J Korean Med Sci.
2023 Jul;38(30):e225. 10.3346/jkms.2023.38.e225.
Change in Severity and Clinical Manifestation of MIS-C Over SARSCoV-2 Variant Outbreaks in Korea
- Affiliations
-
- 1Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Pediatrics, Bundang Jesaeng General Hospital, Seongnam, Korea
- 4Department of Pediatrics, Nowon Eulji University Hospital, Seoul, Korea
- 5Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Pediatrics, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Department of Pediatrics, School of Medicine Kyungpook National University, Daegu, Korea
- 8Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea
- 9Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- 10Department of Pediatrics, Kangbuk Samsung Hospital, Seoul, Korea
- 11Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea
- 12Director General for Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Korea
- KMID: 2544949
- DOI: http://doi.org/10.3346/jkms.2023.38.e225
Abstract
- Background
There is difference in the incidence of multi-system inflammatory syndrome in children (MIS-C) in patients with different variants of severe acute respiratory syndrome coronavirus 2, however, little is known about the epidemiology in Asian countries. We investigated and compared the epidemiology of the MIS-C during omicron-dominant period with that of previous periods in South Korea.
Methods
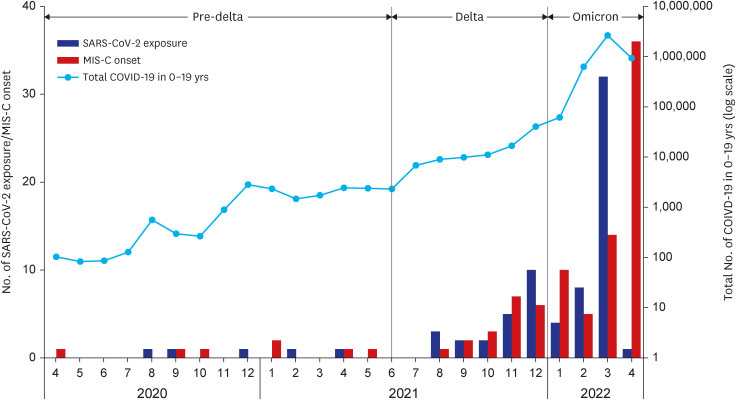
We obtained clinical, epidemiological and laboratory data on MIS-C cases from national MIS-C surveillance in South Korea. We defined pre-delta period as January 2020–May 2021; delta period as June 2021–December 2021; and omicron period as January 2022–April 2022. We describe the clinical characteristics and outcomes of MIS-C patients by period.
Results
A total of 91 cases were assessed to be MIS-C cases. Number of MIS-C cases have increased from six cases during pre-delta period to 66 cases during omicron period, while the incidence rate (the number of MIS-C cases per 100,000 cases of reported coronavirus disease 2019) has decreased from 38.5 cases per 100,000 (95% confidence interval [CI], 14.1–83.9) during pre-delta period to 1.6 cases per 100,000 (95% CI, 1.2–2.0) during omicron periods. During pre-delta period, 66.7% and 100% had hypotension and gastrointestinal involvement, respectively; while during omicron period, 12.1% and 6.1% had such clinical manifestations. Fifty percent of pre-delta MIS-C patients were taken intensive care unit (ICU) cares, while 10.6% of patients during omicron periods were in ICUs.
Conclusion
Omicron period were associated with less severe clinical manifestation compared to pre-delta and delta periods. Although incidence rate of MIS-C was lower for the omicron period than pre-delta and delta periods, number of patients reported with MIS-C may pose a substantial clinical burden.
Keyword
Figure
Reference
-
1. Karim SS, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021; 398(10317):2126–2128. PMID: 34871545.2. Belot A, Antona D, Renolleau S, Javouhey E, Hentgen V, Angoulvant F, et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Euro Surveill. 2020; 25(22):2001010. PMID: 32524957.3. Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020; 369:m2094. PMID: 32493739.4. Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020; 395(10239):1771–1778. PMID: 32410760.5. Nygaard U, Holm M, Hartling UB, Glenthøj J, Schmidt LS, Nordly SB, et al. Incidence and clinical phenotype of multisystem inflammatory syndrome in children after infection with the SARS-CoV-2 delta variant by vaccination status: a Danish nationwide prospective cohort study. Lancet Child Adolesc Health. 2022; 6(7):459–465. PMID: 35526537.6. Payne AB, Gilani Z, Godfred-Cato S, Belay ED, Feldstein LR, Patel MM, et al. Incidence of multisystem inflammatory syndrome in children among US persons infected with SARS-CoV-2. JAMA Netw Open. 2021; 4(6):e2116420. PMID: 34110391.7. Yousaf AR, Cortese MM, Taylor AW, Broder KR, Oster ME, Wong JM, et al. Reported cases of multisystem inflammatory syndrome in children aged 12-20 years in the USA who received a COVID-19 vaccine, December, 2020, through August, 2021: a surveillance investigation. Lancet Child Adolesc Health. 2022; 6(5):303–312. PMID: 35216660.8. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MB, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020; 383(4):334–346. PMID: 32598831.9. Cohen JM, Carter MJ, Ronny Cheung C, Ladhani S. Evelina Paediatric Inflammatory Multisystem Syndrome Temporally related to SARS-CoV-2 (PIMS-TS) Study Group. Lower risk of multisystem inflammatory syndrome in children with the delta and omicron variants of severe acute respiratory syndrome coronavirus 2. Clin Infect Dis. 2023; 76(3):e518–e521. PMID: 35788276.10. Holm M, Espenhain L, Glenthøj J, Schmidt LS, Nordly SB, Hartling UB, et al. Risk and phenotype of multisystem inflammatory syndrome in vaccinated and unvaccinated Danish children before and during the omicron wave. JAMA Pediatr. 2022; 176(8):821–823. PMID: 35675054.11. Levy N, Koppel JH, Kaplan O, Yechiam H, Shahar-Nissan K, Cohen NK, et al. Severity and incidence of multisystem inflammatory syndrome in children during 3 SARS-CoV-2 pandemic waves in Israel. JAMA. 2022; 327(24):2452–2454. PMID: 35588048.12. Li W, Tang Y, Shi Y, Chen Y, Liu E. Why multisystem inflammatory syndrome in children has been less commonly described in Asia? Transl Pediatr. 2020; 9(6):873–875. PMID: 33457311.13. Torjesen I. Covid-19: omicron variant is linked to steep rise in hospital admissions of very young children. BMJ. 2022; 376:o110. PMID: 35031537.14. Kang S, Kim Y, Kim J. An analysis of the policy participation of field response nurses in South Korea: COVID-19 response guidelines and the infectious disease act revision. J Nurs Scholarsh. 2023; 55(1):202–214. PMID: 36480159.15. Lee H, Choi EH, Park YJ, Choe YJ. Short term impact of coronavirus disease 2019 vaccination in children in Korea. J Korean Med Sci. 2022; 37(17):e124. PMID: 35502499.16. Jang EJ, Choe YJ, Kim RK, Park YJ. BNT162b2 vaccine effectiveness against the SARS-CoV-2 omicron variant in children aged 5 to 11 years. JAMA Pediatr. 2023; 177(3):319–320. PMID: 36622683.17. Choe YJ, Choi EH, Choi JW, Eun BW, Eun LY, Kim YJ, et al. Surveillance of COVID-19-associated multisystem inflammatory syndrome in children, South Korea. Emerg Infect Dis. 2021; 27(4):1196–1200. PMID: 33539720.18. Kim EY, Choe YJ, Park H, Jeong H, Chung JH, Yu J, et al. Community transmission of SARS-CoV-2 omicron variant, South Korea, 2021. Emerg Infect Dis. 2022; 28(4):898–900. PMID: 35171760.19. Lopez L, Burgner D, Glover C, Carr J, Clark J, Boast A, et al. Lower risk of multi-system inflammatory syndrome in children (MIS-C) with the omicron variant. Lancet Reg Health West Pac. 2022; 27:100604. PMID: 36237982.20. Kenney PO, Chang AJ, Krabill L, Hicar MD. decreased clinical severity of pediatric acute COVID-19 and MIS-C and increase of incidental cases during the omicron wave in comparison to the delta wave. Viruses. 2023; 15(1):180. PMID: 36680220.21. Garcia-Beltran WF, Lam EC, Astudillo MG, Yang D, Miller TE, Feldman J, et al. COVID-19-neutralizing antibodies predict disease severity and survival. Cell. 2021; 184(2):476–488.e11. PMID: 33412089.22. Imai K, Kitagawa Y, Tabata S, Kubota K, Nagura-Ikeda M, Matsuoka M, et al. Antibody response patterns in COVID-19 patients with different levels of disease severity in Japan. J Med Virol. 2021; 93(5):3211–3218. PMID: 33620098.23. Kim YJ, Bae JY, Bae S, Hwang S, Kwon KT, Chang HH, et al. Neutralizing antibody responses to SARS-CoV-2 in Korean patients who have recovered from COVID-19. Yonsei Med J. 2021; 62(7):584–592. PMID: 34164955.24. Middelburg JG, Crijnen TE, D’Antiga L, Verdoni L, Chikermane A, Garg P, et al. Association of ethnicity with multisystem inflammatory syndrome in children related to SARS-CoV-2 infection: an international case-referent study. Front Pediatr. 2021; 9:707650. PMID: 34722416.25. Stierman B, Abrams JY, Godfred-Cato SE, Oster ME, Meng L, Yip L, et al. Racial and ethnic disparities in multisystem inflammatory syndrome in children in the United States, March 2020 to February 2021. Pediatr Infect Dis J. 2021; 40(11):e400–e406. PMID: 34382615.26. Moorthy GS, Smith MJ, Staples BB. Coronavirus disease 2019 vaccine in children. Pediatr Rev. 2021; 42(10):576–578. PMID: 34599060.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe SARS-CoV-2 Infection With Multiorgan Involvement Followed by MIS-C in an Adolescent
- Occurrence of Norovirus GII.4 Sydney Variant-related Outbreaks in Korea
- Epidemics of Norovirus GII.4 Variant in Outbreak Cases in Korea, 2004–2012
- Current Application of Minimally Invasive Surgery for Gastrointestinal Diseases
- Comparison of COVID-19-associated multisystem inflammatory syndrome in children (MIS-C) and Kawasaki disease shock syndrome: case reports and literature review