J Korean Med Sci.
2023 Jun;38(24):e183. 10.3346/jkms.2023.38.e183.
Intravenous Versus Perineural Dexamethasone for Reducing Rebound Pain After Interscalene Brachial Plexus Block: A Randomized Controlled Trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- 2Department of Orthopedic Surgery, College of Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- KMID: 2543974
- DOI: http://doi.org/10.3346/jkms.2023.38.e183
Abstract
- Background
Interscalene brachial plexus block (ISB) is a common regional technique to manage acute postoperative pain for arthroscopic rotator cuff tear repair. However, rebound pain may compromise its overall benefit. Our aim was to investigate the primary hypothesis that perineural and intravenous dexamethasone have different effects on rebound pain after resolution of ISB for arthroscopic rotator cuff tear repair.
Methods
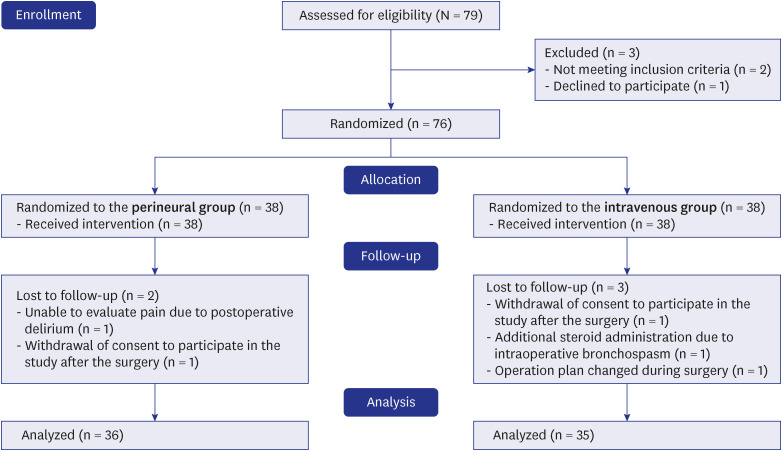
Patients aged ≥ 20 years scheduled for elective arthroscopic rotator cuff tear repair under general anesthesia with preoperative ISB were included. The participants were randomized to receive dexamethasone either perineurally (perineural group) or intravenously (intravenous group). In the perineural group, patients received ISB with 12 mL of 0.5% ropivacaine containing 5 mg of dexamethasone; simultaneously, 1 mL of 0.9% normal saline was administered intravenously. In the intravenous group, patients received ISB with 12 mL of 0.5% ropivacaine; simultaneously, 1 mL of dexamethasone 5 mg was administered intravenously. The primary outcome was the difference in the pain score (0–10 on numeric rating scale) between before and after ISB resolution. The secondary outcomes were the incidence of rebound pain; onset, duration, and intensity of rebound pain; time to the first analgesic request; and pain-related sleep disturbance.
Results
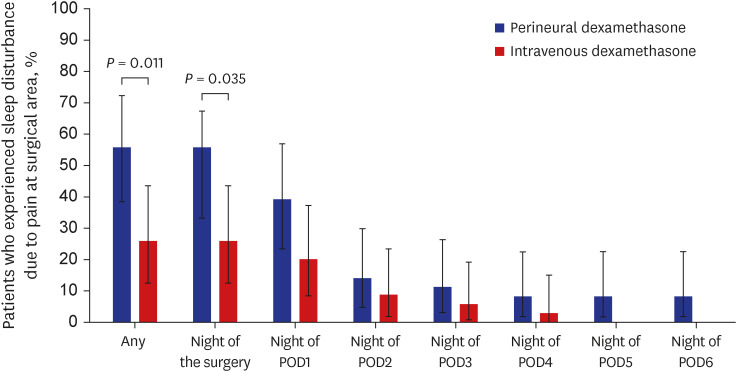
A total of 71 patients were randomized to either perineural group (n = 36) or intravenous group (n = 35). After block resolution, pain scores increased significantly more in the perineural group (mean ± standard deviation, 4.9 ± 2.1) compared to the intravenous group (4.0 ± 1.7, P = 0.043). The duration of ISB was more prolonged in the perineural group (median [interquartile range], 19.9 [17.2–23.1] hours) than the intravenous group (15.1 [13.7–15.9] hours, P < 0.001). The incidence of rebound pain and pain-related sleep disturbance during the first postoperative week was significantly higher in the perineural group than in the intravenous group (rebound pain: 44.4% vs. 20.0%, P = 0.028; sleep disturbance: 55.6% vs. 25.7%, P = 0.011). The duration and intensity of rebound pain were similar between the two groups.
Conclusion
Although perineural dexamethasone provided longer postoperative analgesia, intravenous dexamethasone was more beneficial in reducing pain increase after ISB resolution, incidence of rebound pain, and pain-related sleep disturbance.
Figure
Reference
-
1. Calvo E, Torres MD, Morcillo D, Leal V. Rotator cuff repair is more painful than other arthroscopic shoulder procedures. Arch Orthop Trauma Surg. 2019; 139(5):669–674. PMID: 30560289.2. Lavand’homme P. Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol. 2018; 31(6):679–684. PMID: 30124544.3. Sunderland S, Yarnold CH, Head SJ, Osborn JA, Purssell A, Peel JK, et al. Regional versus general anesthesia and the incidence of unplanned health care resource utilization for postoperative pain after wrist fracture surgery: results from a retrospective quality improvement project. Reg Anesth Pain Med. 2016; 41(1):22–27. PMID: 26650425.4. Muñoz-Leyva F, Cubillos J, Chin KJ. Managing rebound pain after regional anesthesia. Korean J Anesthesiol. 2020; 73(5):372–383. PMID: 32773724.5. Kahn RL, Cheng J, Gadulov Y, Fields KG, YaDeau JT, Gulotta LV. Perineural low-dose dexamethasone prolongs interscalene block analgesia with bupivacaine compared with systemic dexamethasone: a randomized trial. Reg Anesth Pain Med. 2018; 43(6):572–579. PMID: 29889698.6. Sakae TM, Marchioro P, Schuelter-Trevisol F, Trevisol DJ. Dexamethasone as a ropivacaine adjuvant for ultrasound-guided interscalene brachial plexus block: a randomized, double-blinded clinical trial. J Clin Anesth. 2017; 38:133–136. PMID: 28372653.7. McHardy PG, Singer O, Awad IT, Safa B, Henry PD, Kiss A, et al. Comparison of the effects of perineural or intravenous dexamethasone on low volume interscalene brachial plexus block: a randomised equivalence trial. Br J Anaesth. 2020; 124(1):84–91. PMID: 31591018.8. Heesen M, Klimek M, Imberger G, Hoeks SE, Rossaint R, Straube S. Co-administration of dexamethasone with peripheral nerve block: intravenous vs perineural application: systematic review, meta-analysis, meta-regression and trial-sequential analysis. Br J Anaesth. 2018; 120(2):212–227. PMID: 29406171.9. Woo JH, Lee HJ, Oh HW, Lee JW, Baik HJ, Kim YJ. Perineural dexamethasone reduces rebound pain after ropivacaine single injection interscalene block for arthroscopic shoulder surgery: a randomized controlled trial. Reg Anesth Pain Med. 2021; 46(11):965–970. PMID: 34535548.10. Henzi I, Walder B, Tramèr MR. Dexamethasone for the prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg. 2000; 90(1):186–194. PMID: 10625002.11. Jacobs A, Lemoine A, Joshi GP, Van de Velde M, Bonnet F. PROSPECT Working Group Collaborators. PROSPECT guideline for oncological breast surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2020; 75(5):664–673. PMID: 31984479.12. Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014; 112(6):991–1004. PMID: 24829420.13. Kim JY, Song SH, Cho JH, Cho HR. Comparison of clinical efficacy among remifentanil, nicardipine, and remifentanil plus nicardipine continuous infusion for hypotensive anesthesia during arthroscopic shoulder surgery. J Orthop Surg (Hong Kong). 2017; 25(2):2309499017716251. PMID: 28639533.14. Chun EH, Kim YJ, Woo JH. Which is your choice for prolonging the analgesic duration of single-shot interscalene brachial blocks for arthroscopic shoulder surgery? intravenous dexamethasone 5 mg vs. perineural dexamethasone 5 mg randomized, controlled, clinical trial. Medicine (Baltimore). 2016; 95(23):e3828. PMID: 27281084.15. Kawanishi R, Yamamoto K, Tobetto Y, Nomura K, Kato M, Go R, et al. Perineural but not systemic low-dose dexamethasone prolongs the duration of interscalene block with ropivacaine: a prospective randomized trial. Local Reg Anesth. 2014; 7:5–9. PMID: 24817819.16. Chong MA, Berbenetz NM, Lin C, Singh S. Perineural versus intravenous dexamethasone as an adjuvant for peripheral nerve blocks: a systematic review and meta-analysis. Reg Anesth Pain Med. 2017; 42(3):319–326. PMID: 28252523.17. Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34(5):335–338. PMID: 2167604.18. Pehora C, Pearson AM, Kaushal A, Crawford MW, Johnston B. Dexamethasone as an adjuvant to peripheral nerve block. Cochrane Database Syst Rev. 2017; 11(11):CD011770. PMID: 29121400.19. Huang L, Li P, Zhang L, Kang G, Zhou H, Zhao Z. Analgesic comparison between perineural and intravenous dexamethasone for shoulder arthroscopy: a meta-analysis of randomized controlled trials. J Orthop Surg. 2022; 17(1):103.20. Williams BA, Schott NJ, Mangione MP, Ibinson JW. Perineural dexamethasone and multimodal perineural analgesia: how much is too much? Anesth Analg. 2014; 118(5):912–914. PMID: 24781562.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent updates on interscalene brachial plexus block for shoulder surgery
- Prolonged Horner's Syndrome Following Interscalene Brachial Plexus Block: A case report
- A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial
- Bilateral Interscalene Brachial Plexus Block for Surgery on Both Upper Extremities in a Patient with Unilateral Vocal Cord Paralysis : A case report
- Effects of Interscalene Brachial Plexus Block Combined with Patient Controlled Analgesia in a Patient with CRPS: A case report