J Korean Med Sci.
2023 Aug;38(33):e257. 10.3346/jkms.2023.38.e257.
Clinical Characteristics and Followup Assessment in Patients Diagnosed With Alzheimer’s Dementia Through Regional Dementia Centers and Conventional Hospital System
- Affiliations
-
- 1Department of Medicine, Graduate School, Dong-A University, Busan, Korea
- 2Department of Neurology, Pohang Stroke and Spine Hospital, Pohang, Korea
- 3Department of Rehabilitation Medicine, Pohang Stroke and Spine Hospital, Pohang, Korea
- 4Department of Medical Science and Engineering, School of Convergence Science and Technology, Pohang University of Science and Technology, Pohang, Korea
- 5Department of Neurosurgery, Pohang Stroke and Spine Hospital, Pohang, Korea
- 6Department of Neurology, Dong-A University College of Medicine, Busan, Korea
- 7Department of Translational Biomedical Sciences, Graduate School, Dong-A University, Busan, Korea
- KMID: 2545209
- DOI: http://doi.org/10.3346/jkms.2023.38.e257
Abstract
- Background
The rapidly increasing socioeconomic strain caused by dementia represents a significant public health concern. Regional dementia centers (RDCs) have been established nationwide, and they aim to provide timely screening and diagnosis of dementia. This study investigated the clinical characteristics and progression of patients diagnosed with Alzheimer’s dementia (AD), who underwent treatment in RDCs or conventional communitybased hospital systems.
Methods
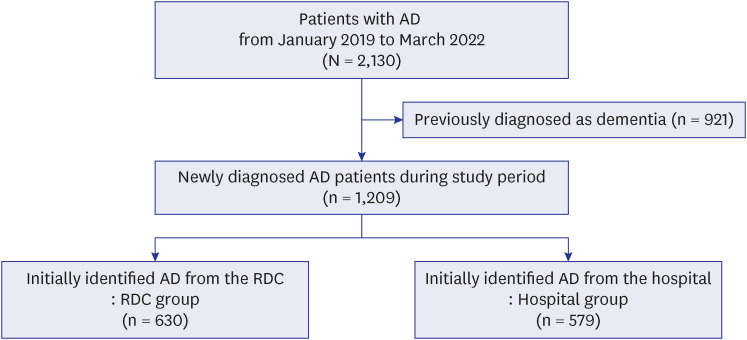
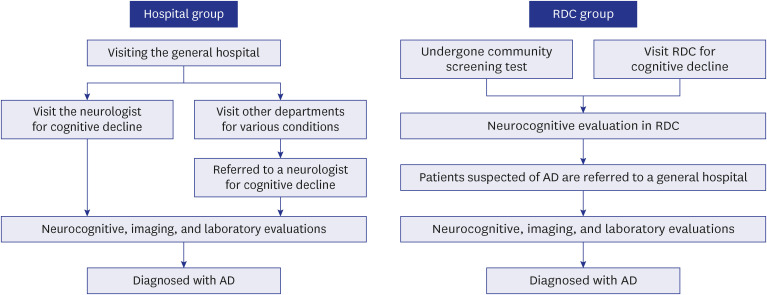
This retrospective single-center cohort study included patients who were diagnosed with AD between January 2019 and March 2022. This study compared two groups of patients: the hospital group, consisting of patients who presented directly to the hospital, and the RDC group, those who were referred to the hospital from the RDCs in Pohang city. The clinical courses of the patients were monitored for a year after AD diagnosis.
Results
A total of 1,209 participants were assigned to the hospital (n = 579) or RDC group (n = 630). The RDC group had a mean age of 80.1 years ± 6.6 years, which was significantly higher than that of the hospital group (P < 0.001). The RDC group had a higher proportion of females (38.3% vs. 31.9%; P = 0.022), higher risk for alcohol consumption (12.4% vs. 3.3%; P < 0.001), and greater number of patients who discontinued treatment 1 year after diagnosis (48.3% vs. 39.0%; P = 0.001). In the linear regression model, the RDC group was independently associated with the clinical dementia rating sum of boxes increment (β = 22.360, R 2 = 0.048, and P < 0.001).
Conclusion
Patients in the RDC group were older, had more advanced stages of conditions, and exhibited a more rapid rate of cognitive decline than patients diagnosed through the conventional hospital system. Our results suggested that RDC contributed to the screening of AD in a local region, and further nationwide study with the RDC database of various areas of Korea is needed.
Figure
Reference
-
1. Cao Q, Tan CC, Xu W, Hu H, Cao XP, Dong Q, et al. The prevalence of dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2020; 73(3):1157–1166. PMID: 31884487.2. Chan KY, Wang W, Wu JJ, Liu L, Theodoratou E, Car J, et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet. 2013; 381(9882):2016–2023. PMID: 23746902.3. Fiest KM, Roberts JI, Maxwell CJ, Hogan DB, Smith EE, Frolkis A, et al. The prevalence and incidence of dementia due to Alzheimer’s disease: a systematic review and meta-analysis. Can J Neurol Sci. 2016; 43(Suppl 1):S51–S82. PMID: 27307128.4. Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in Korea: a systematic review and meta-analysis. J Korean Med Sci. 2014; 29(7):903–912. PMID: 25045221.5. Jang JW, Park JH, Kim S, Lee SH, Lee SH, Kim YJ. Prevalence and incidence of dementia in South Korea: a nationwide analysis of the National Health Insurance Service senior cohort. J Clin Neurol. 2021; 17(2):249–256. PMID: 33835746.6. Shin JH. Dementia epidemiology fact sheet 2022. Ann Rehabil Med. 2022; 46(2):53–59. PMID: 35508924.7. Cheng ST. Dementia caregiver burden: a research update and critical analysis. Curr Psychiatry Rep. 2017; 19(9):64. PMID: 28795386.8. Seok JE. Public long-term care insurance for the elderly in Korea: design, characteristics, and tasks. Soc Work Public Health. 2010; 25(2):185–209. PMID: 20391261.9. Han JW, Jeong H, Park JY, Kim TH, Lee DY, Lee DW, et al. Effects of social supports on burden in caregivers of people with dementia. Int Psychogeriatr. 2014; 26(10):1639–1648. PMID: 25006855.10. Shon C, Yoon H. Health-economic burden of dementia in South Korea. BMC Geriatr. 2021; 21(1):549. PMID: 34645415.11. Porsteinsson AP, Isaacson RS, Knox S, Sabbagh MN, Rubino I. Diagnosis of early Alzheimer’s disease: clinical practice in 2021. J Prev Alzheimers Dis. 2021; 8(3):371–386. PMID: 34101796.12. Choi H, Kim SH. Policy of national responsibility and dementia care. J Korean Med Assoc. 2018; 61(5):309.13. Lee DW. What is needed for the success of national responsibility for dementia. J Korean Med Assoc. 2017; 60(8):618.14. Kim SH. Future policy directions for planning of national responsibility for dementia care. J Korean Med Assoc. 2017; 60(8):622–626.15. Cho SJ, Kang JM. Dementia incidence on the decline in Korea: lessons learned and future directions. J Korean Med Sci. 2019; 34(44):e299. PMID: 31726497.16. Choi H, Kim SH, Lee JH, Lee AY, Park KW, Lee EA, et al. National responsibility policy for dementia care: current and future. J Korean Neurol Assoc. 2018; 36(3):152–158.17. Petersen RC, Wiste HJ, Weigand SD, Fields JA, Geda YE, Graff-Radford J, et al. NIA-AA Alzheimer’s disease framework: clinical characterization of stages. Ann Neurol. 2021; 89(6):1145–1156. PMID: 33772866.18. Wahlund LO, Westman E, van Westen D, Wallin A, Shams S, Cavallin L, et al. Imaging biomarkers of dementia: recommended visual rating scales with teaching cases. Insights Imaging. 2017; 8(1):79–90. PMID: 28004274.19. Vickers AJ. The use of percentage change from baseline as an outcome in a controlled trial is statistically inefficient: a simulation study. BMC Med Res Methodol. 2001; 1(1):6. PMID: 11459516.20. Xu W, Tan L, Wang HF, Tan MS, Tan L, Li JQ, et al. Education and risk of dementia: dose-response meta-analysis of prospective cohort studies. Mol Neurobiol. 2016; 53(5):3113–3123. PMID: 25983035.21. Zhao M, Lv X, Tuerxun M, He J, Luo B, Chen W, et al. Delayed help seeking behavior in dementia care: preliminary findings from the Clinical Pathway for Alzheimer’s Disease in China (CPAD) study. Int Psychogeriatr. 2016; 28(2):211–219. PMID: 26138923.22. Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009; 23(4):306–314. PMID: 19568149.23. Park D, Son KJ, Jeong E, Kim H, Lee SY, Kim JH, et al. Effects of socioeconomic status and residence areas on long-term survival in patients with early-onset dementia: the Korean National Health Insurance Service Database study. J Korean Med Sci. 2022; 37(49):e354. PMID: 36536548.24. Brayne C, Fox C, Boustani M. Dementia screening in primary care: is it time? JAMA. 2007; 298(20):2409–2411. PMID: 18042918.25. Kaduszkiewicz H, Wiese B, van den Bussche H. Self-reported competence, attitude and approach of physicians towards patients with dementia in ambulatory care: results of a postal survey. BMC Health Serv Res. 2008; 8(1):54. PMID: 18321394.26. Chan CQ, Lee KH, Low LL. A systematic review of health status, health seeking behaviour and healthcare utilisation of low socioeconomic status populations in urban Singapore. Int J Equity Health. 2018; 17(1):39. PMID: 29609592.27. Kwon HS, Jeong YW, Kim SH, Park KH, Seo SW, Na HR, et al. Annual incidence of dementia from 2003 to 2018 in metropolitan Seoul, Korea: a population-based study. J Clin Med. 2022; 11(3):819. PMID: 35160270.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention and Treatment of Vascular Dementia
- An Analysis on Prescribing Patterns of Alzheimer's Dementia Treatment and Choline Alfoscerate using HIRA Claims Data
- Biomarkers for Alzheimer's Dementia : Focus on Neuroimaging
- Relationship Between Sleep and Alzheimer’s Dementia
- Differential Diagnosis of Vascular Dementia and Alzheimer's Disease