Korean J Health Promot.
2023 Jun;23(2):65-74. 10.15384/kjhp.2023.23.2.65.
Influence of Job Stress and Resilience on Burnout of Clinical Nurses Working in Small and Medium-Sized Hospital: Focusing on Comparing National Safety Hospital and COVID-19 Dedicated Hospital
- Affiliations
-
- 1Department of Nursing, New Sungmin Hospital, Incheon, Korea
- 2Department of Nursing, College of Nursing, Gachon University, Incheon, Korea
- KMID: 2544123
- DOI: http://doi.org/10.15384/kjhp.2023.23.2.65
Abstract
- Background
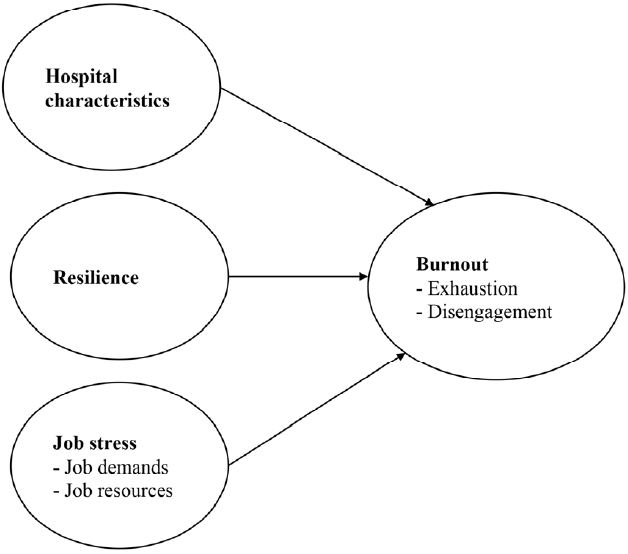
This study was conducted to compare the job stress, resilience, and burnout levels of small and medium-sized hospital nurses working at National safety hospitals and coronavirus disease-19 (COVID-19) dedicated hospitals, and to identify influencing factors on burnout.
Methods
This study was a cross-sectional study and research participants were nurses at small and medium-sized hospitals working at National safety hospitals and COVID-19 dedicated hospitals. Data from 292 nurses collected using a structured questionnaires from April 1 to 30, 2020 were used. Data was analyzed using multiple regression analyses.
Results
As a result of this study, there was a significant difference in stress on job demand and job resources of nurses working at National safety hospital type B and COVID-19 dedicated Hospital. There was no difference in job stress and resilience of nurses among types of hospitals. As a result of multiple regression, stress to job demands and resilience were factors influencing the level of exhaustion of nurses. Stress to job demands and job resources and resilience were factors influencing the level of disengagement of nurses.
Conclusions
Considering the results of this study, it is suggested to introduce strategies to reduce nurses’ job stress and burnout caused by COVID-19.
Figure
Reference
-
1. Kang J, Jang YY, Kim J, Han SH, Lee KR, Kim M, et al. South Korea’s responses to stop the COVID-19 pandemic. Am J Infect Control. 2020; 48(9):1080–6.
Article2. World Health Organization. Timeline: WHO’s COVID-19 response [Internet]. Geneva: World Health Organization; 2023 [cited Apr 30, 2023]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline.3. Center Disaster Management Headquarters and Center Disease Control Headquarters. Occurence status [Internet]. Osong: Center Disaster Management Headquarters and Center Disease Control Headquarters; 2023 [cited Feb 20, 2023]. Available from: https://ncov.kdca.go.kr/.4. Center Disaster Management Headquarters and Center Disease Control Headquarters. Public advice & notice [Internet]. Osong: Center Disaster Management Headquarters and Center Disease Control Headquarters; 2023 [cited Feb 20, 2023]. Available from: https://ncov.kdca.go.kr/duBoardList.do.5. Ha BY, Bae YS, Ryu HS, Jeon MK. Experience of nurses in charge of COVID-19 screening at general hospitals in Korea. J Korean Acad Nurs. 2022; 52(1):66–79.
Article6. Kim HY, Kim M, Jung SO, Kim HJ. The experience of ward nurses participating in COVID-19 patient care. J Korea Soc Wellness. 2022; 17(1):311–21.
Article7. Chung S, Seong M, Park JY. Nurses’ experience in COVID-19 patient care. J Korean Acad Nurs Adm. 2022; 28(2):142–53.
Article8. Kim GH, You JO, Lee M, Choi Y, Lee YM, Shin JH. Factors affecting burnout among tertiary hospital nurses during the COVID-19 outbreak. J Korean Acad Psychiatr Ment Health Nurs. 2021; 30(4):390–9.
Article9. Sullivan D, Sullivan V, Weatherspoon D, Frazer C. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. 2022; 57(1):79–99.
Article10. Kim J, Lee TJ, Choi H, Park E. Measures to establish public medical infrastructure to respond to infectious disease crises [Internet]. Seoul: Seoul National University SNU R&DB Foundation; 2021 [cited Apr 21, 2023]. Available from: https://educat.na.go.kr:444/flexer/index2.jsp?ftype=hwp&attachNo=467216.11. Shin R, Baek HJ, Ahn DB. Influence of job stress and resilience on the burnout of nurses who works at the designated public relief hospital. J Korea Cont Assoc. 2021; 21(9):595–608.12. Kim H, Kim D, Kim M, Kim Y, Bang S, Lee G, et al. Factors influencing burnout of nurses working in a hospital nationally designated for COVID-19 patients. Korean J Adult Nurs. 2022; 34(1):74–84.
Article13. Park SM, Ha YJ. Effects of job stress, social supprt, and resilience on burnout of nurses in the national infectious disease hospital. J Korea Soc Wellness. 2022; 17(4):75–81.
Article14. Hong JY, Chae J, Song MR, Kim EM. A utilization strategy of nursing staff by types of medical institutions-nurse staffing level of medium and small-sized hospitals. J Korea Academia-Industrial Cooperation Soc. 2017; 18(8):162–70.15. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001; 86(3):499–512.
Article16. Fletcher D, Sarkar M. Psychological resilience. Eur Psychol. 2013; 18(1):12–23.
Article17. Kim JS, Choi JS. Factors influencing emergency nurses’ burnout during an outbreak of Middle East respiratory syndrome coronavirus in Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2016; 10(4):295–9.
Article18. Baek H, Kim I, Park JH, Yun M, Nam EJ. Standardization of the occupational stress scale for Korean nurses (1433) [Internet]. Ulsan: Korea Occupational Safety and Health Agency; 2019 [cited Jan 27, 2020]. Available from: https://www.kosha.or.kr/oshri/publication/researchReportSearch.do?mode=download&articleNo=411125&attachNo=232357.19. Na YJ. The construct validity of the oldenburg burnout inventory (OLBI) [dissertation]. Suwon: Ajou University;2013. Korean.20. Park MM, Park JW. Development of resilience scale for nurses. J Korean Acad Fundam Nurs. 2016; 23(1):32–41.
Article21. Kim SH, Park SH. Verification of validity and reliability of resilience scale for nurses. JKDAS. 2016; 18(4B):2257–69.22. Lee HJ, Jung M. The effect of workplace bullying, job stress, and organizational commitment on turnover intention of nurses in small and medium-sized hospitals. J Korea Cont Assoc. 2020; 20(8):572–82.23. Hwang S, Kwon KT. Burnout among healthcare workers during COVID-19 pandemic. Korean J Healthcare Assoc Infect Control Prev. 2022; 27(1):28–34.
Article24. Seo YE, Kim HC, Yoo SY, Lee KU, Lee HW, Lee SH. Factors associated with burnout among healthcare workers during an outbreak of MERS. Psychiatry Investig. 2020; 17(7):674–80.
Article25. Oh H, Lee NK. A phenomenological study of the lived experience of nurses caring for patients with COVID-19 in Korea. J Korean Acad Nurs. 2021; 51(5):561–72.
Article26. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979; 24(2):285–308.
Article27. Budisavljevic A, Kelemenic-Drazin R, Silovski T, Plestina S, Plavetic ND. Correlation between psychological resilience and burnout syndrome in oncologists amid the Covid-19 pandemic. Support Care Cancer. 2023; 31(4):207.
Article28. Jo S, Kurt S, Bennett JA, Mayer K, Pituch KA, Simpson V, et al. Nurses' resilience in the face of coronavirus (COVID-19): an international view. Nurs Health Sci. 2021; 23(3):646–57.29. Stacey G, Cook G. A scoping review exploring how the conceptualisation of resilience in nursing influences interventions aimed at increasing resilience. Int Pract Dev J. 2019; 9(1):1–16.
Article30. Henshall C, Davey Z, Jackson D. Nursing resilience interventions-a way forward in challenging Healthcare territories. J Clin Nurs. 2020; 29(19-20):3597–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing Burnout of Nurses Working in a Hospital Nationally Designated for COVID-19 Patients
- Influence of the Job Stress, Resilience, and Professional Identity on Burnout in Operation Room Nurses
- Relationship between Job Stress and Compassion Satisfaction, Compassion Fatigue, Burnout for Nurses in Children's Hospital
- Moderating Effects of Work-family Conflict between Job . Organizational . Career Characteristics and Turnover Intention among Nurses in Small and Medium-sized Hospitals
- The Impact of Job Stress on the Patient Safety Nursing Activity among Nurses in Small-Medium Sized General Hospitals