Ann Rehabil Med.
2023 Aug;47(4):282-290. 10.5535/arm.23067.
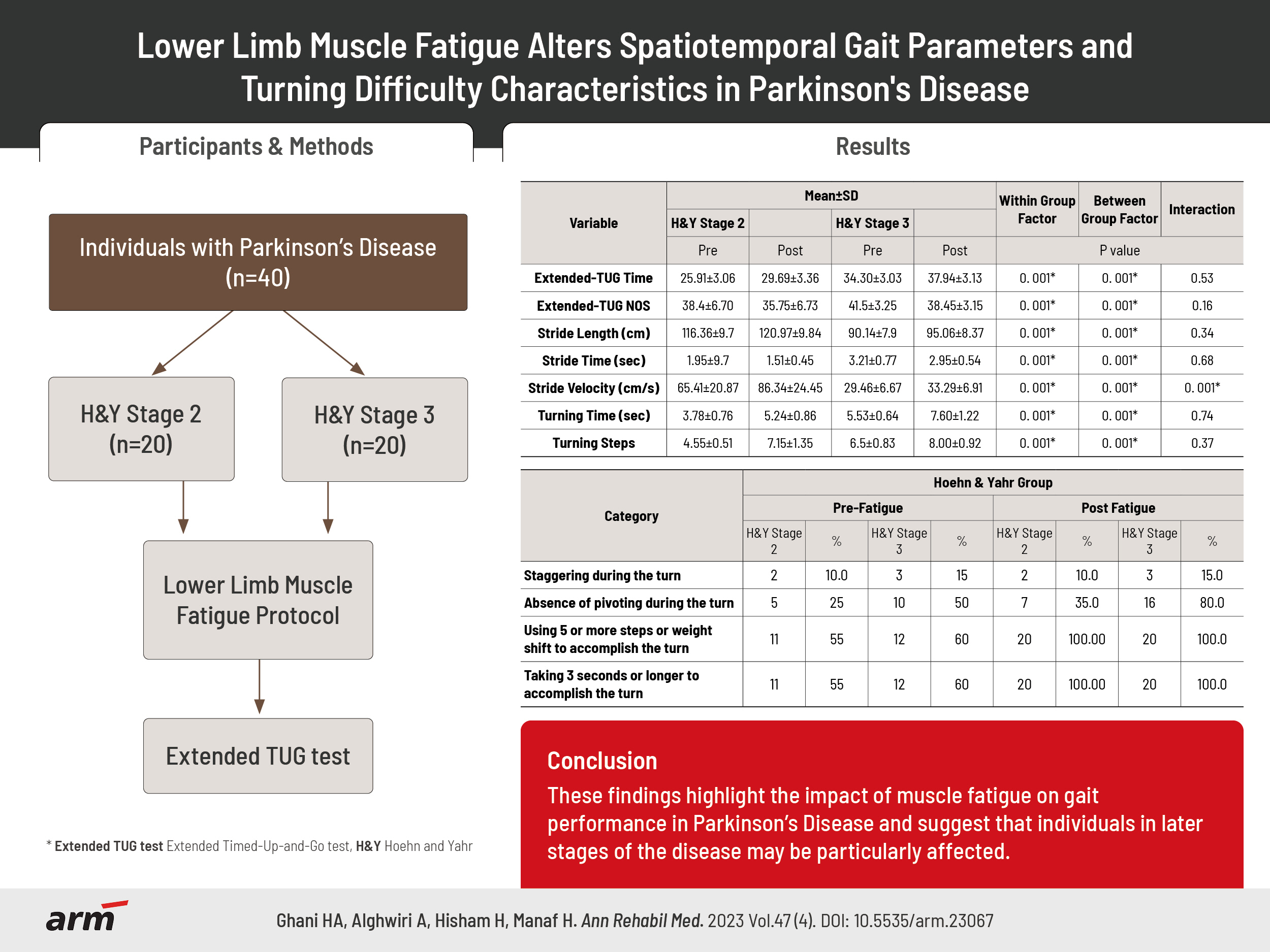
Lower Limb Muscle Fatigue Alters Spatiotemporal Gait Parameters and Turning Difficulty Characteristics in Parkinson’s Disease
- Affiliations
-
- 1Physiotherapy Program, Institut Latihan Kementerian Kesihatan Malaysia, Johor, Malaysia
- 2Department of Physiotherapy, Faculty of Allied Medical Sciences, Applied Science Private University, Amman, Jordan
- 3Physiotherapy Program, Center for Rehabilitation and Special Needs Studies, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 4Centre for Physiotherapy Studies, Faculty of Health Sciences, Universiti Teknologi MARA, Puncak Alam Campus, Puncak Alam, Malaysia
- 5Integrative Pharmacogenomics Institute, Universiti Teknologi MARA, Puncak Alam Campus, Puncak Alam, Malaysia
- KMID: 2545324
- DOI: http://doi.org/10.5535/arm.23067
Abstract
Objective
To determine the effects of lower limb muscle fatigue on spatiotemporal gait parameters and turning difficulty characteristics during the extended Timed Up and Go (extended TUG) test in individuals with different severity stages of Parkinson’s disease (PD).
Methods
Forty individuals with PD, classified as Hoehn and Yahr (H&Y) stages 2 and 3 participated in this pre- and post-experimental study design. The participants performed a continuous sit-to-stand task from a chair based on 30 cycles/min set-up to induce lower limb muscle fatigue. They performed extended TUG test immediately before and after completing the fatigue protocol. Spatiotemporal gait parameters and turning difficulty characteristics were recorded using two GoPro® Hero 4 Silver cameras. Data were subjected to a repeated-measure ANOVA.
Results
Individuals with PD experience significant changes in spatiotemporal gait parameters, specifically stride velocity and length, under conditions of lower limb muscle fatigue (p=0.001). These changes were more pronounced in individuals with PD in the H&Y stage 3 group. Additionally, both PD groups exhibited difficulty with turning, requiring more than five steps to complete a 180° turn and taking more than 3 seconds to accomplish it.
Conclusion
These findings highlight the impact of muscle fatigue on gait performance in PD and suggest that individuals in later stages of the disease may be particularly affected. Further research is needed to explore interventions that can mitigate these gait impairments and improve mobility in individuals with PD.
Keyword
Figure
Reference
-
1. Crenna P, Carpinella I, Rabuffetti M, Calabrese E, Mazzoleni P, Nemni R, et al. The association between impaired turning and normal straight walking in Parkinson's disease. Gait Posture. 2007; 26:172–8.
Article2. Patla AE, Adkin A, Ballard T. Online steering: coordination and control of body center of mass, head and body reorientation. Exp Brain Res. 1999; 129:629–34.
Article3. Thigpen MT, Light KE, Creel GL, Flynn SM. Turning difficulty characteristics of adults aged 65 years or older. Phys Ther. 2000; 80:1174–87.
Article4. Zampieri C, Salarian A, Carlson-Kuhta P, Aminian K, Nutt JG, Horak FB. The instrumented timed up and go test: potential outcome measure for disease modifying therapies in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2010; 81:171–6.
Article5. Radder DLM, Sturkenboom IH, van Nimwegen M, Keus SH, Bloem BR, de Vries NM. Physical therapy and occupational therapy in Parkinson’s disease. Int J Neurosci. 2017; 127:930–43.
Article6. Lord S, Baker K, Nieuwboer A, Burn D, Rochester L. Gait variability in Parkinson’s disease: an indicator of non-dopaminergic contributors to gait dysfunction? J Neurol. 2011; 258:566–72.
Article7. Schlachetzki JCM, Barth J, Marxreiter F, Gossler J, Kohl Z, Reinfelder S, et al. Wearable sensors objectively measure gait parameters in Parkinson’s disease. PLoS One. 2017; 12:e0183989.8. Orcioli-Silva D, Barbieri FA, Dos Santos PCR, Beretta VS, Simieli L, Vitorio R, et al. Double obstacles increase gait asymmetry during obstacle crossing in people with Parkinson's disease and healthy older adults: a pilot study. Sci Rep. 2020; 10:2272.
Article9. Murdock GH, Hubley-Kozey CL. Effect of a high intensity quadriceps fatigue protocol on knee joint mechanics and muscle activation during gait in young adults. Eur J Appl Physiol. 2012; 112:439–49.10. Stevens-Lapsley J, Kluger BM, Schenkman M. Quadriceps muscle weakness, activation deficits, and fatigue with Parkinson disease. Neurorehabil Neural Repair. 2012; 26:533–41.11. Rochester L, Jones D, Hetherington V, Nieuwboer A, Willems AM, Kwakkel G, et al. Gait and gait-related activities and fatigue in Parkinson’s disease: what is the relationship? Disabil Rehabil. 2006; 28:1365–71.12. Santos PC, Gobbi LT, Orcioli-Silva D, Simieli L, van Dieën JH, Barbieri FA. Effects of leg muscle fatigue on gait in patients with Parkinson's disease and controls with high and low levels of daily physical activity. Gait Posture. 2016; 47:86–91.13. Huang YZ, Chang FY, Liu WC, Chuang YF, Chuang LL, Chang YJ. Fatigue and muscle strength involving walking speed in Parkinson's disease: insights for developing rehabilitation strategy for PD. Neural Plast. 2017; 2017:1941980.14. Baer M, Klemetson B, Scott D, Murtishaw AS, Navalta JW, Kinney JW, et al. Effects of fatigue on balance in individuals with Parkinson disease: influence of medication and brain-derived neurotrophic factor genotype. J Neurol Phys Ther. 2018; 42:61–71.
Article15. Weiss A, Mirelman A, Giladi N, Barnes LL, Bennett DA, Buchman AS, et al. Transition between the timed up and go turn to sit subtasks: is timing everything? J Am Med Dir Assoc. 2016; 17:864.e9–15.
Article16. Greene BR, Doheny EP, O'Halloran A, Anne Kenny R. Frailty status can be accurately assessed using inertial sensors and the TUG test. Age Ageing. 2014; 43:406–11.
Article17. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–8.
Article18. Rogers ME, Rogers NL, Takeshima N, Islam MM. Methods to assess and improve the physical parameters associated with fall risk in older adults. Prev Med. 2003; 36:255–64.19. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000; 80:896–903.20. Evans T, Jefferson A, Byrnes M, Walters S, Ghosh S, Mastaglia FL, et al. Extended “Timed Up and Go” assessment as a clinical indicator of cognitive state in Parkinson's disease. J Neurol Sci. 2017; 375:86–91.
Article21. Bedoya-Belmonte JJ, Rodríguez-González MDM, González-Sánchez M, Pitarch JMB, Galán-Mercant A, Cuesta-Vargas AI. İnter-rater and intra-rater reliability of the extended TUG test in elderly participants. BMC Geriatr. 2020; 20:56.
Article22. Wüest S, Massé F, Aminian K, Gonzenbach R, de Bruin ED. Reliability and validity of the inertial sensor-based Timed “Up and Go” test in individuals affected by stroke. J Rehabil Res Dev. 2016; 53:599–610.
Article23. Carvalho DV, Santos RMS, Magalhães HC, Souza MS, Christo PP, Almeida-Leite CM, et al. Can fatigue predict walking capacity of patients with Parkinson’s disease? Arq Neuropsiquiatr. 2020; 78:70–5.
Article24. Salarian A, Horak FB, Zampieri C, Carlson-Kuhta P, Nutt JG, Aminian K. iTUG, a sensitive and reliable measure of mobility. IEEE Trans Neural Syst Rehabil Eng. 2010; 18:303–10.
Article25. Hickey A, Del Din S, Rochester L, Godfrey A. Detecting free-living steps and walking bouts: validating an algorithm for macro gait analysis. Physiol Meas. 2017; 38:N1–15.
Article26. Sun J, Liu YC, Yan SH, Wang SS, Lester DK, Zeng JZ, et al. Clinical gait evaluation of patients with lumbar spine stenosis. Orthop Surg. 2018; 10:32–9.
Article27. Aung N, Bovonsunthonchai S, Hiengkaew V, Tretriluxana J, Rojasavastera R, Pheung-Phrarattanatrai A. Concurrent validity and intratester reliability of the video-based system for measuring gait poststroke. Physiother Res Int. 2020; 25:e1803.
Article28. Skinner JW, Lee HK, Roemmich RT, Amano S, Hass CJ. Execution of activities of daily living in persons with Parkinson disease. Med Sci Sports Exerc. 2015; 47:1906–12.
Article29. Hof AL, van Bockel RM, Schoppen T, Postema K. Control of lateral balance in walking. Experimental findings in normal subjects and above-knee amputees. Gait Posture. 2007; 25:250–8.30. Hof AL, Gazendam MG, Sinke WE. The condition for dynamic stability. J Biomech. 2005; 38:1–8.
Article31. Barbieri FA. Impact of muscle fatigue on mechanics and motor control of walking [dissertation]. Amsterdam: Vrije Universiteit Amsterdam;2013.32. Barbieri FA, dos Santos PC, Simieli L, Orcioli-Silva D, van Dieën JH, Gobbi LT. Interactions of age and leg muscle fatigue on unobstructed walking and obstacle crossing. Gait Posture. 2014; 39:985–90.
Article33. Granacher U, Wolf I, Wehrle A, Bridenbaugh S, Kressig RW. Effects of muscle fatigue on gait characteristics under single and dual-task conditions in young and older adults. J Neuroeng Rehabil. 2010; 7:56.
Article34. Huang S, Cai S, Li G, Chen Y, Ma K, Xie L. sEMG-based detection of compensation caused by fatigue during rehabilitation therapy: a pilot study. IEEE Access. 2019; 7:127055–65.
Article35. Alves G, Wentzel-Larsen T, Larsen JP. Is fatigue an independent and persistent symptom in patients with Parkinson disease? Neurology. 2004; 63:1908–11.
Article36. Barbieri FA, dos Santos PC, Vitório R, van Dieën JH, Gobbi LT. Effect of muscle fatigue and physical activity level in motor control of the gait of young adults. Gait Posture. 2013; 38:702–7.
Article37. Alota Ignacio Pereira V, Augusto Barbieri F, Moura Zagatto A, Cezar Rocha Dos Santos P, Simieli L, Augusto Barbieri R, et al. Muscle fatigue does not change the effects on lower limbs strength caused by aging and Parkinson's disease. Aging Dis. 2018; 9:988–98.
Article38. Hak L, Houdijk H, Steenbrink F, Mert A, van der Wurff P, Beek PJ, et al. Speeding up or slowing down?: gait adaptations to preserve gait stability in response to balance perturbations. Gait Posture. 2012; 36:260–4.
Article39. Bruijn SM, van Dieën JH, Meijer OG, Beek PJ. Is slow walking more stable? J Biomech. 2009; 42:1506–12.
Article40. Mellone S, Mancini M, King LA, Horak FB, Chiari L. The quality of turning in Parkinson’s disease: a compensatory strategy to prevent postural instability? J Neuroeng Rehabil. 2016; 13:39.
Article41. Plotnik M, Giladi N, Hausdorff JM. Bilateral coordination of gait and Parkinson’s disease: the effects of dual tasking. J Neurol Neurosurg Psychiatry. 2009; 80:347–50.
Article42. Hausdorff JM, Balash J, Giladi N. Effects of cognitive challenge on gait variability in patients with Parkinson’s disease. J Geriatr Psychiatry Neurol. 2003; 16:53–8.
Article43. Morris ME, Huxham F, McGinley J, Dodd K, Iansek R. The biomechanics and motor control of gait in Parkinson disease. Clin Biomech (Bristol, Avon). 2001; 16:459–70.
Article44. Rahman S, Griffin HJ, Quinn NP, Jahanshahi M. Quality of life in Parkinson's disease: the relative importance of the symptoms. Mov Disord. 2008; 23:1428–34.
Article45. Hagell P, Brundin L. Towards an understanding of fatigue in Parkinson disease. J Neurol Neurosurg Psychiatry. 2009; 80:489–92.
Article46. Hong M, Perlmutter JS, Earhart GM. A kinematic and electromyographic analysis of turning in people with Parkinson disease. Neurorehabil Neural Repair. 2009; 23:166–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adjustability of Gait Speed in Clinics and Free-Living Environments for People With Parkinson’s Disease
- Spatiotemporal Gait Parameter Comparison for Parkinson's Disease, Multiple System Atrophy, and Other Parkinsonism Diseases
- Effects of the Team Approach Rehabilitation Program on Balance, Gait, and Muscle Strength of Lower Extremities for Elderly Patients with Parkinson's Disease
- Influence of Unilateral Muscle Fatigue in Knee and Ankle Joint on Balance and Gait in Healthy Adults
- Gait Analysis in Patients with Idiopathic Parkinson's Disease during Obstacle Crossing