defects: Adipofascial Turnover Flap Based on the Peroneal Artery Perforator
- Clinical Applications of Peroneal Perforator Flap
- Surgery for Synovial Fistula after Excision of the Lateral Malleolar Bursitis of the Ankle: A Case Report