Clin Endosc.
2023 Jul;56(4):433-445. 10.5946/ce.2023.013.
Endoscopic retrograde cholangiopancreatography-related complications: risk stratification, prevention, and management
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore
- 2Duke-NUS Medical School, Singapore
- KMID: 2544564
- DOI: http://doi.org/10.5946/ce.2023.013
Abstract
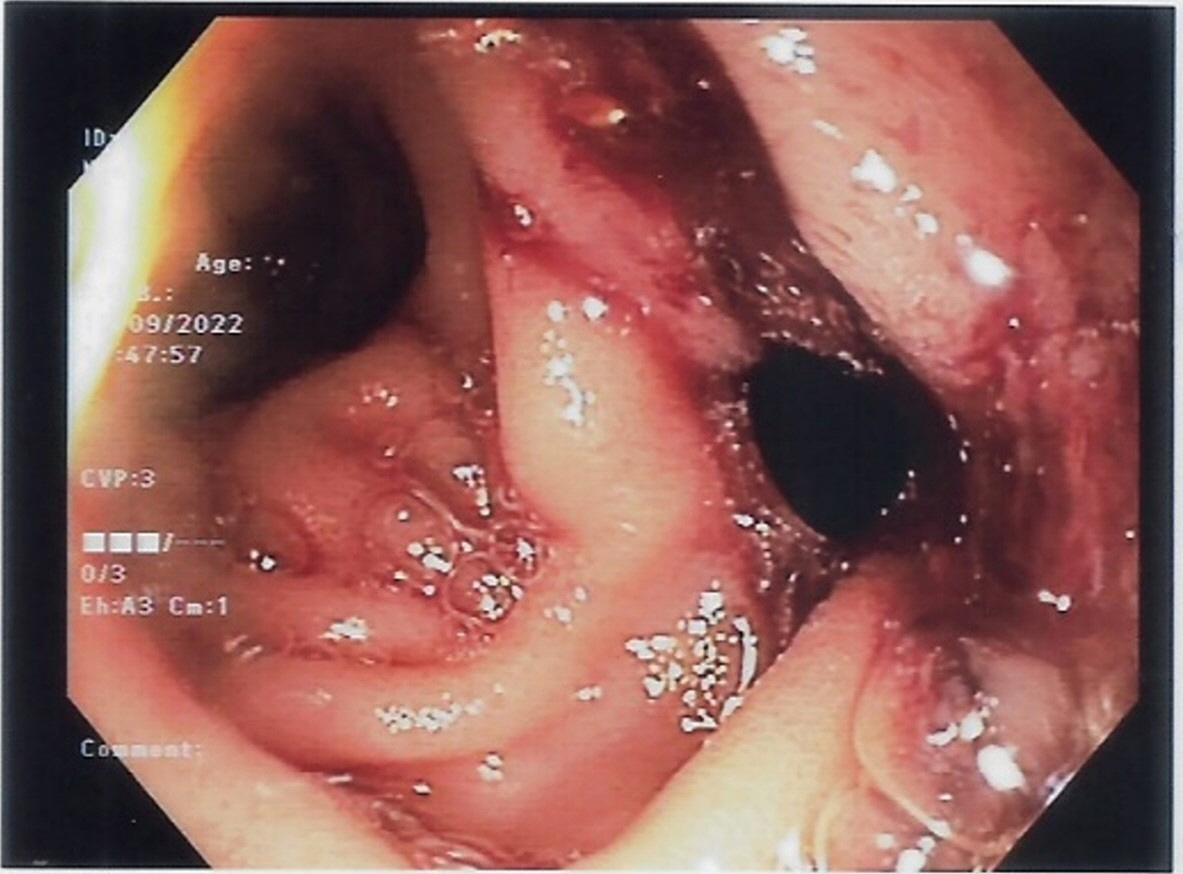
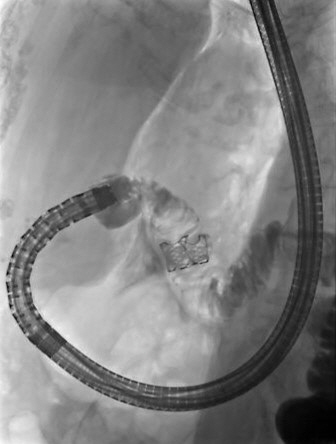
- Endoscopic retrograde cholangiopancreatography (ERCP) plays a crucial role in the management of pancreaticobiliary disorders. Although the ERCP technique has been refined over the past five decades, it remains one of the endoscopic procedures with the highest rate of complications. Risk factors for ERCP-related complications are broadly classified into patient-, procedure-, and operator-related risk factors. Although non-modifiable, patient-related risk factors allow for the closer monitoring and instatement of preventive measures. Post-ERCP pancreatitis is the most common complication of ERCP. Risk reduction strategies include intravenous hydration, rectal nonsteroidal anti-inflammatory drugs, and pancreatic stent placement in selected patients. Perforation is associated with significant morbidity and mortality, and prompt recognition and treatment of ERCP-related perforations are key to ensuring good clinical outcomes. Endoscopy plays an expanding role in the treatment of perforations. Specific management strategies depend on the location of the perforation and the patient’s clinical status. The risk of post-ERCP bleeding can be attenuated by preprocedural optimization and adoption of intra-procedural techniques. Endoscopic measures are the mainstay of management for post-ERCP bleeding. Escalation to angioembolization or surgery may be required for refractory bleeding. Post-ERCP cholangitis can be reduced with antibiotic prophylaxis in high risk patients. Bile culture-directed therapy plays an important role in antimicrobial treatment.
Keyword
Figure
Reference
-
1. Cappell MS, Friedel DM. Stricter national standards are required for credentialing of endoscopic-retrograde-cholangiopancreatography in the United States. World J Gastroenterol. 2019; 25:3468–3483.2. Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020; 52:127–149.3. ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017; 85:32–47.4. Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102:1781–1788.5. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.6. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013; 62:102–111.7. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001; 54:425–434.8. Inamdar S, Berzin TM, Sejpal DV, et al. Pregnancy is a risk factor for pancreatitis after endoscopic retrograde cholangiopancreatography in a national cohort study. Clin Gastroenterol Hepatol. 2016; 14:107–114.9. Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006; 101:139–147.10. Masci E, Mariani A, Curioni S, et al. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003; 35:830–834.11. Cennamo V, Fuccio L, Zagari RM, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk?: meta-analysis of randomized controlled trials. Endoscopy. 2010; 42:381–388.12. Itoi T, Yasuda I, Doi S, et al. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011; 43:369–372.13. Dumonceau JM, Andriulli A, Elmunzer BJ, et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline: updated June 2014. Endoscopy. 2014; 46:799–815.14. Harewood GC, Pochron NL, Gostout CJ. Prospective, randomized, controlled trial of prophylactic pancreatic stent placement for endoscopic snare excision of the duodenal ampulla. Gastrointest Endosc. 2005; 62:367–370.15. Syrén EL, Sandblom G, Enochsson L, et al. Outcome of ERCP related to case-volume. Surg Endosc. 2022; 36:5339–5347.16. Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012; 366:1414–1422.17. Ishiwatari H, Urata T, Yasuda I, et al. No benefit of oral diclofenac on post-endoscopic retrograde cholangiopancreatography pancreatitis. Dig Dis Sci. 2016; 61:3292–3301.18. Kato K, Shiba M, Kakiya Y, et al. Celecoxib oral administration for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: a randomized prospective trial. Pancreas. 2017; 46:880–886.19. Staritz M, Poralla T, Ewe K, et al. Effect of glyceryl trinitrate on the sphincter of Oddi motility and baseline pressure. Gut. 1985; 26:194–197.20. Wehrmann T, Schmitt T, Stergiou N, et al. Topical application of nitrates onto the papilla of Vater: manometric and clinical results. Endoscopy. 2001; 33:323–328.21. Bai Y, Xu C, Yang X, et al. Glyceryl trinitrate for prevention of pancreatitis after endoscopic retrograde cholangiopancreatography: a meta-analysis of randomized, double-blind, placebo-controlled trials. Endoscopy. 2009; 41:690–695.22. Sotoudehmanesh R, Eloubeidi MA, Asgari AA, et al. A randomized trial of rectal indomethacin and sublingual nitrates to prevent post-ERCP pancreatitis. Am J Gastroenterol. 2014; 109:903–909.23. Tomoda T, Kato H, Ueki T, et al. Combination of diclofenac and sublingual nitrates is superior to diclofenac alone in preventing pancreatitis after endoscopic retrograde cholangiopancreatography. Gastroenterology. 2019; 156:1753–1760.24. Wu M, Jiang S, Lu X, et al. Aggressive hydration with lactated ringer solution in prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. Medicine (Baltimore). 2021; 100:e25598.25. Sperna Weiland CJ, Engels MM, et al. Increased use of prophylactic measures in preventing post-endoscopic retrograde cholangiopancreatography pancreatitis. Dig Dis Sci. 2021; 66:4457–4466.26. Tarnasky PR, Palesch YY, Cunningham JT, et al. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology. 1998; 115:1518–1524.27. Fan JH, Qian JB, Wang YM, et al. Updated meta-analysis of pancreatic stent placement in preventing post-endoscopic retrograde cholangiopancreatography pancreatitis. World J Gastroenterol. 2015; 21:7577–7583.28. Ito K, Fujita N, Noda Y, et al. Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation?: a prospective randomized controlled trial. J Gastroenterol. 2010; 45:1183–1191.29. Tse F, Yuan Y, Bukhari M, et al. Pancreatic duct guidewire placement for biliary cannulation for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2016; (5):CD010571.30. Freeman ML, Overby C, Qi D. Pancreatic stent insertion: consequences of failure and results of a modified technique to maximize success. Gastrointest Endosc. 2004; 59:8–14.31. Tse F, Liu J, Yuan Y, et al. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2022; 3(3):CD009662.32. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.33. Cirocchi R, Kelly MD, Griffiths EA, et al. A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system. Surgeon. 2017; 15:379–387.34. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298.35. Kumbhari V, Sinha A, Reddy A, et al. Algorithm for the management of ERCP-related perforations. Gastrointest Endosc. 2016; 83:934–943.36. Langerth A, Isaksson B, Karlson BM, et al. ERCP-related perforations: a population-based study of incidence, mortality, and risk factors. Surg Endosc. 2020; 34:1939–1947.37. Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000; 232:191–198.38. Parlak E, Köksal A, Dişibeyaz S, et al. Endoscopic closure of ERCP-related duodenal perforations by using endoclips: a case series. Surg Laparosc Endosc Percutan Tech. 2013; 23:e225–e228.39. Tyberg A, Zerbo S, Sharaiha RZ, et al. Endoscopic management of a GI perforation. Gastrointest Endosc. 2015; 82:955.40. Khater S, Rahmi G, Perrod G, et al. Over-the-scope clip (OTSC) reduces surgery rate in the management of iatrogenic gastrointestinal perforations. Endosc Int Open. 2017; 5:E389–E394.41. Hyun JJ, Kozarek RA, Irani SS. Endoscopic suturing of a large type I duodenal perforation. VideoGIE. 2018; 4:78–80.42. Zhang LY, Bejjani M, Ghandour B, et al. Endoscopic through-the-scope suturing. VideoGIE. 2021; 7:46–51.43. Patil NS, Solanki N, Mishra PK, et al. ERCP-related perforation: an analysis of operative outcomes in a large series over 12 years. Surg Endosc. 2020; 34:77–87.44. Vezakis A, Fragulidis G, Polydorou A. Endoscopic retrograde cholangiopancreatography-related perforations: diagnosis and management. World J Gastrointest Endosc. 2015; 7:1135–1141.45. Odemis B, Oztas E, Kuzu UB, et al. Can a fully covered self-expandable metallic stent be used temporarily for the management of duodenal retroperitoneal perforation during ERCP as a part of conservative therapy? Surg Laparosc Endosc Percutan Tech. 2016; 26:e9–e17.46. Theopistos V, Theocharis G, Konstantakis C, et al. Non-operative management of type 2 ERCP-related retroperitoneal duodenal perforations: a 9-year experience from a single center. Gastroenterology Res. 2018; 11:207–212.47. Arvanitakis M, Dumonceau JM, Albert J, et al. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines. Endoscopy. 2018; 50:524–546.48. Paspatis GA, Arvanitakis M, Dumonceau JM, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) position statement: update 2020. Endoscopy. 2020; 52:792–810.49. Mashiana HS, Dhaliwal AS, Sayles H, et al. Endoscopic retrograde cholangiopancreatography in cirrhosis - a systematic review and meta-analysis focused on adverse events. World J Gastrointest Endosc. 2018; 10:354–366.50. Kim JY, Lee HS, Chung MJ, et al. Bleeding complications and clinical safety of endoscopic retrograde cholangiopancreatography in patients with liver cirrhosis. Yonsei Med J. 2019; 60:440–445.51. Oh HC, El Hajj II, Easler JJ, et al. Post-ERCP bleeding in the era of multiple antiplatelet agents. Gut Liver. 2018; 12:214–218.52. Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021; 70:1611–1628.53. Parras Castañera E, Rodríguez López P, Álvarez A, et al. Predictive factors for post-ERCP bleeding: influence of direct oral anticoagulants. Rev Esp Enferm Dig. 2021; 113:591–596.54. Nakaji S, Hirata N, Matsui H, et al. Hemodialysis is a strong risk factor for post-endoscopic sphincterotomy bleeding in patients with choledocholithiasis. Endosc Int Open. 2018; 6:E568–E574.55. Bae SS, Lee DW, Han J, et al. Risk factor of bleeding after endoscopic sphincterotomy in average risk patients. Surg Endosc. 2019; 33:3334–3340.56. Lee HJ, Cho CM, Heo J, et al. Impact of hospital volume and the experience of endoscopist on adverse events related to endoscopic retrograde cholangiopancreatography: a prospective observational study. Gut Liver. 2020; 14:257–264.57. ASGE Standards of Practice Committee, Acosta RD, Abraham NS, et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016; 83:3–16.58. Feng Y, Zhu H, Chen X, et al. Comparison of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for retrieval of choledocholithiasis: a meta-analysis of randomized controlled trials. J Gastroenterol. 2012; 47:655–663.59. Mirjalili SA, Stringer MD. The arterial supply of the major duodenal papilla and its relevance to endoscopic sphincterotomy. Endoscopy. 2011; 43:307–311.60. Wilcox CM, Canakis J, Mönkemüller KE, et al. Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol. 2004; 99:244–248.61. Liu F, Wang GY, Li ZS. Cap-assisted hemoclip application with forward-viewing endoscope for hemorrhage induced by endoscopic sphincterotomy: a prospective case series study. BMC Gastroenterol. 2015; 15:135.62. Aranez JL, Miller J, Hughes M, et al. A novel, duodenoscope-friendly endoscopic clip for treating massive upper-GI bleeding secondary to a Dieulafoy lesion. VideoGIE. 2018; 3:205–206.63. Bilal M, Chandnani M, McDonald NM, et al. Use of fully covered self-expanding metal biliary stents for managing endoscopic biliary sphincterotomy related bleeding. Endosc Int Open. 2021; 9:E667–E673.64. Dunne R, McCarthy E, Joyce E, et al. Post-endoscopic biliary sphincterotomy bleeding: an interventional radiology approach. Acta Radiol. 2013; 54:1159–1164.65. ASGE Standards of Practice Committee, Khashab MA, Chithadi KV, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2015; 81:81–89.66. Chen M, Wang L, Wang Y, et al. Risk factor analysis of post-ERCP cholangitis: a single-center experience. Hepatobiliary Pancreat Dis Int. 2018; 17:55–58.67. Navaneethan U, Jegadeesan R, Nayak S, et al. ERCP-related adverse events in patients with primary sclerosing cholangitis. Gastrointest Endosc. 2015; 81:410–419.68. Othman MO, Guerrero R, Elhanafi S, et al. A prospective study of the risk of bacteremia in directed cholangioscopic examination of the common bile duct. Gastrointest Endosc. 2016; 83:151–157.69. Sethi A, Chen YK, Austin GL, et al. ERCP with cholangiopancreatoscopy may be associated with higher rates of complications than ERCP alone: a single-center experience. Gastrointest Endosc. 2011; 73:251–256.70. Harris A, Chan AC, Torres-Viera C, et al. Meta-analysis of antibiotic prophylaxis in endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy. 1999; 31:718–724.71. Brand M, Bizos D, O’Farrell P Jr. Antibiotic prophylaxis for patients undergoing elective endoscopic retrograde cholangiopancreatography. Cochrane Database Syst Rev. 2010; (10):CD007345.72. Kager LM, Sjouke B, van den Brand M, et al. The role of antibiotic prophylaxis in endoscopic retrograde cholangiopancreatography; a retrospective single-center evaluation. Scand J Gastroenterol. 2012; 47:245–250.73. Tonolini M, Pagani A, Bianco R. Cross-sectional imaging of common and unusual complications after endoscopic retrograde cholangiopancreatography. Insights Imaging. 2015; 6:323–338.74. Chandra S, Klair JS, Soota K, et al. Endoscopic retrograde cholangio-pancreatography-obtained bile culture can guide antibiotic therapy in acute cholangitis. Dig Dis. 2019; 37:155–160.75. Negm AA, Schott A, Vonberg RP, et al. Routine bile collection for microbiological analysis during cholangiography and its impact on the management of cholangitis. Gastrointest Endosc. 2010; 72:284–291.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
- Prevention and Management of Post-Endoscopic Retrograde Cholangiopancreatography Complications
- Basic knowledge of endoscopic retrograde cholangiopancreatography
- Preparation of High-Risk Patients and the Choice of Guidewire for a Successful Endoscopic Retrograde Cholangiopancreatography Procedure
- The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation