Cancer Res Treat.
2023 Jul;55(3):707-719. 10.4143/crt.2022.1599.
Metastasis-Directed Local Therapy of Hepatic Oligometastasis from Colorectal Cancer and Future Perspective in Radiation Therapy
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Radiation Oncology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Department of Radiation Oncology, Chonnam National University Hwasun Hospital, Chonnam National University College of Medicine, Hwasun, Korea
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Surgery, St. Vincent`s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 6Department of Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Asan, Korea
- 7Department of Radiation Oncology, St. Vincent`s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2544155
- DOI: http://doi.org/10.4143/crt.2022.1599
Abstract
- Introduction
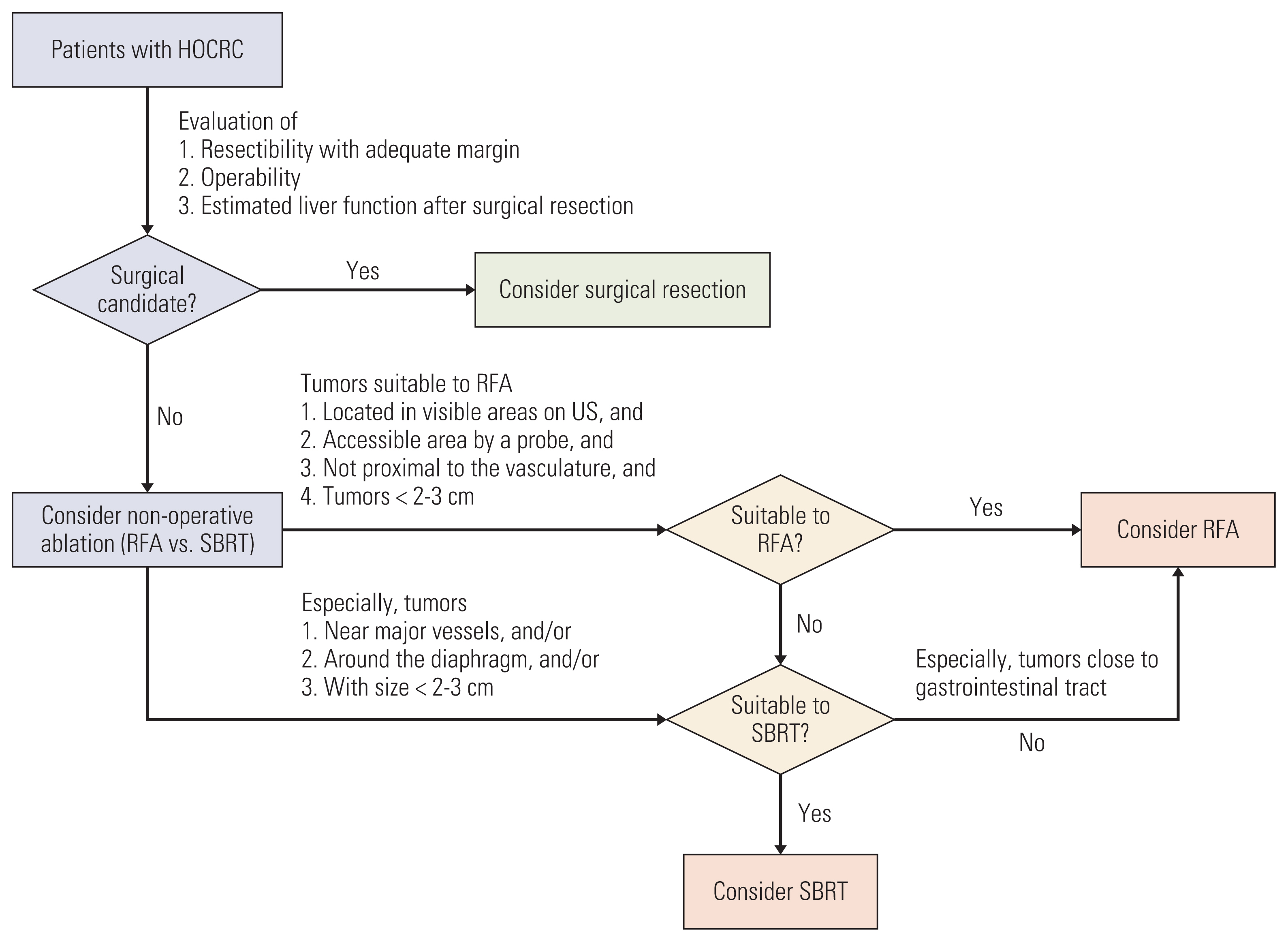
of the concept for oligometastasis led to wide application of metastasis-directed local ablative therapies for metastatic colorectal cancer (CRC). By application of the metastasis-directed local ablative therapies including surgical resection, radiofrequency ablation (RFA), and stereotactic ablative body radiotherapy (SABR), the survival outcomes of patients with metastatic CRC have improved. The liver is the most common distant metastatic site in CRC patients, and recently various metastasis-directed local therapies for hepatic oligometastasis from CRC (HOCRC) are widely used. Surgical resection is the first line of metastatic-directed local therapy for HOCRC, but its eligibility is very limited. Alternatively, RFA can be applied to patients who are ineligible for surgical resection of liver metastasis. However, there are some limitations such as inferior local control (LC) compared with surgical resection and technical feasibility based on location, size, and visibility on ultrasonography of the liver metastasis. Recent advances in radiation therapy technology have led to an increase in the use of SABR for liver tumors. SABR is considered complementary to RFA for patients with HOCRC who are ineligible for RFA. Furthermore, SABR can potentially result in better LC for liver metastases > 2-3 cm compared with RFA. In this article, the previous studies regarding curative metastasis-directed local therapies for HOCRC based on the radiation oncologist’s and surgeon’s perspective are reviewed and discussed. In addition, future perspectives regarding SABR in the treatment of HOCRC are suggested.
Figure
Reference
-
References
1. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995; 13:8–10.
Article2. Gadd MA, Casper ES, Woodruff JM, McCormack PM, Brennan MF. Development and treatment of pulmonary metastases in adult patients with extremity soft tissue sarcoma. Ann Surg. 1993; 218:705–12.
Article3. Hughes KS, Simon R, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery. 1986; 100:278–84.4. Nordlinger B, Vaillant JC, Guiguet M, Balladur P, Paris F, Bachellier P, et al. Survival benefit of repeat liver resections for recurrent colorectal metastases: 143 cases. Association Francaise de Chirurgie. J Clin Oncol. 1994; 12:1491–6.
Article5. Yoshino T, Arnold D, Taniguchi H, Pentheroudakis G, Yamazaki K, Xu RH, et al. Pan-Asian adapted ESMO consensus guidelines for the management of patients with metastatic colorectal cancer: a JSMO-ESMO initiative endorsed by CSCO, KACO, MOS, SSO and TOS. Ann Oncol. 2018; 29:44–70.
Article6. Rim CH, Cho WK, Lee JH, Kim YS, Suh YG, Kim KH, et al. Role of local treatment for oligometastasis: a comparability-based meta-analysis. Cancer Res Treat. 2022; 54:953–69.7. Yoo GS, Yu JI, Park W, Huh SJ, Choi DH. Prognostic factors in breast cancer with extracranial oligometastases and the appropriate role of radiation therapy. Radiat Oncol J. 2015; 33:301–9.8. Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol. 2020; 38:2830–8.
Article9. Nevens D, Jongen A, Kindts I, Billiet C, Deseyne P, Joye I, et al. Completeness of reporting oligometastatic disease characteristics in the literature and influence on oligometastatic disease classification using the ESTRO/EORTC nomenclature. Int J Radiat Oncol Biol Phys. 2022; 114:587–95.
Article10. Rao A, Vapiwala N, Schaeffer EM, Ryan CJ. Oligometastatic prostate cancer: a shrinking subset or an opportunity for cure? Am Soc Clin Oncol Educ Book. 2019; 39:309–20.
Article11. Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, deSouza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020; 21:e18–28.12. Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radia-tion oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020; 148:157–66.13. Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021; 14:101174.
Article14. National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer stat facts: colorectal cancer [Internet]. Bethesda, MD: National Cancer Institute;2022. [cited 2022 Jan 28]. Available from: https://seer.cancer.gov/statfacts/html/colorect.html .15. Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021; 325:669–85.16. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article17. Riihimaki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016; 6:29765.18. Rhu J, Heo JS, Choi SH, Choi DW, Kim JM, Joh JW, et al. Streamline flow of the portal vein affects the lobar distribution of colorectal liver metastases and has a clinical impact on survival. Ann Surg Treat Res. 2017; 92:348–54.
Article19. House MG, Ito H, Gonen M, Fong Y, Allen PJ, DeMatteo RP, et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg. 2010; 210:744–55.
Article20. Wei AC, Greig PD, Grant D, Taylor B, Langer B, Gallinger S. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol. 2006; 13:668–76.
Article21. Leal JN, Bressan AK, Vachharajani N, Gonen M, Kingham TP, D’Angelica MI, et al. Time-to-surgery and survival outcomes in resectable colorectal liver metastases: a multi-institutional evaluation. J Am Coll Surg. 2016; 222:766–79.
Article22. Valderrama-Trevino AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Jave EE. Hepatic metastasis from colorectal cancer. Euroasian J Hepatogastroenterol. 2017; 7:166–75.
Article23. Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ. Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer. 2014; 14:810.
Article24. Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016; 27:1386–422.
Article25. Scorsetti M, Comito T, Tozzi A, Navarria P, Fogliata A, Clerici E, et al. Final results of a phase II trial for stereotactic body radiation therapy for patients with inoperable liver metastases from colorectal cancer. J Cancer Res Clin Oncol. 2015; 141:543–53.26. Rusthoven KE, Kavanagh BD, Cardenes H, Stieber VW, Burri SH, Feigenberg SJ, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol. 2009; 27:1572–8.
Article27. Hughes KS, Rosenstein RB, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of long-term survivors. Dis Colon Rectum. 1988; 31:1–4.28. Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005; 241:715–22.29. Bogach J, Wang J, Griffiths C, Parpia S, Saskin R, Hallet J, et al. Simultaneous versus staged resection for synchronous colorectal liver metastases: a population-based cohort study. Int J Surg. 2020; 74:68–75.
Article30. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999; 230:309–18.31. Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996; 77:1254–62.32. Gawdi R, Valenzuela CD, Moaven O, Stauffer JA, Del Piccolo NR, Cheung T, et al. Perioperative chemotherapy for resectable colorectal liver metastases: analysis from the Colorectal Operative Liver Metastases International Collaborative (COLOMIC). J Surg Oncol. 2022; 126:339–47.
Article33. Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007; 25:4575–80.
Article34. de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009; 250:440–8.35. Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, Dellanoce M, et al. Percutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology. 2001; 221:159–66.
Article36. Curley SA, Izzo F, Delrio P, Ellis LM, Granchi J, Vallone P, et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg. 1999; 230:1–8.
Article37. Ruers T, Van Coevorden F, Punt CJ, Pierie JE, Borel-Rinkes I, Ledermann JA, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017; 109:djx015.
Article38. Otto G, Duber C, Hoppe-Lotichius M, Konig J, Heise M, Pitton MB. Radiofrequency ablation as first-line treatment in patients with early colorectal liver metastases amenable to surgery. Ann Surg. 2010; 251:796–803.
Article39. Kron P, Linecker M, Jones RP, Toogood GJ, Clavien PA, Lodge JP. Ablation or resection for colorectal liver metastases? A systematic review of the literature. Front Oncol. 2019; 9:1052.
Article40. Gavriilidis P, Roberts KJ, de’Angelis N, Aldrighetti L, Sutcliffe RP. Recurrence and survival following microwave, radiofrequency ablation, and hepatic resection of colorectal liver metastases: a systematic review and network meta-analysis. Hepatobiliary Pancreat Dis Int. 2021; 20:307–14.
Article41. Wang LJ, Zhang ZY, Yan XL, Yang W, Yan K, Xing BC. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: a propensity score analysis. World J Surg Oncol. 2018; 16:207.
Article42. Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004; 239:818–25.
Article43. Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg. 2006; 141:460–6.44. White RR, Avital I, Sofocleous CT, Brown KT, Brody LA, Covey A, et al. Rates and patterns of recurrence for percutaneous radiofrequency ablation and open wedge resection for solitary colorectal liver metastasis. J Gastrointest Surg. 2007; 11:256–63.
Article45. Gleisner AL, Choti MA, Assumpcao L, Nathan H, Schulick RD, Pawlik TM. Colorectal liver metastases: recurrence and survival following hepatic resection, radiofrequency ablation, and combined resection-radiofrequency ablation. Arch Surg. 2008; 143:1204–12.46. McKay A, Fradette K, Lipschitz J. Long-term outcomes following hepatic resection and radiofrequency ablation of colorectal liver metastases. HPB Surg. 2009; 2009:346863.47. Reuter NP, Woodall CE, Scoggins CR, McMasters KM, Martin RC. Radiofrequency ablation vs. resection for hepatic colorectal metastasis: therapeutically equivalent? J Gastrointest Surg. 2009; 13:486–91.
Article48. Lee KH, Kim HO, Yoo CH, Son BH, Park YL, Cho YK, et al. Comparison of radiofrequency ablation and resection for hepatic metastasis from colorectal cancer. Korean J Gastroenterol. 2012; 59:218–23.
Article49. Agcaoglu O, Aliyev S, Karabulut K, El-Gazzaz G, Aucejo F, Pelley R, et al. Complementary use of resection and radiofrequency ablation for the treatment of colorectal liver metastases: an analysis of 395 patients. World J Surg. 2013; 37:1333–9.
Article50. Kim WW, Kim KH, Kim SH, Kim JS, Park SJ, Kim KH, et al. Comparison of hepatic resection and radiofrequency ablation for the treatment of colorectal liver metastasis. Indian J Surg. 2015; 77:1126–30.
Article51. Puijk RS, Ruarus AH, Vroomen L, van Tilborg A, Scheffer HJ, Nielsen K, et al. Colorectal liver metastases: surgery versus thermal ablation (COLLISION) - a phase III single-blind prospective randomized controlled trial. BMC Cancer. 2018; 18:821.
Article52. Comparison of hepatectomy and local ablation for resectable synchronous and metachronous colorectal liver metastasis (HELARC) [Internet]. Bethesda, MD: U.S. National Library of Medicine;2016. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT02886104 .53. Gurusamy K, Corrigan N, Croft J, Twiddy M, Morris S, Woodward N, et al. Liver resection surgery versus thermal ablation for colorectal LiVer MetAstases (LAVA): study protocol for a randomised controlled trial. Trials. 2018; 19:105.
Article54. Chang DT, Swaminath A, Kozak M, Weintraub J, Koong AC, Kim J, et al. Stereotactic body radiotherapy for colorectal liver metastases: a pooled analysis. Cancer. 2011; 117:4060–9.
Article55. Kress MS, Collins BT, Collins SP, Dritschilo A, Gagnon G, Unger K. Stereotactic body radiation therapy for liver metastases from colorectal cancer: analysis of safety, feasibility, and early outcomes. Front Oncol. 2012; 2:8.56. Burkon P, Slampa P, Kazda T, Slavik M, Prochazka T, Vrzal M. Stereotactic body radiation therapy for colorectal cancer liver metastases; early results. Klin Onkol. 2012; 25 Suppl 2:2S93–7.57. McPartlin A, Swaminath A, Wang R, Pintilie M, Brierley J, Kim J, et al. Long-term outcomes of phase 1 and 2 studies of SBRT for hepatic colorectal metastases. Int J Radiat Oncol Biol Phys. 2017; 99:388–95.
Article58. Joo JH, Park JH, Kim JC, Yu CS, Lim SB, Park IJ, et al. Local control outcomes using stereotactic body radiation therapy for liver metastases from colorectal cancer. Int J Radiat Oncol Biol Phys. 2017; 99:876–83.59. Doi H, Uemoto K, Suzuki O, Yamada K, Masai N, Tatsumi D, et al. Effect of primary tumor location and tumor size on the response to radiotherapy for liver metastases from colorectal cancer. Oncol Lett. 2017; 14:453–60.
Article60. Barry A, Wong R, Dawson LA. The management of colorectal cancer liver metastases: the radiation oncology viewpoint. Int J Radiat Oncol Biol Phys. 2019; 103:540–1.
Article61. Kim YS, Lim HK, Rhim H, Lee MW, Choi D, Lee WJ, et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol. 2013; 58:89–97.
Article62. Goldberg SN, Hahn PF, Tanabe KK, Mueller PR, Schima W, Athanasoulis CA, et al. Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol. 1998; 9:101–11.
Article63. Kim N, Cheng J, Jung I, Liang J, Shih YL, Huang WY, et al. Stereotactic body radiation therapy vs. radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol. 2020; 73:121–9.
Article64. Kang TW, Lim HK, Lee MW, Kim YS, Choi D, Rhim H. First-line radiofrequency ablation with or without artificial ascites for hepatocellular carcinomas in a subcapsular location: local control rate and risk of peritoneal seeding at long-term follow-up. Clin Radiol. 2013; 68:e641–51.65. Rim CH, Lee HY, Kim JS, Kim H. Radiofrequency ablation and stereotactic body radiotherapy for hepatocellular carcinoma: should they clash or reconcile? Int J Radiat Biol. 2021; 97:111–9.66. Radiofrequency ablation versus stereotactic radiotherapy in colorectal liver metastases (RAS01) [Internet]. Bethesda, MD: U.S. National Library of Medicine;2016. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT01233544 .67. Yu J, Kim DH, Lee J, Shin YM, Kim JH, Yoon SM, et al. Radiofrequency ablation versus stereotactic body radiation therapy in the treatment of colorectal cancer liver metastases. Cancer Res Treat. 2022; 54:850–9.68. Franzese C, Comito T, Clerici E, Di Brina L, Tomatis S, Navar-ria P, et al. Liver metastases from colorectal cancer: propensity score-based comparison of stereotactic body radiation therapy vs. microwave ablation. J Cancer Res Clin Oncol. 2018; 144:1777–83.
Article69. Stintzing S, Grothe A, Hendrich S, Hoffmann RT, Heinemann V, Rentsch M, et al. Percutaneous radiofrequency ablation (RFA) or robotic radiosurgery (RRS) for salvage treatment of colorectal liver metastases. Acta Oncol. 2013; 52:971–7.
Article70. Vigano L, Pedicini V, Comito T, Carnaghi C, Costa G, Poretti D, et al. Aggressive and multidisciplinary local approach to iterative recurrences of colorectal liver metastases. World J Surg. 2018; 42:2651–9.
Article71. Nieuwenhuizen S, Dijkstra M, Puijk RS, Timmer FE, Nota IM, Opperman J, et al. Thermal ablation versus stereotactic ablative body radiotherapy to treat unresectable colorectal liver metastases: a comparative analysis from the prospective Amsterdam CORE Registry. Cancers (Basel). 2021; 13:4303.
Article72. Gotohda N, Nomura S, Doi M, Karasawa K, Ohki T, Shimizu Y, et al. Clinical impact of radiofrequency ablation and stereotactic body radiation therapy for colorectal liver metastasis as local therapies for elderly, vulnerable patients. JGH Open. 2020; 4:722–8.
Article73. Cheng JY, Liu CM, Wang YM, Hsu HC, Huang EY, Huang TT, et al. Proton versus photon radiotherapy for primary hepatocellular carcinoma: a propensity-matched analysis. Radiat Oncol. 2020; 15:159.
Article74. Kim TH, Koh YH, Kim BH, Kim MJ, Lee JH, Park B, et al. Proton beam radiotherapy vs. radiofrequency ablation for recurrent hepatocellular carcinoma: a randomized phase III trial. J Hepatol. 2021; 74:603–12.
Article75. Hong TS, Wo JY, Borger DR, Yeap BY, McDonnell EI, Willers H, et al. Phase II study of proton-based stereotactic body radiation therapy for liver metastases: importance of tumor genotype. J Natl Cancer Inst. 2017; 109:djx031.
Article76. Kim K, Yu JI, Park HC, Yoo GS, Lim DH, Noh JM, et al. A phase II trial of hypofractionated high-dose proton beam therapy for unresectable liver metastases. Radiother Oncol. 2022; 176:9–16.
Article77. Curative proton beam therapy for patients with liver metastasis of colorectal cancer [Internet]. Bethesda, MD: U.S. National Library of Medicine;2019. [cited 2022 Jan 28]. Available from: https://clinicaltrials.gov/ct2/show/NCT03577665 .78. Lee MT, Kim JJ, Dinniwell R, Brierley J, Lockwood G, Wong R, et al. Phase I study of individualized stereotactic body radiotherapy of liver metastases. J Clin Oncol. 2009; 27:1585–91.79. Oh D, Ahn YC, Seo JM, Shin EH, Park HC, Lim DH, et al. Potentially curative stereotactic body radiation therapy (SBRT) for single or oligometastasis to the lung. Acta Oncol. 2012; 51:596–602.
Article80. Ahmed KA, Caudell JJ, El-Haddad G, Berglund AE, Welsh EA, Yue B, et al. Radiosensitivity differences between liver metastases based on primary histology suggest implications for clinical outcomes after stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2016; 95:1399–404.
Article81. Anuja K, Chowdhury AR, Saha A, Roy S, Rath AK, Kar M, et al. Radiation-induced DNA damage response and resistance in colorectal cancer stem-like cells. Int J Radiat Biol. 2019; 95:667–79.
Article82. Bardelli A, Saha S, Sager JA, Romans KE, Xin B, Markowitz SD, et al. PRL-3 expression in metastatic cancers. Clin Cancer Res. 2003; 9:5607–15.83. Scott JG, Berglund A, Schell MJ, Mihaylov I, Fulp WJ, Yue B, et al. A genome-based model for adjusting radiotherapy dose (GARD): a retrospective, cohort-based study. Lancet Oncol. 2017; 18:202–11.
Article84. Andre T, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N Engl J Med. 2020; 383:2207–18.
Article85. Diaz LA Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022; 23:659–70.
Article86. Pevzner AM, Tsyganov MM, Ibragimova MK, Litvyakov NV. Abscopal effect in the radio and immunotherapy. Radiat Oncol J. 2021; 39:247–53.87. Torok JA, Salama JK. Combining immunotherapy and radiotherapy for the STAR treatment. Nat Rev Clin Oncol. 2019; 16:666–7.
Article88. Ngwa W, Irabor OC, Schoenfeld JD, Hesser J, Demaria S, Formenti SC. Using immunotherapy to boost the abscopal effect. Nat Rev Cancer. 2018; 18:313–22.
Article89. Ebner DK, Kamada T, Yamada S. Abscopal effect in recurrent colorectal cancer treated with carbon-ion radiation therapy: 2 case reports. Adv Radiat Oncol. 2017; 2:333–8.
Article90. Ji D, Song C, Li Y, Xia J, Wu Y, Jia J, et al. Combination of radiotherapy and suppression of Tregs enhances abscopal antitumor effect and inhibits metastasis in rectal cancer. J Immunother Cancer. 2020; 8:e000826.
Article91. Parikh AR, Szabolcs A, Allen JN, Clark JW, Wo JY, Raabe M, et al. Radiation therapy enhances immunotherapy response in microsatellite stable colorectal and pancreatic adenocarcinoma in a phase II trial. Nat Cancer. 2021; 2:1124–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of metastasis-directed therapy and local therapy of the primary tumor in the management of oligometastatic prostate cancer
- Complete response to local therapy for advanced hepatocellular carcinoma with lung metastasis: a case report
- Long-term survival after multimodal treatment involving radiotherapy for huge hepatocellular carcinoma with oligometastasis: a case report
- Management of Colorectal Cancer Liver Metastasis
- Differential Perspectives by Specialty on Oligometastatic Colorectal Cancer: A Korean Oligometastasis Working Group’s Comparative Survey Study