Korean J Orthod.
2023 Jul;53(4):232-240. 10.4041/kjod23.020.
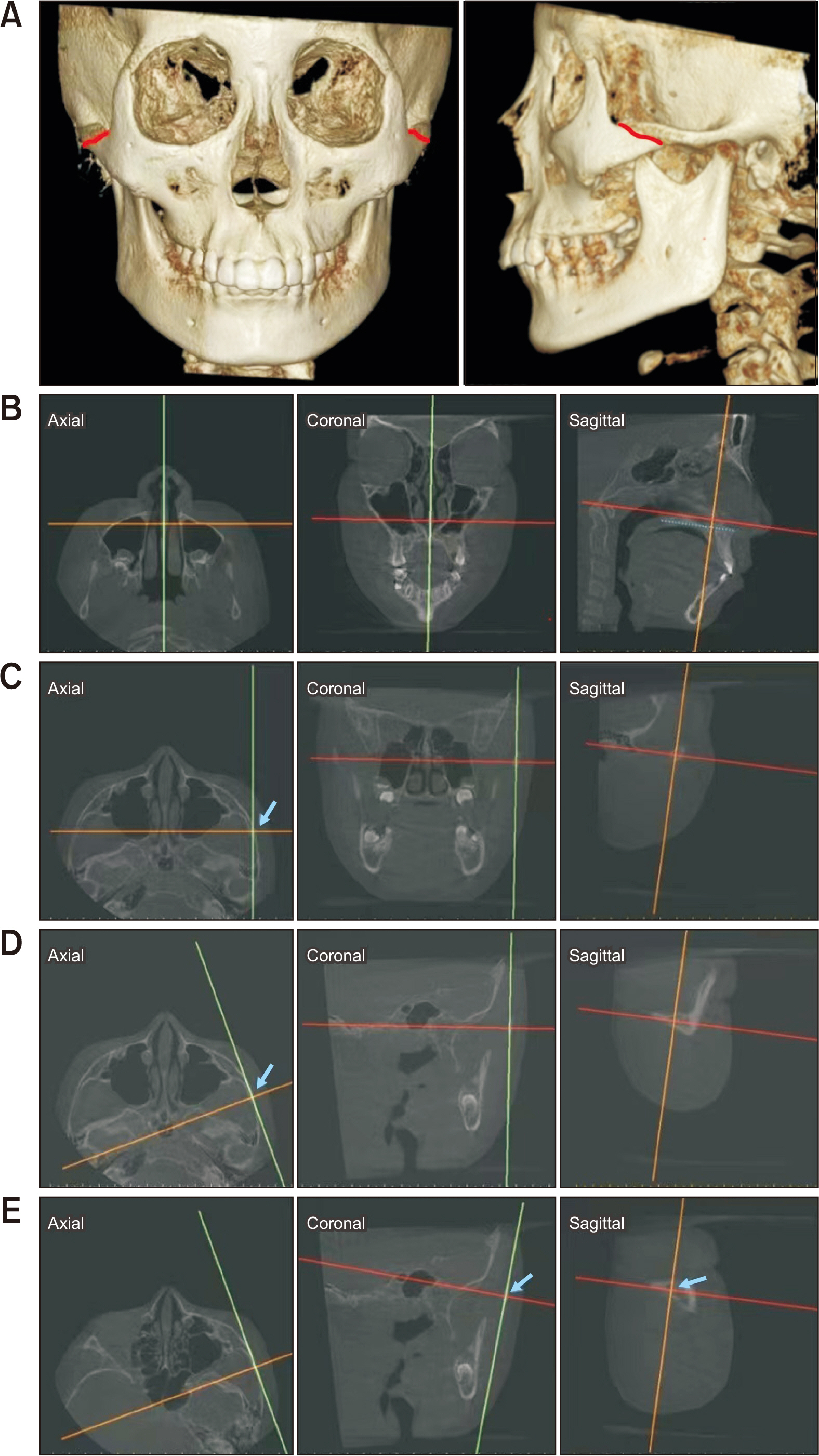
Zygomaticotemporal suture maturation evaluation in Chinese population using cone-beam computed tomography images
- Affiliations
-
- 1Department of Orthodontics, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2College of Stomatology, Shanghai Jiao Tong University, Shanghai, China c National Center for Stomatology, Shanghai, China
- 3National Clinical Research Center for Oral Diseases, Shanghai, China
- 4Shanghai Key Laboratory of Stomatology, Shanghai, China
- 5Shanghai Research Institute of Stomatology, Shanghai, China
- KMID: 2545039
- DOI: http://doi.org/10.4041/kjod23.020
Abstract
Objective
This study aimed to evaluate the zygomaticotemporal suture (ZTS) maturation, analyze the age distribution patterns of ZTS maturation stages, and investigate the relationship between ZTS and cervical vertebral maturation (CVM).
Methods
A total of 261 patients who underwent cone-beam computed tomography (112 males, mean age, 13.1 ± 3.3 years; 149 females, mean age, 13.7 ± 3.1 years) were examined to evaluate the ZTS stages. The ZTS stages were defined based on a modified method from previous studies on zygomaticomaxillary sutures. Differences between groups and correlations between indicators were analyzed using the Spearman correlation test, intraclass coefficient of correlation (ICC), one-way analysis of variance and rank sum test. Statistical significance was set at p < 0.05. The diagnostic value of CVM stages in identifying ZTS maturation stages was evaluated using positive likelihood ratios (LRs).
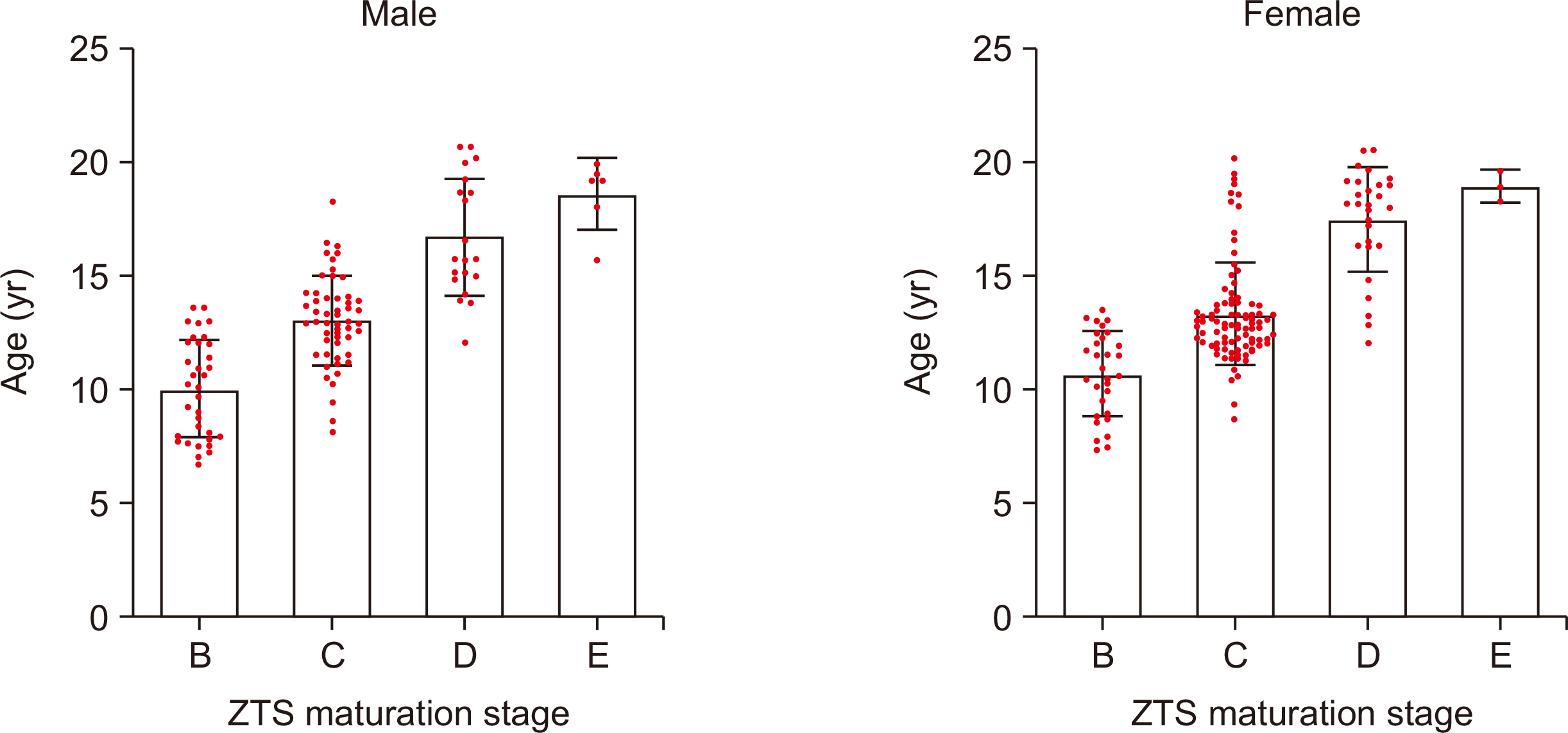
Results
A positive relationship was found between the ZTS and CVM stage (r = 0.747, ICC = 0.621, p < 0.01) and between the ZTS stage and chronological age (r = 0.727, ICC = 0.330, p < 0.01). Positive LRs > 10 were found for several cervical stages (CSs), including CS1 and CS2 for the diagnosis of stage B, CS1 to CS3 for the diagnosis of stages B and C, and CS6 for the diagnosis of stages D and E.
Conclusions
The ZTS maturation stage may be more relevant to the CVM stage than to the chronological age. The CVM stages can be good indicators for clinical decisions regarding maxillary protraction, except for CS4 and CS5.
Figure
Reference
-
1. Celikoglu M, Buyukcavus MH. 2017; Changes in pharyngeal airway dimensions and hyoid bone position after maxillary protraction with different alternate rapid maxillary expansion and construction protocols: a prospective clinical study. Angle Orthod. 87:519–25. https://doi.org/10.2319/082316-632.1. DOI: 10.2319/082316-632.1. PMID: 28139938. PMCID: PMC8366701.
Article2. Willmann JH, Nienkemper M, Tarraf NE, Wilmes B, Drescher D. 2018; Early Class III treatment with Hybrid-Hyrax - Facemask in comparison to Hybrid-Hyrax-Mentoplate - skeletal and dental outcomes. Prog Orthod. 19:42. https://doi.org/10.1186/s40510-018-0239-8. DOI: 10.1186/s40510-018-0239-8. PMID: 30345472. PMCID: PMC6196146. PMID: 2fda100b26f54c179891b36314ca90b6.
Article3. Al Dayeh A, Williams RA, Trojan TM, Claro WI. 2019; Deformation of the zygomaticomaxillary and nasofrontal sutures during bone-anchored maxillary protraction and reverse-pull headgear treatments: an ex-vivo study. Am J Orthod Dentofacial Orthop. 156:745–57. https://doi.org/10.1016/j.ajodo.2018.12.019. DOI: 10.1016/j.ajodo.2018.12.019. PMID: 31784008.
Article4. Vracar TR, Claro W, Vracar ME 2nd, Jenkins RS, Bland L, Dayeh AA. 2021; Sutural deformation during bone-anchored maxillary protraction. J Oral Biol Craniofac Res. 11:447–50. https://doi.org/10.1016/j.jobcr.2021.05.008. DOI: 10.1016/j.jobcr.2021.05.008. PMID: 34094844. PMCID: PMC8167158.
Article5. Herring SW. 2008; Mechanical influences on suture development and patency. Front Oral Biol. 12:41–56. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826139/. DOI: 10.1159/000115031. PMID: 18391494. PMCID: PMC2826139.
Article6. Tong F, Liu F, Liu J, Xiao C, Liu J, Wu J. 2017; Effects of a magnetic palatal expansion appliance with reactivation system: an animal experiment. Am J Orthod Dentofacial Orthop. 151:132–42. https://doi.org/10.1016/j.ajodo.2016.06.030. DOI: 10.1016/j.ajodo.2016.06.030. PMID: 28024766.
Article7. Curtis N, Witzel U, Fagan MJ. 2014; Development and three-dimensional morphology of the zygomaticotemporal suture in primate skulls. Folia Primatol (Basel). 85:77–87. https://doi.org/10.1159/000357526. DOI: 10.1159/000357526. PMID: 24481002.8. Kajan ZD, Nasab NK, Eghrari N. 2018; Quantitative evaluation of midpalatal suture opening and its relation with zygomaticomaxillary suture status in patients aged 7-25 years using cone beam computed tomography images: in an Iranian population. Contemp Clin Dent. 9(Suppl 1):S89–94. https://doi.org/10.4103/ccd.ccd_71_18. DOI: 10.4103/ccd.ccd_71_18. PMID: 29962771. PMCID: PMC6006867.9. Yin J, Liao L, Lu L, Tong H, Zhang X, Zhao Z. 2015; Changes in the zygomaticomaxillary suture during aging. J Craniofac Surg. 26:2201–6. https://doi.org/10.1097/SCS.0000000000002141. DOI: 10.1097/SCS.0000000000002141. PMID: 26468810.10. Melsen B. 1975; Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 68:42–54. https://doi.org/10.1016/0002-9416(75)90158-x. DOI: 10.1016/0002-9416(75)90158-X. PMID: 1056143.11. Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr. 2013; Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 144:759–69. https://doi.org/10.1016/j.ajodo.2013.04.022. DOI: 10.1016/j.ajodo.2013.04.022. PMID: 24182592. PMCID: PMC4185298.12. Angelieri F, Franchi L, Cevidanes LHS, Hino CT, Nguyen T, McNamara JA Jr. 2017; Zygomaticomaxillary suture maturation: a predictor of maxillary protraction? Part I - a classification method. Orthod Craniofac Res. 20:85–94. https://doi.org/10.1111/ocr.12143. DOI: 10.1111/ocr.12143. PMID: 28414869. PMCID: PMC5503123.13. Angelieri F, Ruellas AC, Yatabe MS, Cevidanes LHS, Franchi L, Toyama-Hino C, et al. 2017; Zygomaticomaxillary suture maturation: part II-the influence of sutural maturation on the response to maxillary protraction. Orthod Craniofac Res. 20:152–63. https://doi.org/10.1111/ocr.12191. DOI: 10.1111/ocr.12191. PMID: 28660731. PMCID: PMC5698016.14. Ok G, Sen Yilmaz B, Aksoy DO, Kucukkeles N. 2021; Maturity evaluation of orthodontically important anatomic structures with computed tomography. Eur J Orthod. 43:8–14. https://doi.org/10.1093/ejo/cjaa009. DOI: 10.1093/ejo/cjaa009. PMID: 32006443.15. Li R, Shan Y, Li Y, Huang S, Tong Q, Zhou Z, et al. 2022; Zygomaticomaxillary suture maturation evaluation in patients with and without cleft lip and palate. Am J Orthod Dentofacial Orthop. 162:162–72. https://doi.org/10.1016/j.ajodo.2021.01.030. DOI: 10.1016/j.ajodo.2021.01.030. PMID: 35654687.16. Jang HI, Kim SC, Chae JM, Kang KH, Cho JW, Chang NY, et al. 2016; Relationship between maturation indices and morphology of the midpalatal suture obtained using cone-beam computed tomography images. Korean J Orthod. 46:345–55. https://doi.org/10.4041/kjod.2016.46.6.345. DOI: 10.4041/kjod.2016.46.6.345. PMID: 27896208. PMCID: PMC5118213.17. Kim KY, Bayome M, Park JH, Kim KB, Mo SS, Kook YA. 2015; Displacement and stress distribution of the maxillofacial complex during maxillary protraction with buccal versus palatal plates: finite element analysis. Eur J Orthod. 37:275–83. https://doi.org/10.1093/ejo/cju039. DOI: 10.1093/ejo/cju039. PMID: 25090997.18. Lee NK, Baek SH. 2012; Stress and displacement between maxillary protraction with miniplates placed at the infrazygomatic crest and the lateral nasal wall: a 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 141:345–51. https://doi.org/10.1016/j.ajodo.2011.07.021. DOI: 10.1016/j.ajodo.2011.07.021. PMID: 22381495.19. Buyukcavus MH, Kale B. 2021; Effects of different types of maxillary protraction on maxilla with finite element analysis. J Pak Med Assoc. 71:877–82. https://doi.org/10.47391/JPMA.1087. DOI: 10.47391/JPMA.1087. PMID: 34057939. PMID: 58d595a180dc4b42a89d3cb007ae4fe7.20. Zhao N, Xu Y, Chen Y, Xu Y, Han X, Wang L. 2008; Effects of Class III magnetic orthopedic forces on the craniofacial sutures of rhesus monkeys. Am J Orthod Dentofacial Orthop. 133:401–9. https://doi.org/10.1016/j.ajodo.2006.04.035. DOI: 10.1016/j.ajodo.2006.04.035. PMID: 18331940.21. Kambara T. 1977; Dentofacial changes produced by extraoral forward force in the Macaca irus. Am J Orthod. 71:249–77. https://doi.org/10.1016/0002-9416(77)90187-7. DOI: 10.1016/0002-9416(77)90187-7. PMID: 402814.22. Baccetti T, Franchi L, McNamara JA Jr.. 2005; The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 11:119–29. https://doi.org/10.1053/j.sodo.2005.04.005. DOI: 10.1053/j.sodo.2005.04.005.23. McGee S. 2002; Simplifying likelihood ratios. J Gen Intern Med. 17:646–9. https://doi.org/10.1046/j.1525-1497.2002.10750.x. DOI: 10.1046/j.1525-1497.2002.10750.x. PMID: 12213147. PMCID: PMC1495095.24. Lee SH, Koh SD, Chung DH, Lee JW, Lee SM. 2020; Comparison of skeletal anchorage and tooth-borne maxillary protraction followed by fixed appliance in Class III malocclusion. Eur J Orthod. 42:193–9. https://doi.org/10.1093/ejo/cjz086. DOI: 10.1093/ejo/cjz086. PMID: 31750516.25. Buyukcavus MH, Kale B, Aydemir B. 2020; Comparison of treatment effects of different maxillary protraction methods in skeletal class III patients. Orthod Craniofac Res. 23:445–54. https://doi.org/10.1111/ocr.12389. DOI: 10.1111/ocr.12389. PMID: 32406170.26. Liang S, Wang F, Chang Q, Bai Y. 2021; Three-dimensional comparative evaluation of customized bone-anchored vs tooth-borne maxillary protraction in patients with skeletal Class III malocclusion. Am J Orthod Dentofacial Orthop. 160:374–84. https://doi.org/10.1016/j.ajodo.2020.04.034. DOI: 10.1016/j.ajodo.2020.04.034. PMID: 34172344.27. Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, et al. 2015; Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 44:20140197. https://doi.org/10.1259/dmfr.20140197. Erratum in: Dentomaxillofac Radiol 2015;44:20159003. https://doi.org/10.1259/dmfr.20159003. DOI: 10.1259/dmfr.20159003. PMID: 25874892. PMCID: PMC4628416.28. Kaasalainen T, Ekholm M, Siiskonen T, Kortesniemi M. 2021; Dental cone beam CT: an updated review. Phys Med. 88:193–217. https://doi.org/10.1016/j.ejmp.2021.07.007. DOI: 10.1016/j.ejmp.2021.07.007. PMID: 34284332.29. Spin-Neto R, Matzen LH, Schropp L, Gotfredsen E, Wenzel A. 2016; Movement characteristics in young patients and the impact on CBCT image quality. Dentomaxillofac Radiol. 45:20150426. https://doi.org/10.1259/dmfr.20150426. DOI: 10.1259/dmfr.20150426. PMID: 26915407. PMCID: PMC4846179.30. Angelieri F, Franchi L, Cevidanes LH, Bueno-Silva B, McNamara JA Jr. 2016; Prediction of rapid maxillary expansion by assessing the maturation of the midpalatal suture on cone beam CT. Dental Press J Orthod. 21:115–25. https://doi.org/10.1590/2177-6709.21.6.115-125.sar. DOI: 10.1590/2177-6709.21.6.115-125.sar. PMID: 28125147. PMCID: PMC5278941.31. Tonello DL, Ladewig VM, Guedes FP, Ferreira Conti ACC, Almeida-Pedrin RR, Capelozza-Filho L. 2017; Midpalatal suture maturation in 11- to 15-year-olds: a cone-beam computed tomographic study. Am J Orthod Dentofacial Orthop. 152:42–8. https://doi.org/10.1016/j.ajodo.2016.11.028. DOI: 10.1016/j.ajodo.2016.11.028. PMID: 28651767.32. Alesbury HS, Ubelaker DH, Bernstein R. 2013; Utility of the frontonasal suture for estimating age at death in human skeletal remains. J Forensic Sci. 58:104–8. https://doi.org/10.1111/j.1556-4029.2012.02193.x. DOI: 10.1111/j.1556-4029.2012.02193.x. PMID: 22621250.33. Rice DP. 2008; Developmental anatomy of craniofacial sutures. Front Oral Biol. 12:1–21. https://doi.org/10.1159/000115028. DOI: 10.1159/000115028. PMID: 18391492.34. Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B. 2007; Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop. 68:364–76. https://doi.org/10.1007/s00056-007-0729-7. DOI: 10.1007/s00056-007-0729-7. PMID: 17882364.35. Mahdian A, Safi Y, Dalaie K, Kavousinejad S, Behnaz M. 2020; Correlation assessment of cervical vertebrae maturation stage and mid-palatal suture maturation in an Iranian population. J World Fed Orthod. 9:112–6. https://doi.org/10.1016/j.ejwf.2020.05.004. DOI: 10.1016/j.ejwf.2020.05.004. PMID: 32800572.36. Angelieri F, Franchi L, Cevidanes LH, McNamara JA Jr. 2015; Diagnostic performance of skeletal maturity for the assessment of midpalatal suture maturation. Am J Orthod Dentofacial Orthop. 148:1010–6. https://doi.org/10.1016/j.ajodo.2015.06.016. DOI: 10.1016/j.ajodo.2015.06.016. PMID: 26672707.37. Mellion ZJ, Behrents RG, Johnston LE Jr. 2013; The pattern of facial skeletal growth and its relationship to various common indexes of maturation. Am J Orthod Dentofacial Orthop. 143:845–54. https://doi.org/10.1016/j.ajodo.2013.01.019. DOI: 10.1016/j.ajodo.2013.01.019. PMID: 23726335.38. Liu WT, Wang YR, Wang XD, Zhou YH. 2022; [A cone-beam computed tomography evaluation of three-dimensional changes of circummaxillary sutures following maxillary protraction with alternate rapid palatal expansions and constrictions]. Beijing Da Xue Xue Bao Yi Xue Ban. 54:346–55. Chinese.DOI: 10.19723/j.issn.1671-167X.2022.02.024. PMID: 35435203. PMCID: PMC9069022.39. Isfeld D, Flores-Mir C, Leon-Salazar V, Lagravère M. 2019; Evaluation of a novel palatal suture maturation classification as assessed by cone-beam computed tomography imaging of a pre- and postexpansion treatment cohort. Angle Orthod. 89:252–61. https://doi.org/10.2319/040518-258.1. DOI: 10.2319/040518-258.1. PMID: 30457354. PMCID: PMC8120889.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Midpalatal Suture Maturation in Young Koreans Using Cone-Beam Computed Tomography
- Evaluation of Midpalatal Suture Maturation using Cone-Beam Computed Tomography in Children and Adolescents
- Quantitative evaluation of midpalatal suture maturation via fractal analysis
- Relationship between maturation indices and morphology of the midpalatal suture obtained using cone-beam computed tomography images
- Assessment of Midpalatal Suture Maturation by Skeletal Maturity on Hand Wrist Radiographs