J Korean Med Sci.
2023 Aug;38(33):e252. 10.3346/jkms.2023.38.e252.
Clinical Manifestation of Ralstonia mannitolilytica Infection in Pediatric Patients and Epidemiological Investigation of Outbreaks
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Infectious Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Office for Infection Control, Asan Medical Center, Seoul, Korea
- KMID: 2545207
- DOI: http://doi.org/10.3346/jkms.2023.38.e252
Abstract
- Background
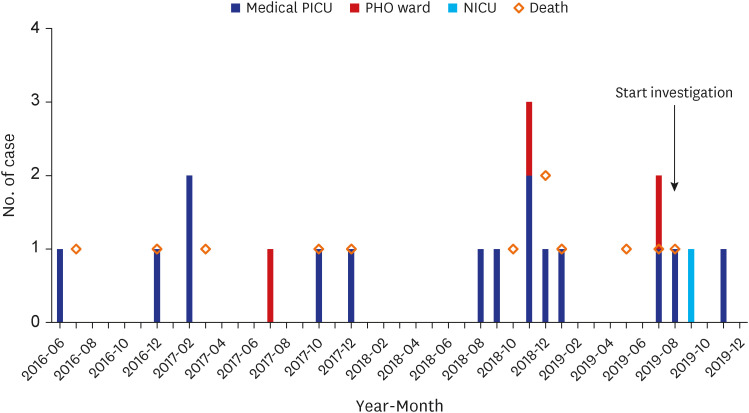
Ralstonia mannitolilytica is a causative organism of nosocomial infections, particularly associated with contaminated water, and resistant to various antibiotics, including carbapenems. Several clusters of R. mannitolilytica infections appeared in children at our institute from August 2018 to November 2019.
Methods
From March 2009 to March 2023, all patients admitted to Asan Medical Center Children’s Hospital in Seoul, Korea, with culture-confirmed R. mannitolilytica and corresponding clinical signs of infection were identified. Epidemiological and environmental investigations were conducted. Polymerase chain reaction (PCR) was performed for the genes of OXA-443 and OXA-444 on R. mannitolilytica isolates.
Results
A total of 18 patients with R. mannitolilytica infection were included in this study, with 94.4% (17/18) and 5.6% (1/18) being diagnosed with pneumonia and central line-associated bloodstream infection, respectively. All-cause 30-day mortality rate was 61.1% (11/18), and seven of the fatal cases were caused by R. mannitolilytica infection itself. The resistance rates to meropenem and imipenem werew 94.4% (17/18) and 5.6% (1/18), respectively. Although four out of nine meropenem-resistant R.mannitolilytica isolates had positive PCR results for OXA-443 and OXA-444 genes, there were no significant differences in antimicrobial susceptibility patterns. Environmental sampling identified R. mannitolylica at two sites: a cold-water tap of a water purifier and an exhalation circuit of a patient mechanical ventilator.After implementing and improving adherence to infection control policies, no additional R. mannitolilyticainfection cases have been reported since December 2019.
Conclusion
R. mannitolilytica can cause life-threatening infections with high mortality in fragile pediatric populations. To prevent outbreaks, healthcare workers should be aware of R. mannitolilytica infections and strive to comply with infection control policies.
Figure
Reference
-
1. Fang Q, Feng Y, Feng P, Wang X, Zong Z. Nosocomial bloodstream infection and the emerging carbapenem-resistant pathogen Ralstonia insidiosa . BMC Infect Dis. 2019; 19(1):334. PMID: 31014269.2. Ryan MP, Adley CC. Ralstonia spp.: emerging global opportunistic pathogens. Eur J Clin Microbiol Infect Dis. 2014; 33(3):291–304. PMID: 24057141.3. Lucarelli C, Di Domenico EG, Toma L, Bracco D, Prignano G, Fortunati M, et al. Ralstonia mannitolilytica infections in an oncologic day ward: description of a cluster among high-risk patients. Antimicrob Resist Infect Control. 2017; 6(1):20. PMID: 28191308.4. Gröbner S, Heeg P, Autenrieth IB, Schulte B. Monoclonal outbreak of catheter-related bacteraemia by Ralstonia mannitolilytica on two haemato-oncology wards. J Infect. 2007; 55(6):539–544. PMID: 17881058.5. Basso M, Venditti C, Raponi G, Navazio AS, Alessandri F, Giombini E, et al. A case of persistent bacteraemia by Ralstonia mannitolilytica and Ralstonia pickettii in an intensive care unit. Infect Drug Resist. 2019; 12:2391–2395. PMID: 31447567.6. Boattini M, Bianco G, Biancone L, Cavallo R, Costa C. Ralstonia mannitolilytica bacteraemia: a case report and literature review. Infez Med. 2018; 26(4):374–378. PMID: 30555144.7. Jhung MA, Sunenshine RH, Noble-Wang J, Coffin SE, St John K, Lewis FM, et al. A national outbreak of Ralstonia mannitolilytica associated with use of a contaminated oxygen-delivery device among pediatric patients. Pediatrics. 2007; 119(6):1061–1068. PMID: 17545371.8. Liu EM, Pegg KM, Oelschlaeger P. The sequence-activity relationship between metallo-β-lactamases IMP-1, IMP-6, and IMP-25 suggests an evolutionary adaptation to meropenem exposure. Antimicrob Agents Chemother. 2012; 56(12):6403–6406. PMID: 23006757.9. Souza DC, Palmeiro JK, Maestri AC, Cogo LL, Rauen CH, Graaf ME, et al. Ralstonia mannitolilytica bacteremia in a neonatal intensive care unit. Rev Soc Bras Med Trop. 2018; 51(5):709–711. PMID: 30304284.10. Vaneechoutte M, De Baere T, Wauters G, Steyaert S, Claeys G, Vogelaers D, et al. One case each of recurrent meningitis and hemoperitoneum infection with Ralstonia mannitolilytica. J Clin Microbiol. 2001; 39(12):4588–4590. PMID: 11724893.11. Liu CX, Yan C, Zhang P, Li FQ, Yang JH, Li XY. Ralstonia mannitolilytica-induced septicemia and homology analysis in infected patients: 3 case reports. Jundishapur J Microbiol. 2016; 9(7):e34373. PMID: 27679705.12. Falcone-Dias MF, Vaz-Moreira I, Manaia CM. Bottled mineral water as a potential source of antibiotic resistant bacteria. Water Res. 2012; 46(11):3612–3622. PMID: 22534119.13. Fluit AC, Bayjanov JR, Aguilar MD, Cantón R, Tunney MM, Elborn JS, et al. Characterization of clinical Ralstonia strains and their taxonomic position. Antonie van Leeuwenhoek. 2021; 114(10):1721–1733. PMID: 34463860.14. Suzuki M, Nishio H, Asagoe K, Kida K, Suzuki S, Matsui M, et al. Genome sequence of a carbapenem-resistant strain of Ralstonia mannitolilytica . Genome Announc. 2015; 3(3):e00405-15. PMID: 25953190.15. Girlich D, Naas T, Nordmann P. OXA-60, a chromosomal, inducible, and imipenem-hydrolyzing class D beta-lactamase from Ralstonia pickettii . Antimicrob Agents Chemother. 2004; 48(11):4217–4225. PMID: 15504844.16. Centers for Disease Control and Prevention. Pneumonia (Ventilator-associated [VAP] and non-ventilatorassociated Pneumonia [PNEU]) Event. https://www.cdc.gov/nhsn/pdfs/pscmanual/6pscvapcurrent.pdf .17. Centers for Disease Control and Prevention. Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection). https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf .18. Clinical and Laboratory Standards Institute(CLSI). Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute. 25th ed. 2015. CLSI supplement M100.19. Green H, Jones AM. Emerging Gram-negative bacteria: pathogenic or innocent bystanders. Curr Opin Pulm Med. 2018; 24(6):592–598. PMID: 30095492.20. Block C, Ergaz-Shaltiel Z, Valinsky L, Temper V, Hidalgo-Grass C, Minster N, et al. Déjà vu: Ralstonia mannitolilytica infection associated with a humidifying respiratory therapy device, Israel, June to July 2011. Euro Surveill. 2013; 18(18):20471. PMID: 23725776.21. Said M, van Hougenhouck-Tulleken W, Naidoo R, Mbelle N, Ismail F. Outbreak of Ralstonia mannitolilytica bacteraemia in patients undergoing haemodialysis at a tertiary hospital in Pretoria, South Africa. Antimicrob Resist Infect Control. 2020; 9(1):117. PMID: 32727576.22. Green HD, Bright-Thomas R, Kenna DT, Turton JF, Woodford N, Jones AM. Ralstonia infection in cystic fibrosis. Epidemiol Infect. 2017; 145(13):2864–2872. PMID: 28791938.23. Coman I, Bilodeau L, Lavoie A, Carricart M, Tremblay F, Zlosnik JE, et al. Ralstonia mannitolilytica in cystic fibrosis: a new predictor of worse outcomes. Respir Med Case Rep. 2017; 20:48–50. PMID: 27995056.24. Flemming HC, Wingender J, Szewzyk U, Steinberg P, Rice SA, Kjelleberg S. Biofilms: an emergent form of bacterial life. Nat Rev Microbiol. 2016; 14(9):563–575. PMID: 27510863.25. Park S, Lee E, So HJ, Yoo RN, Lee J. The impact of antibiotic burden on the selective resistance of gram negative bacteria in children. Pediatr Infect Vaccine. 2021; 28(2):82–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Source Investigation and Control of Ralstonia mannitolilytica Bacteremia in a Neonatal Intensive Care Unit: A Case Report
- Epidemiological Characteristic and Risk Factor of COVID-19 Cluster Related to Educational Facilities in Gangwon-do, Korea (December 10, 2020–September 23, 2021)
- A Case of Corneal Ulcer Caused by Ralstonia Paucula Infection
- Epidemiological characteristics of carbapenemaseproducing Enterobacteriaceae outbreaks in the Republic of Korea between 2017 and 2022
- Current status and challenges in disease surveillance and epidemiological investigation systems for companion animals in South Korea