Korean J Transplant.
2023 Jun;37(2):135-140. 10.4285/kjt.23.0001.
Transplant-associated Kaposi’s sarcoma in a kidney allograft: a case report
- Affiliations
-
- 1Division of Kidney and Pancreas Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2544119
- DOI: http://doi.org/10.4285/kjt.23.0001
Abstract
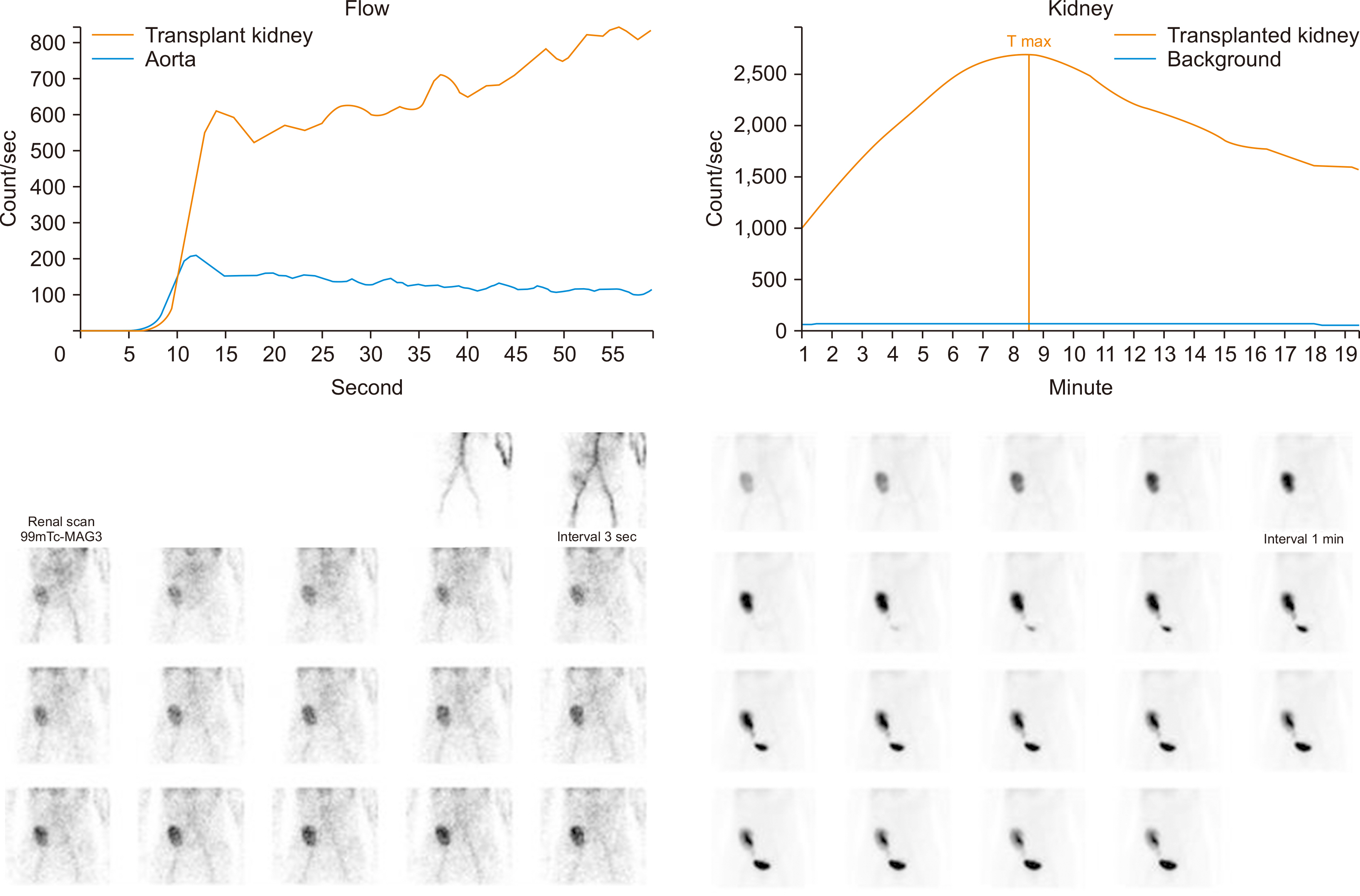
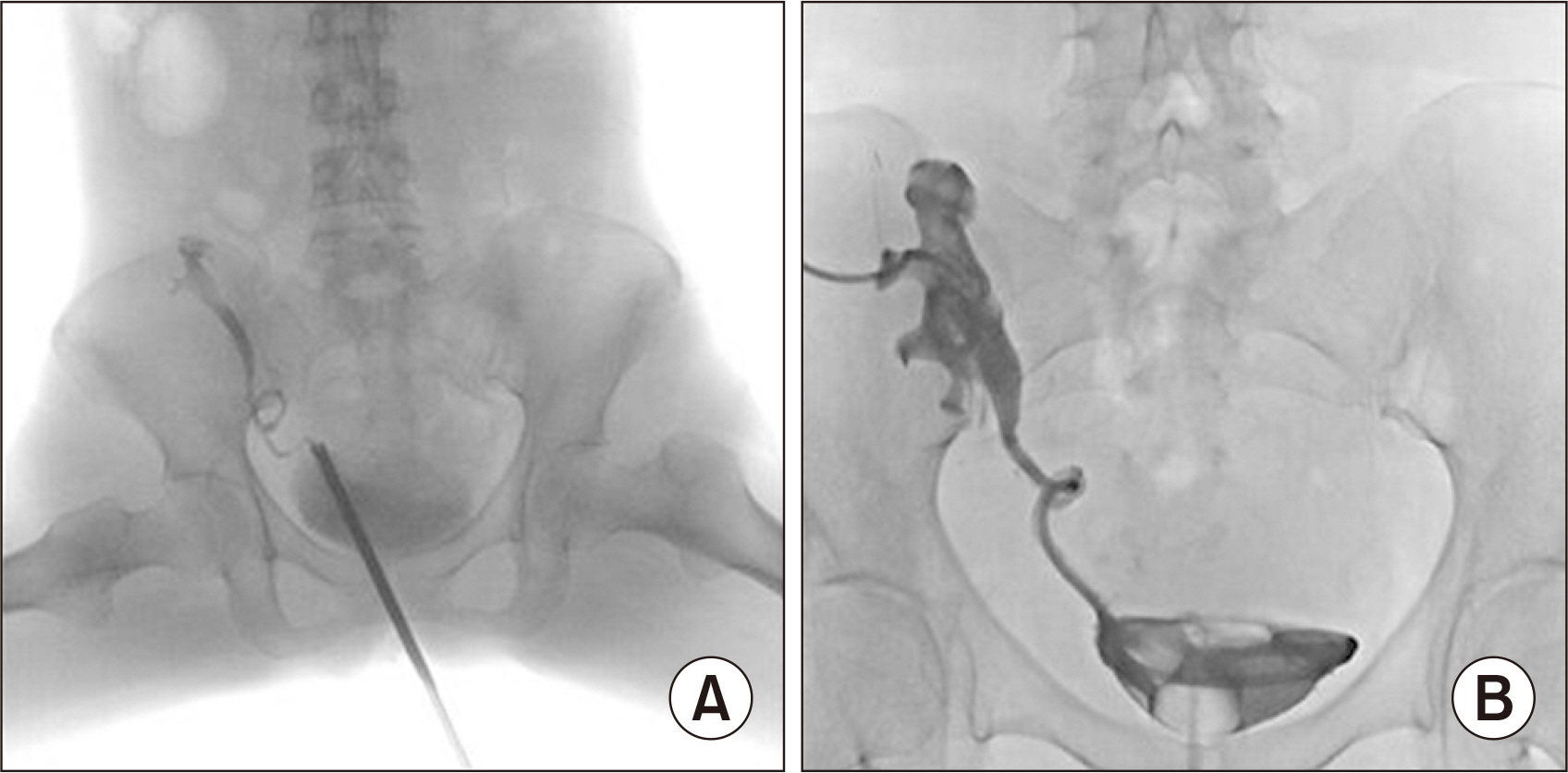
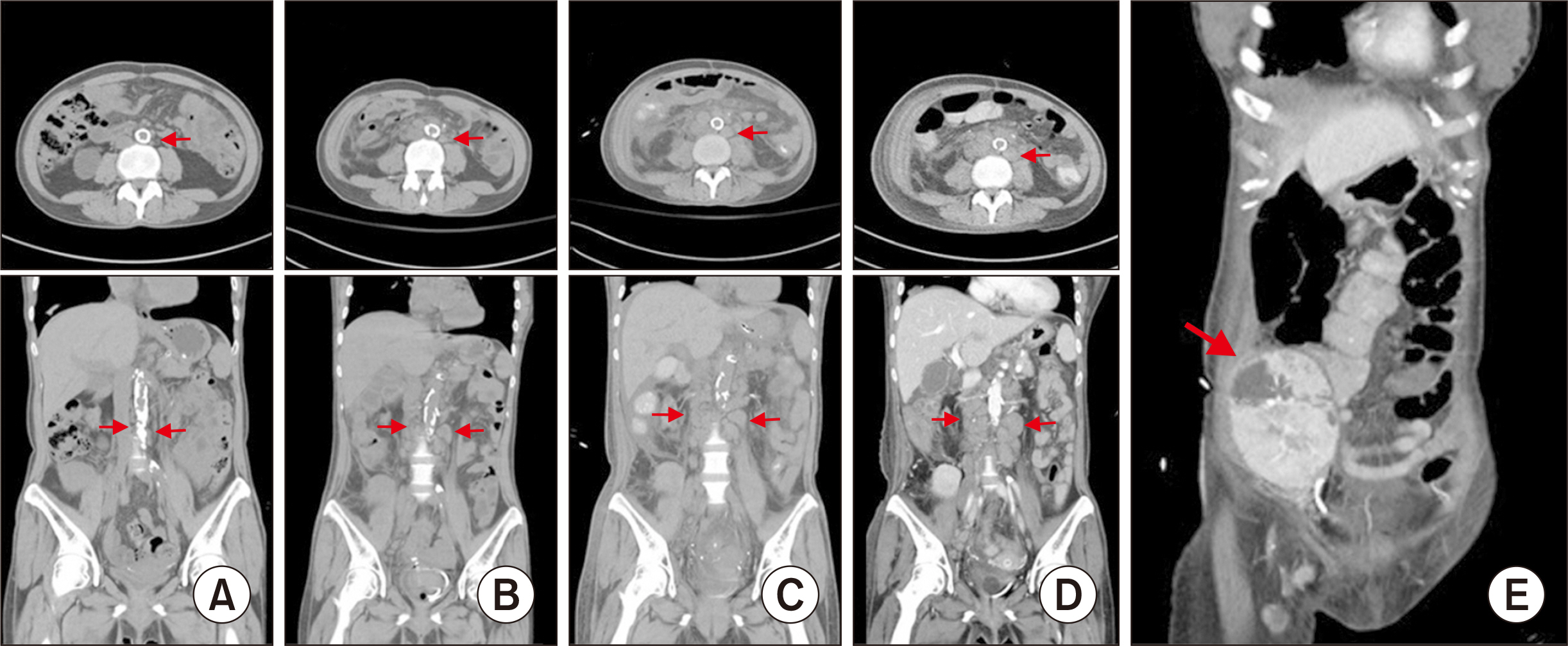
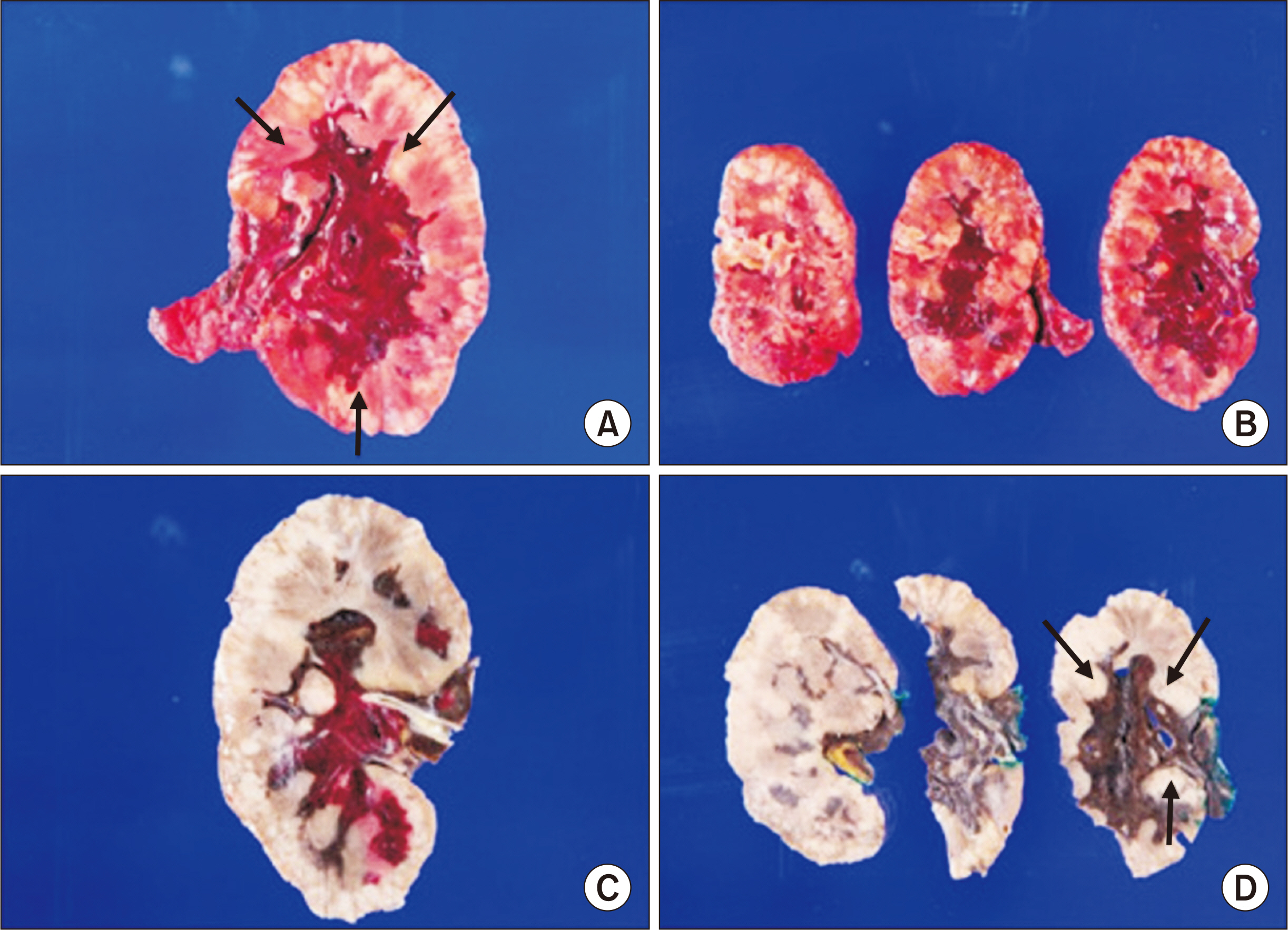
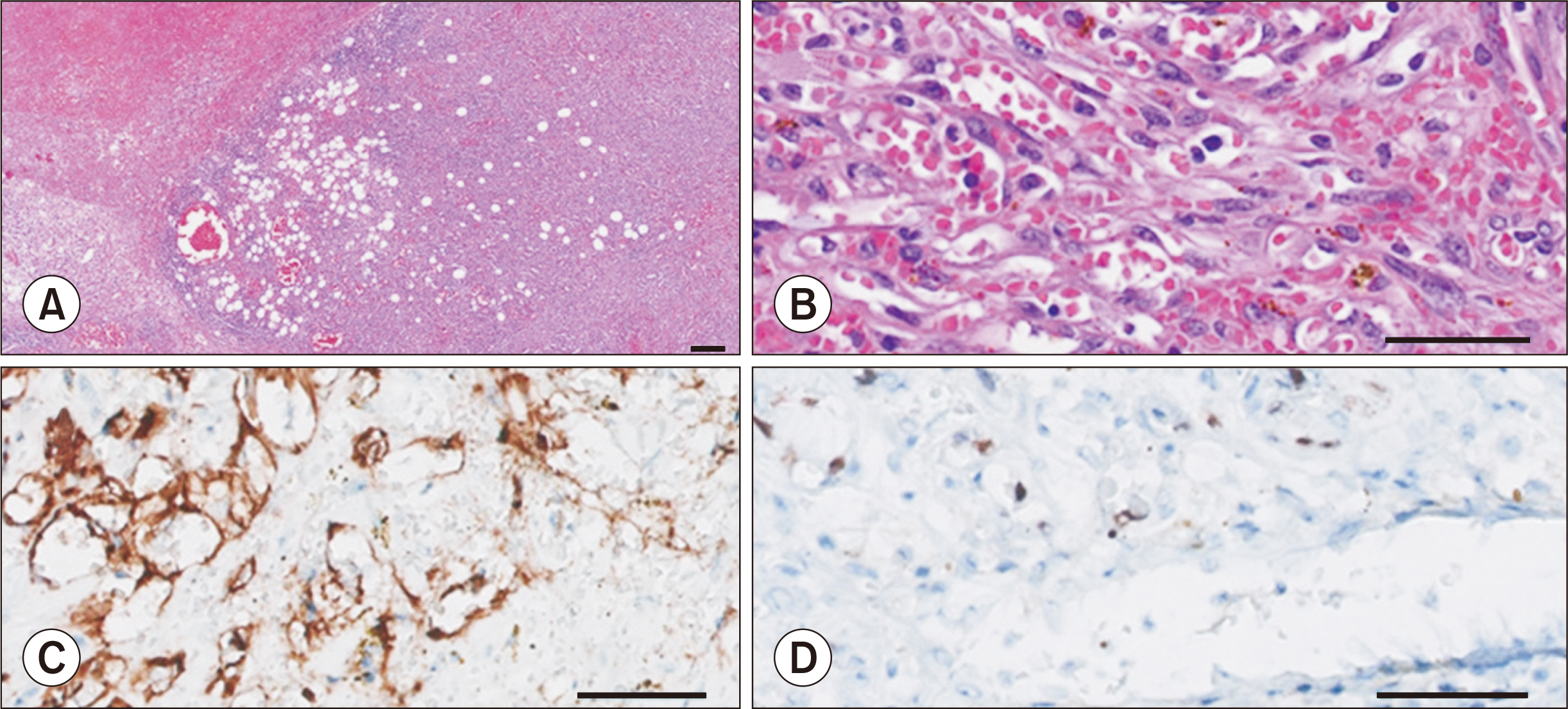
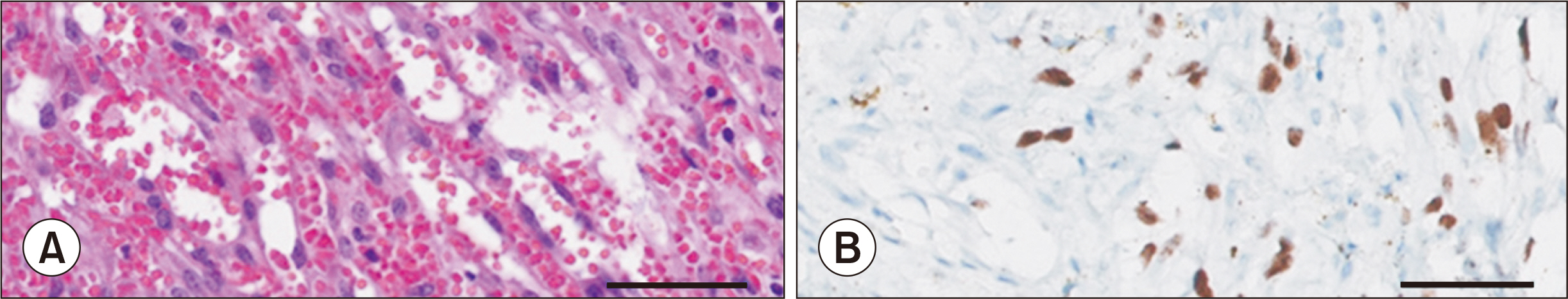
- Kaposi’s sarcoma (KS) is a disease that is not widely known among the general public, but has a high prevalence among organ transplant recipients. Here, we present a rare case of intragraft KS after kidney transplantation. A 53-year-old woman who had been on hemodialysis due to diabetic nephropathy underwent deceased-donor kidney transplantation on December 7, 2021. Approximately 10 weeks after kidney transplantation, her creatinine level increased to 2.99 mg/dL. Upon examination, ureter kinking was confirmed between the ureter orifices and the transplanted kidney. As a result, percutaneous nephrostomy was performed, and a ureteral stent was inserted. During the procedure, bleeding occurred due to a renal artery branch injury, and embolization was performed immediately. Subsequently, kidney necrosis and uncontrolled fever developed, leading to graftectomy. Surgical findings revealed that the kidney parenchyma was necrotic as a whole, and lymphoproliferative lesions had formed diffusely around the iliac artery. These lesions were removed during graftectomy, and a histological examination was performed. The kidney graft and lymphoproliferative lesions were diagnosed as KS based on a histological examination. We report a rare case in which a recipient developed KS in the kidney allograft as well as in adjacent lymph nodes.
Figure
Reference
-
1. Stallone G, Schena A, Infante B, Di Paolo S, Loverre A, Maggio G, et al. 2005; Sirolimus for Kaposi's sarcoma in renal-transplant recipients. N Engl J Med. 352:1317–23. DOI: 10.1056/NEJMoa042831. PMID: 15800227.
Article2. Lebbé C, Euvrard S, Barrou B, Pouteil-Noble C, Garnier JL, Glotz D, et al. 2006; Sirolimus conversion for patients with posttransplant Kaposi's sarcoma. Am J Transplant. 6:2164–8. DOI: 10.1111/j.1600-6143.2006.01412.x. PMID: 16780549.
Article3. Barete S, Calvez V, Mouquet C, Barrou B, Kreis H, Dantal J, et al. 2000; Clinical features and contribution of virological findings to the management of Kaposi sarcoma in organ-allograft recipients. Arch Dermatol. 136:1452–8. DOI: 10.1001/archderm.136.12.1452. PMID: 11115155.
Article4. Harwood AR, Osoba D, Hofstader SL, Goldstein MB, Cardella CJ, Holecek MJ, et al. 1979; Kaposi's sarcoma in recipients of renal transplants. Am J Med. 67:759–65. DOI: 10.1016/0002-9343(79)90731-9. PMID: 159624.
Article5. Kim B, Kang M, Kim Y, Lee HS, Kim B, Lee JJ, et al. 2021; De novo cancer incidence after kidney transplantation in South Korea from 2002 to 2017. J Clin Med. 10:3530. DOI: 10.3390/jcm10163530. PMID: 34441826. PMCID: PMC8396914.
Article6. Donia AF, Fouda MA, Ghoneim ME, Refaie AF, Ali-El-Dein B. 2021; The previously common post-kidney transplant Kaposi sarcoma has become non-existent for a decade: an Egyptian experience. J Cancer Res Clin Oncol. 147:1493–8. DOI: 10.1007/s00432-020-03433-1. PMID: 33130940.
Article7. Dollard SC, Butler LM, Jones AM, Mermin JH, Chidzonga M, Chipato T, et al. 2010; Substantial regional differences in human herpesvirus 8 seroprevalence in sub-Saharan Africa: insights on the origin of the "Kaposi's sarcoma belt". Int J Cancer. 127:2395–401. DOI: 10.1002/ijc.25235. PMID: 20143397. PMCID: PMC2895015.
Article8. Cesarman E, Damania B, Krown SE, Martin J, Bower M, Whitby D. 2019; Kaposi sarcoma. Nat Rev Dis Primers. 5:9. DOI: 10.1038/s41572-019-0060-9. PMID: 30705286. PMCID: PMC6685213.
Article9. Singh N. 2000; Human herpesviruses-6, -7 and -8 in organ transplant recipients. Clin Microbiol Infect. 6:453–9. DOI: 10.1046/j.1469-0691.2000.00129.x. PMID: 11168178.
Article10. Whitby D, Luppi M, Barozzi P, Boshoff C, Weiss RA, Torelli G. 1998; Human herpesvirus 8 seroprevalence in blood donors and lymphoma patients from different regions of Italy. J Natl Cancer Inst. 90:395–7. DOI: 10.1093/jnci/90.5.395. PMID: 9498490.
Article11. Anderson MA, Ying T, Wyburn K, Ferguson PM, Strach MC, Grimison P, et al. 2021; Transplant-associated penile Kaposi sarcoma managed with single agent paclitaxel chemotherapy: a case report. BMC Urol. 21:87. DOI: 10.1186/s12894-021-00855-y. PMID: 34098936. PMCID: PMC8186205.
Article12. Butkus DE, Kirchner KA, Neill J, Raju S. 1989; Kaposi's sarcoma in a transplanted kidney. Transplantation. 48:146–9. DOI: 10.1097/00007890-198907000-00034. PMID: 2665220.
Article13. Diaz-Candamio MJ, Pombo F, Lorenzo MJ, Alonso A. 1998; Kaposi's sarcoma involving a transplanted kidney: CT findings. AJR Am J Roentgenol. 171:1073–4. DOI: 10.2214/ajr.171.4.9762999. PMID: 9762999.
Article14. Rha SE, Byun JY, Kim HH, Baek JH, Hwang TK, Kang SJ. 2000; Kaposi's sarcoma involving a transplanted kidney, ureter and urinary bladder: ultrasound and CT findings. Br J Radiol. 73:1221–3. DOI: 10.1259/bjr.73.875.11144804. PMID: 11144804.
Article15. Delyon J, Rabate C, Euvrard S, Harwood CA, Proby C, Güleç AT, et al. 2019; Management of Kaposi sarcoma after solid organ transplantation: a European retrospective study. J Am Acad Dermatol. 81:448–55. DOI: 10.1016/j.jaad.2019.03.028. PMID: 30902727.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic Kaposi Sarcoma after Kidney Transplantation: A Case Report
- Intragraft Kaposi’s sarcoma after kidney transplantation: a case report
- A Case of Recurrent Kaposi's Sarcoma after Cyclosporine Treatment in Kidney Transplantation Patient
- Kaposi's sarcoma of the oral cavity in renal transplanted patient; a case report
- Intrathoracic Kaposi's Sarcoma in Renal Transplant Recipient proven by Open Lung Biospsy: A Case Report