Cancer Res Treat.
2023 Jul;55(3):1053-1057. 10.4143/crt.2022.1535.
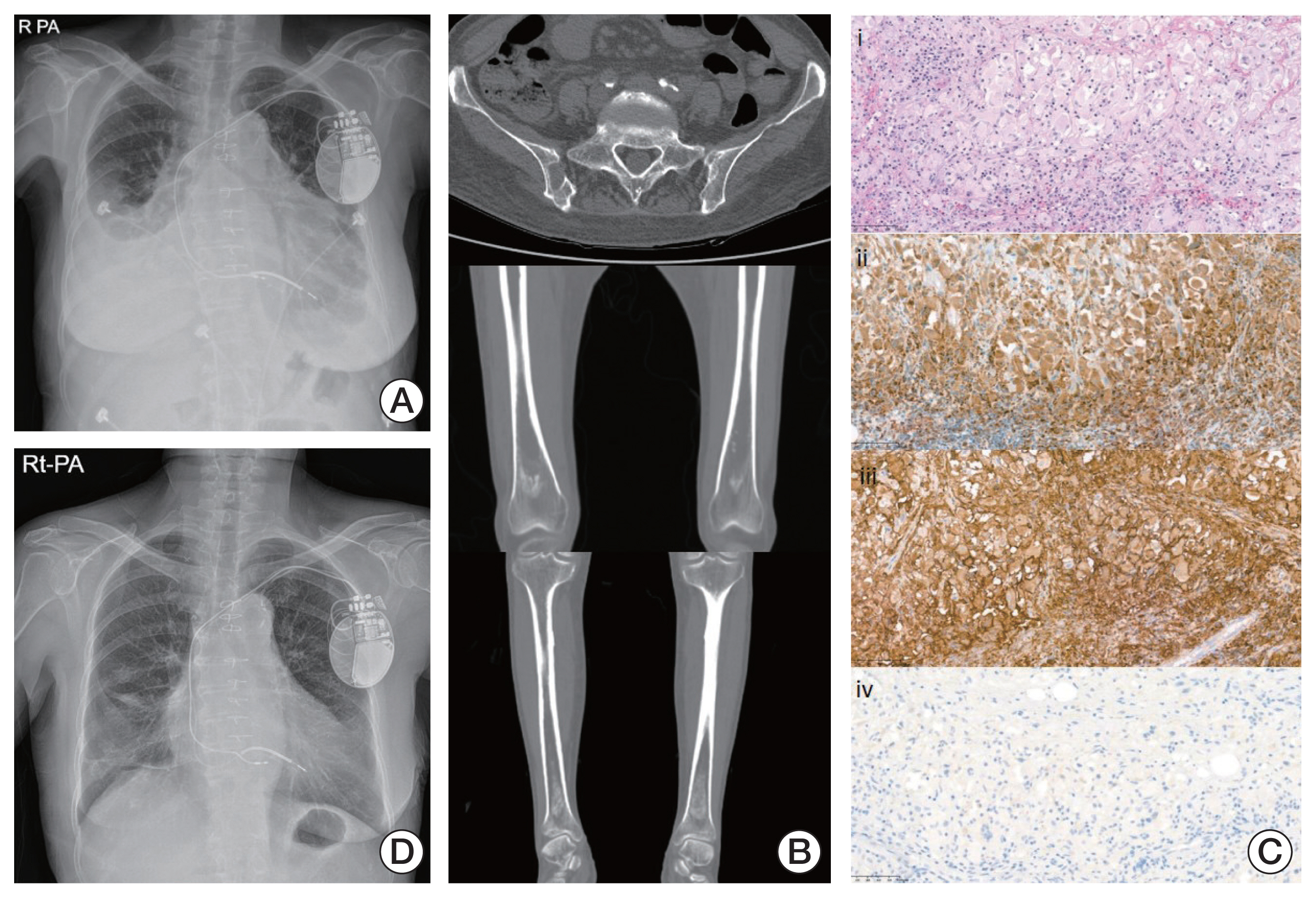
Case Report of Erdheim-Chester Disease Successfully Treated with Pegylated Interferon: A Single-Center Experience
- Affiliations
-
- 1Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2544185
- DOI: http://doi.org/10.4143/crt.2022.1535
Abstract
- Erdheim-Chester disease (ECD), also known as non-Langerhans cell histiocytosis, is a multi-systemic disease with unclear pathogenesis. Based on a small number of case studies, pegylated interferon-α (PEG-IFN-α) has been used as the front-line treatment option. However, there are limited data regarding administration of ropegylated-interferon α-2b (ROPEG-IFN-α 2b) for ECD patients. Herein, we report two cases of severe ECD treated with two types of PEG-IFN-α. One patient with heart and skeleton involvement and BRAF V600E mutation was treated with weekly PEG-IFN-α 2a. Another patient with bone involvement and no BRAF V600E mutation was administered monthly ROPEG-IFN-α 2b. The two types of PEG-IFN-α showed excellent disease control, excellent survival outcomes, and manageable toxicities in ECD patients. These results suggest that ROPEG-IFN-α 2b could be used equivalently to PEG-IFN-α 2a for management of advanced ECD.
Keyword
Figure
Reference
-
References
1. Arnaud L, Hervier B, Neel A, Hamidou MA, Kahn JE, Wechsler B, et al. CNS involvement and treatment with interferon-alpha are independent prognostic factors in Erdheim-Chester disease: a multicenter survival analysis of 53 patients. Blood. 2011; 117:2778–82.2. Munoz J, Janku F, Cohen PR, Kurzrock R. Erdheim-Chester disease: characteristics and management. Mayo Clin Proc. 2014; 89:985–96.
Article3. Vassallo R, Ryu JH, Schroeder DR, Decker PA, Limper AH. Clinical outcomes of pulmonary Langerhans’-cell histiocytosis in adults. N Engl J Med. 2002; 346:484–90.
Article4. Haroche J, Charlotte F, Arnaud L, von Deimling A, Helias-Rodzewicz Z, Hervier B, et al. High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. Blood. 2012; 120:2700–3.
Article5. Diamond EL, Dagna L, Hyman DM, Cavalli G, Janku F, Estrada-Veras J, et al. Consensus guidelines for the diagnosis and clinical management of Erdheim-Chester disease. Blood. 2014; 124:483–92.
Article6. Arnaud L, Gorochov G, Charlotte F, Lvovschi V, Parizot C, Larsen M, et al. Systemic perturbation of cytokine and chemokine networks in Erdheim-Chester disease: a single-center series of 37 patients. Blood. 2011; 117:2783–90.
Article7. Dagna L, Corti A, Langheim S, Guglielmi B, De Cobelli F, Doglioni C, et al. Tumor necrosis factor alpha as a master regulator of inflammation in Erdheim-Chester disease: rationale for the treatment of patients with infliximab. J Clin Oncol. 2012; 30:e286–90.8. Stoppacciaro A, Ferrarini M, Salmaggi C, Colarossi C, Praderio L, Tresoldi M, et al. Immunohistochemical evidence of a cytokine and chemokine network in three patients with Erdheim-Chester disease: implications for pathogenesis. Arthritis Rheum. 2006; 54:4018–22.
Article9. Mossetti G, Rendina D, Numis FG, Somma P, Postiglione L, Nunziata V. Biochemical markers of bone turnover, serum levels of interleukin-6/interleukin-6 soluble receptor and bisphosphonate treatment in Erdheim-Chester disease. Clin Exp Rheumatol. 2003; 21:232–6.10. Braiteh F, Boxrud C, Esmaeli B, Kurzrock R. Successful treatment of Erdheim-Chester disease, a non-Langerhans-cell histiocytosis, with interferon-alpha. Blood. 2005; 106:2992–4.11. Gisslinger H, Klade C, Georgiev P, Krochmalczyk D, Gercheva-Kyuchukova L, Egyed M, et al. Ropeginterferon alfa-2b versus standard therapy for polycythaemia vera (PROUD-PV and CONTINUATION-PV): a randomised, non-inferiority, phase 3 trial and its extension study. Lancet Haematol. 2020; 7:e196–208.12. Haroche J, Amoura Z, Trad SG, Wechsler B, Cluzel P, Grenier PA, et al. Variability in the efficacy of interferon-alpha in Erdheim-Chester disease by patient and site of involvement: results in eight patients. Arthritis Rheum. 2006; 54:3330–6.
Article13. Hervier B, Arnaud L, Charlotte F, Wechsler B, Piette JC, Amoura Z, et al. Treatment of Erdheim-Chester disease with long-term high-dose interferon-alpha. Semin Arthritis Rheum. 2012; 41:907–13.14. Goyal G, Shah MV, Call TG, Litzow MR, Hogan WJ, Go RS. Clinical and radiologic responses to cladribine for the treatment of Erdheim-Chester disease. JAMA Oncol. 2017; 3:1253–6.
Article15. Mazor RD, Manevich-Mazor M, Shoenfeld Y. Erdheim-Chester Disease: a comprehensive review of the literature. Orphanet J Rare Dis. 2013; 8:137.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erdheim-Chester Disease with Perirenal Masses Containing Macroscopic Fat Tissue
- Improvement of Erdheim-Chester disease-related renal failure after treatment with anakinra
- Successful Treatment of Erdheim-Chester Disease with Multisystemic Involvement in a 4-year-old Child by Interferon-α and Corticosteroid
- Commentary on "A Case of Erdheim-Chester Disease with Asymptomatic Renal Involvement"
- A Case of Erdheim-Chester Disease with Bilateral Hydronephrosis