J Korean Med Sci.
2023 Jul;38(28):e210. 10.3346/jkms.2023.38.e210.
Risk Factors for the Occurrence and Severity of Vertebral Fractures in Inflammatory Bowel Disease Patients: A Nationwide Population-Based Cohort Study
- Affiliations
-
- 1Department of Preventive Medicine and Public Health, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Orthopedic Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2544472
- DOI: http://doi.org/10.3346/jkms.2023.38.e210
Abstract
- Background
The risk of vertebral fractures is increased in inflammatory bowel disease (IBD) patients. However, whether the severity of vertebral fractures differs between IBD patients and the general population, or between patients with Crohn’s disease (CD) and ulcerative colitis (UC), is unknown.
Methods
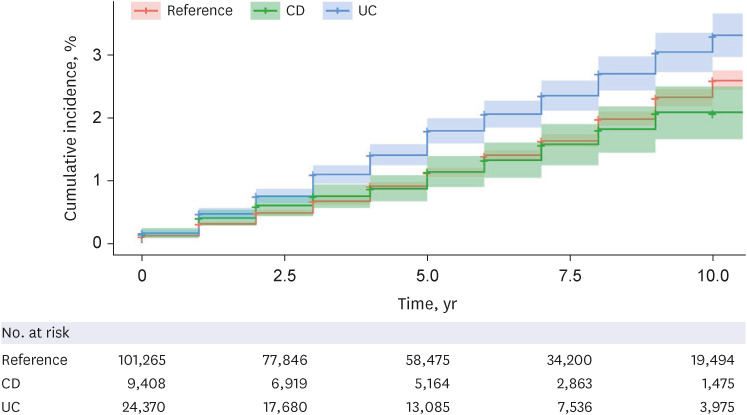
We investigated risk factors associated with the occurrence and severity of vertebral fractures in IBD patients using The National Healthcare Insurance Service (NHIS) database. We defined the patients who underwent vertebroplasty or kyphoplasty after being diagnosed with a vertebral fracture as having a severe vertebral fracture than those with only diagnosis codes.
Results
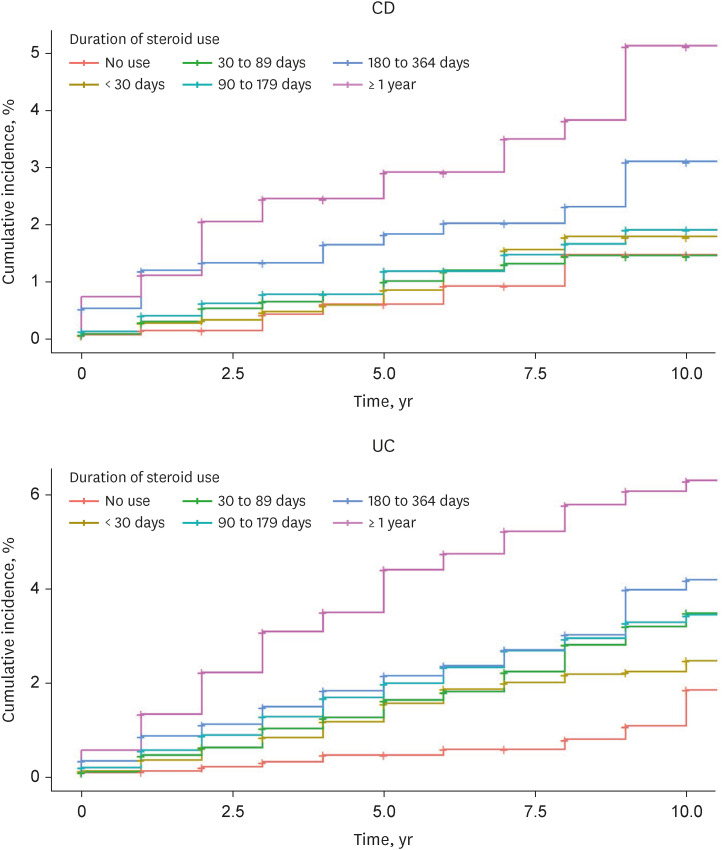
From 2008 to 2018, there were 33,778 patients with IBD (24,370 UC patients and 9,408 CD patients) and 101,265 patients in the reference population. The incidence rate ratio of vertebral fractures in the IBD patients was 1.27 per 1,000 person-years (95% confidence interval [CI], 1.26–1.27). The risk of vertebral fracture was higher in CD and UC patients than in the matched reference group (hazard ratio [HR], 1.59; 95% CI, 1.31–1.92; P < 0.001 and HR, 1.26; 95% CI, 1.14–1.41; P < 0.001, respectively). In a multivariate analysis, the occurrence of vertebral fracture was associated with CD (HR, 1.31; 95% CI, 1.08–1.59; P = 0.006), older age (CD: HR, 1.09; 95% CI, 1.08–1.09; P < 0.001 and UC: HR, 1.09; 95% CI, 1.08–1.09; P < 0.001), female sex (CD: HR, 1.81; 95% CI, 1.63–2.01; P < 0.001 and UC: HR, 2.02; 95% CI, 1.83–2.22; P < 0.001), high Charlson Comorbidity Index (CCI) score (CD: HR, 1.42; 95% CI, 1.23–1.63; P < 0.001 and UC: HR, 1.46; 95% CI, 1.29–1.65, P < 0.001), and long-term steroid use (CD:HR, 3.71; 95% CI, 2.84–3.37; P < 0.001 and UC: HR, 3.88; 95% CI, 3.07–4.91; P < 0.001). The severity of vertebral fractures was associated with IBD (CD: HR, 1.82; 95% CI, 1.17–2.83; P = 0.008 and UC: HR, 1.49; 95% CI, 1.17–1.89; P < 0.001) and older age (HR, 1.06; 95% CI, 1.05–1.07; P < 0.001).
Conclusion
Vertebral fractures occur frequently and more severely in IBD patients, particularly those with CD. Therefore, we suggest monitoring of bone density, regular vitamin D supply, and reducing the use of corticosteroids to prevent vertebral fractures in IBD patients who are older, female, or have comorbidities.
Keyword
Figure
Reference
-
1. Kendler DL, Bauer DC, Davison KS, Dian L, Hanley DA, Harris ST, et al. Vertebral fractures: clinical importance and management. Am J Med. 2016; 129(2):221.e1–221.10.2. Goldstein CL, Chutkan NB, Choma TJ, Orr RD. Management of the elderly with vertebral compression fractures. Neurosurgery. 2015; 77(Suppl 4):S33–S45. PMID: 26378356.3. Kim HY, Ha YC, Kim TY, Cho H, Lee YK, Baek JY, et al. Healthcare costs of osteoporotic fracture in Korea: information from the National Health Insurance claims database, 2008-2011. J Bone Metab. 2017; 24(2):125–133. PMID: 28642857.4. Dewar C. Diagnosis and treatment of vertebral compression fractures. Radiol Technol. 2015; 86(3):301–320. PMID: 25739109.5. Emkey GR, Epstein S. Secondary osteoporosis: pathophysiology & diagnosis. Best Pract Res Clin Endocrinol Metab. 2014; 28(6):911–935. PMID: 25432361.6. Guan Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. 2019; 2019:7247238. PMID: 31886308.7. Filippi J, Al-Jaouni R, Wiroth JB, Hébuterne X, Schneider SM. Nutritional deficiencies in patients with Crohn’s disease in remission. Inflamm Bowel Dis. 2006; 12(3):185–191. PMID: 16534419.8. Bischoff SC, Herrmann A, Göke M, Manns MP, von zur Mühlen A, Brabant G. Altered bone metabolism in inflammatory bowel disease. Am J Gastroenterol. 1997; 92(7):1157–1163. PMID: 9219790.9. Faye AS, Colombel JF. Aging and IBD: a new challenge for clinicians and researchers. Inflamm Bowel Dis. 2022; 28(1):126–132. PMID: 33904578.10. Ahn HJ, Kim YJ, Lee HS, Park JH, Hwang SW, Yang DH, et al. High risk of fractures within 7 years of diagnosis in Asian patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2022; 20(5):e1022–e1039. PMID: 34216823.11. van Staa TP, Cooper C, Brusse LS, Leufkens H, Javaid MK, Arden NK. Inflammatory bowel disease and the risk of fracture. Gastroenterology. 2003; 125(6):1591–1597. PMID: 14724810.12. Ludvigsson JF, Mahl M, Sachs MC, Björk J, Michaelsson K, Ekbom A, et al. Fracture risk in patients with inflammatory bowel disease: a nationwide population-based cohort study from 1964 to 2014. Am J Gastroenterol. 2019; 114(2):291–304. PMID: 30730858.13. Klaus J, Armbrecht G, Steinkamp M, Brückel J, Rieber A, Adler G, et al. High prevalence of osteoporotic vertebral fractures in patients with Crohn’s disease. Gut. 2002; 51(5):654–658. PMID: 12377802.14. Card T, West J, Hubbard R, Logan RF. Hip fractures in patients with inflammatory bowel disease and their relationship to corticosteroid use: a population based cohort study. Gut. 2004; 53(2):251–255. PMID: 14724159.15. Ghishan FK, Kiela PR. Advances in the understanding of mineral and bone metabolism in inflammatory bowel diseases. Am J Physiol Gastrointest Liver Physiol. 2011; 300(2):G191–G201. PMID: 21088237.16. Tsai MS, Lin CL, Tu YK, Lee PH, Kao CH. Risks and predictors of osteoporosis in patients with inflammatory bowel diseases in an Asian population: a nationwide population-based cohort study. Int J Clin Pract. 2015; 69(2):235–241. PMID: 25472555.17. van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int. 2002; 13(10):777–787. PMID: 12378366.18. Buckley L, Humphrey MB. Glucocorticoid-Induced Osteoporosis. N Engl J Med. 2018; 379(26):2547–2556. PMID: 30586507.19. Komaki Y, Komaki F, Micic D, Ido A, Sakuraba A. Risk of fractures in inflammatory bowel diseases: a systematic review and meta-analysis. J Clin Gastroenterol. 2019; 53(6):441–448. PMID: 29672437.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fracture Risk in Middle-Aged and Older Patients With Inflammatory Bowel Disease: A Korean Nationwide Population-Based Cohort Study
- Association between nonalcoholic fatty liver disease and incidence of inflammatory bowel disease: a nationwide population‑based cohort study
- Venous Thromboembolism Risk in Asian Patients with Inflammatory Bowel Disease: A Population-Based Nationwide Inception Cohort Study
- Treatment Goals for Prevention of Vertebral Fractures in Patients with Rheumatoid Arthritis
- Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea