J Korean Foot Ankle Soc.
2015 Sep;19(3):118-121. 10.14193/jkfas.2015.19.3.118.
Surgery for Synovial Fistula after Excision of the Lateral Malleolar Bursitis of the Ankle: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. cool-cool0829@hanmail.net
- KMID: 2045016
- DOI: http://doi.org/10.14193/jkfas.2015.19.3.118
Abstract
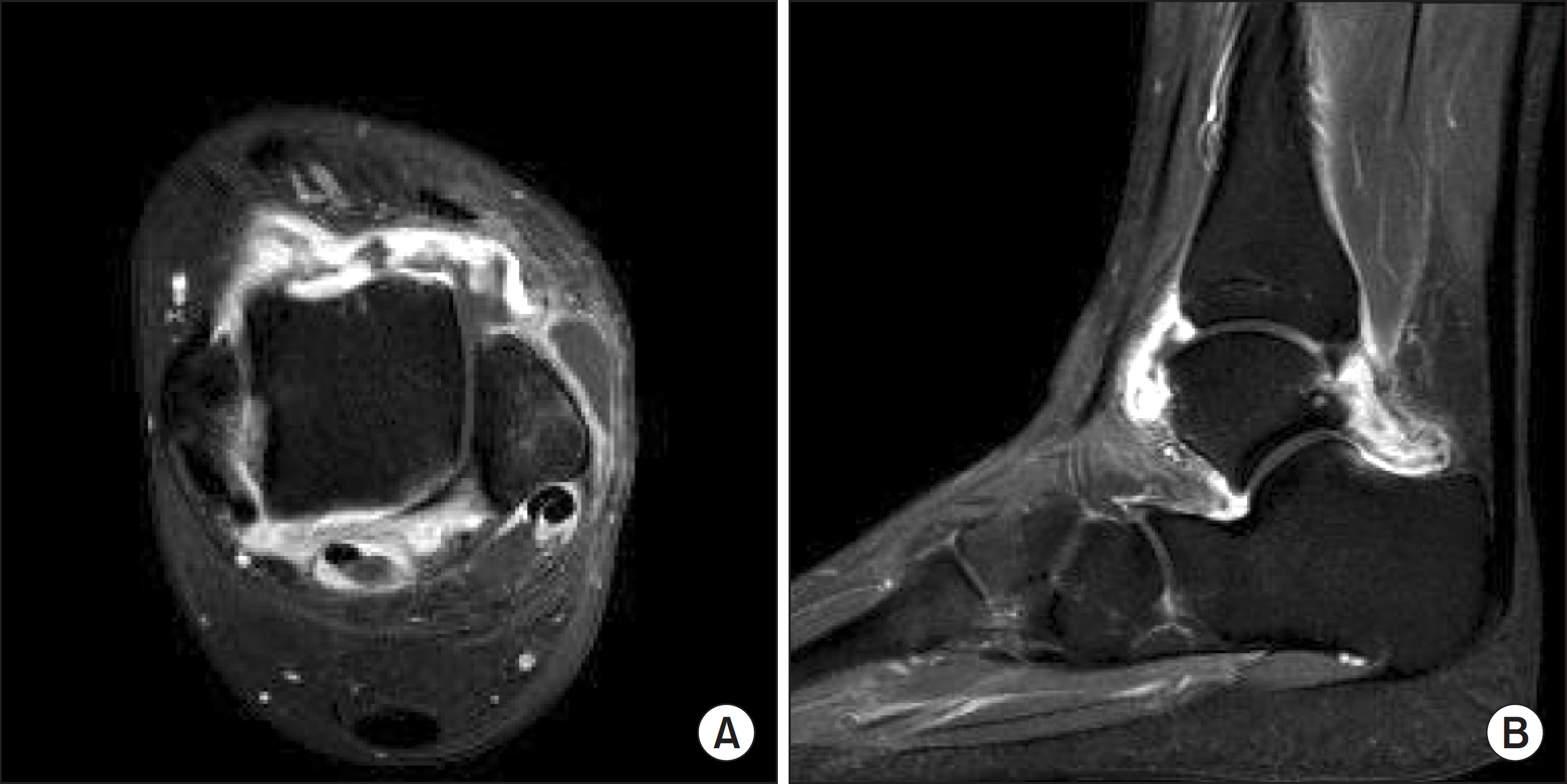
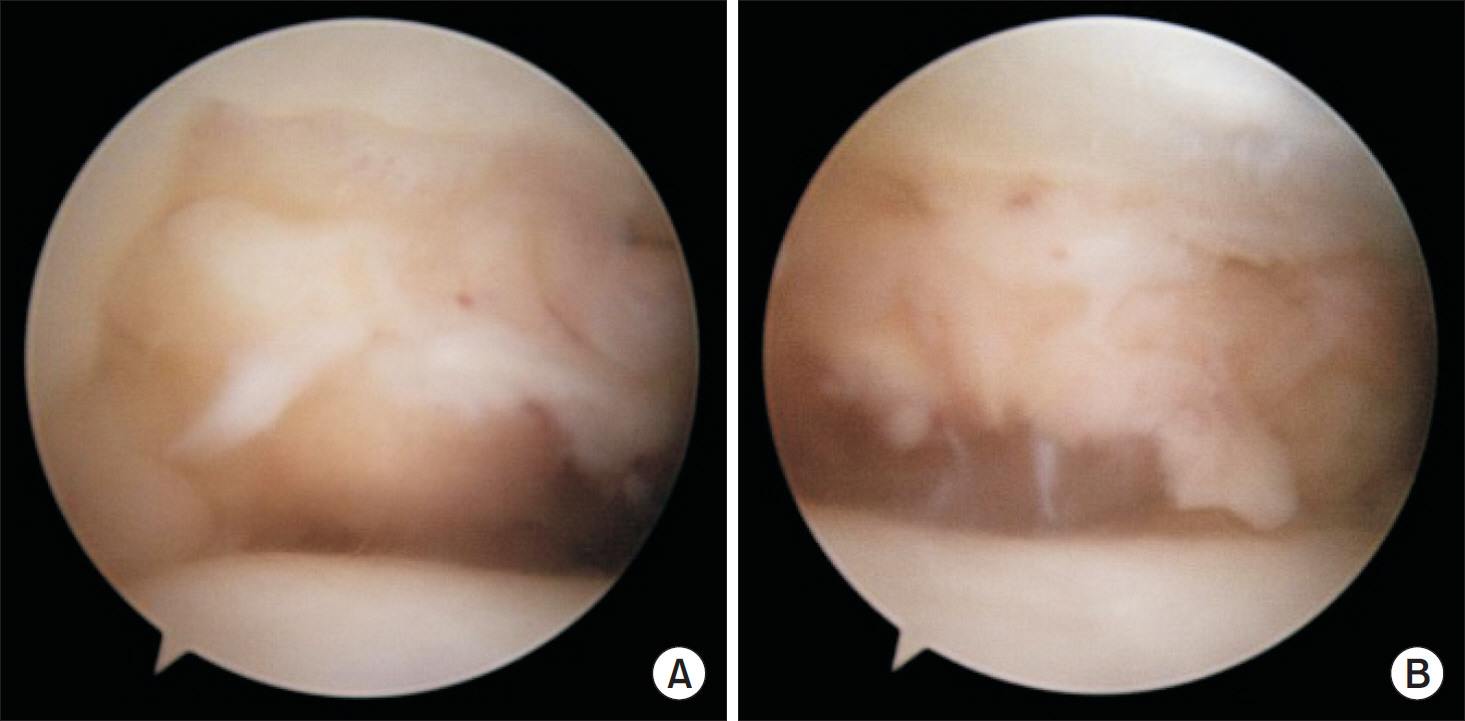
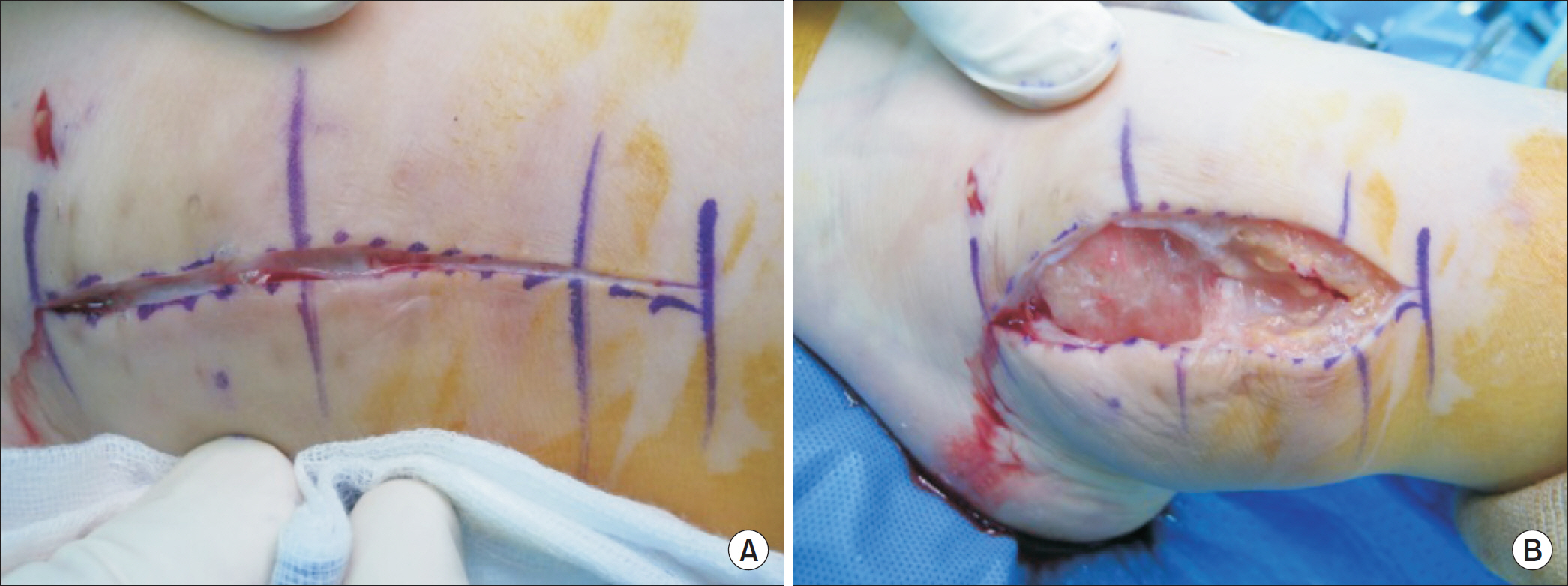
- Lateral malleolar bursitis of the ankle is a commonly encountered disease in the department of orthopedic surgery. Although most cases of lateral malleolar bursitis are managed by conservative treatments, operative treatment is considered in cases of infected bursitis or complication after surgery. There are several potential complications associated with operative treatment, including wound healing problem, skin necrosis, nerve injury, or recurrence. However, synovial fistula of the ankle as a complication after surgery for lateral malleolar bursitis has not been previously reported. The author experienced the complication of synovial fistula after surgery for lateral malleolar bursitis and obtained a satisfactory result in revision surgery for the complication, which was coverage of the fistular formation with a periosteal flap from the distal fibula.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Degreef I, De Smet L. Complications following resection of the olecranon bursa. Acta Orthop Belg. 2006; 72:400–3.2. Brown TD, Varney TE, Micheli LJ. Malleolar bursitis in figure skaters. Indications for operative and nonoperative treatment. Am J Sports Med. 2000; 28:109–11.3. Park KH, Lee J, Choi WJ, Lee JW. OK-432 sclerotherapy for malleolar bursitis of the ankle. Foot Ankle Int. 2013; 34:1389–94.
Article4. Avci S, Sayli U. Lateral premalleolar bursitis as a result of sitting on the foot. Foot Ankle Int. 2001; 22:64–6.
Article5. Choi JH, Lee KT, Lee YK, Kim DH, Kim JR, Chung WC, et al. Endoscopic versus open bursectomy of lateral malleolar bursitis. Knee Surg Sports Traumatol Arthrosc. 2012; 20:1205–8.
Article6. Hashimoto I, Yoshinaga R, Toda M, Nakanishi H. Intractable malleolar bursitis treated with lateral calcaneal artery adipofas-cial flap. Br J Plast Surg. 2003; 56:701–3.
Article7. Méndez-Fernández MA. Treatment of chronic recurrent synovial fistulae with myofascial flaps. Br J Plast Surg. 1993; 46:303–6.8. Proffer DS, Drez D Jr, Daus GP. Synovial fistula of the knee: a complication of arthroscopy. Arthroscopy. 1991; 7:98–100.
Article9. Coulier B, Devyver B, Hamels J. Imaging demonstration of fistulous gas communication between joint and ganglion of medial malleolus. Skeletal Radiol. 2002; 31:57–60.
Article10. Ji JH, Kim WY, Lee YS, Park SE, Ra KH, Kwon OS. Secondary septic arthritis due to lateral malleolar bursitis: a case report. J Korean Foot Ankle Soc. 2006; 10:274–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Negative-Pressure Wound Therapy for Septic Ankle Arthritis Following Intractable Lateral Malleolar Bursitis: A Case Report
- Secondary Septic Arthritis Due to Lateral Malleolar Bursitis: A Case Report
- Unhealed Wound of the Lower Leg due to Synovial Fistula of the Ankle Joint
- The Effect of Indwelling Silk Suture Following Aspiration in the Treatment of Chronic Lateral Malleolar Bursitis
- Anterior Dislocation of the Ankle without Malleolar Fractures: A Case Report