J Rheum Dis.
2023 Jul;30(3):198-203. 10.4078/jrd.2023.0021.
Rosuvastatin treatment alone cannot alleviate lupus in murine model: a pilot study
- Affiliations
-
- 1Department of Molecular Science and Technology, Ajou University, Suwon, Korea
- 2Department of Rheumatology, Ajou University School of Medicine, Suwon, Korea
- KMID: 2543946
- DOI: http://doi.org/10.4078/jrd.2023.0021
Abstract
Objective
Systemic lupus erythematosus (SLE) is an autoimmune disease, characterized by the production of autoantibodies and high cholesterol levels. HMG-CoA (3-hydroxy-3-methylglutaryl-coenzyme A) reductase inhibitors have exhibited anti-inflammatory effects in several clinical trials. We conducted this study to evaluate the effect of rosuvastatin on inflammatory responses in lupus-prone mice.
Methods
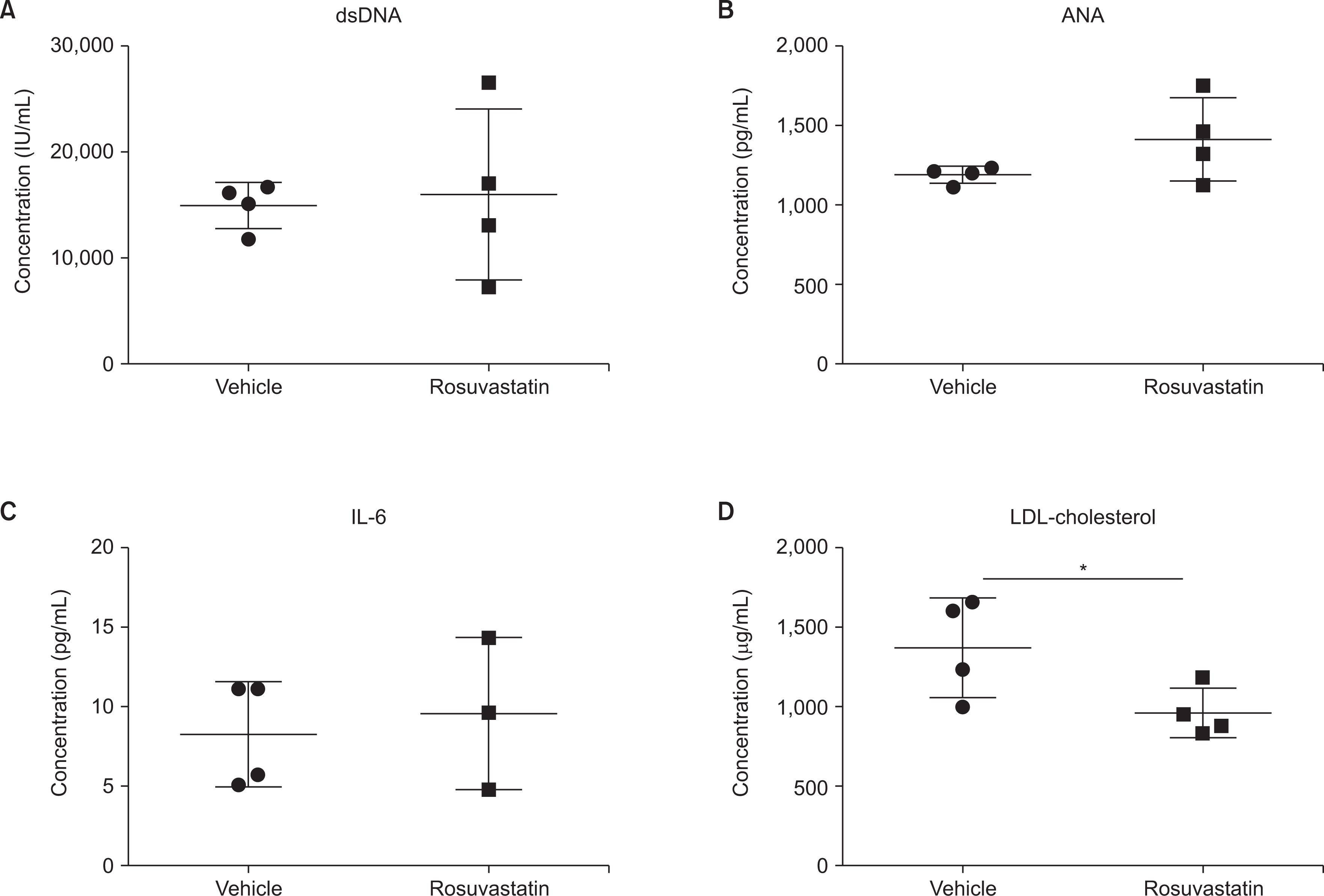
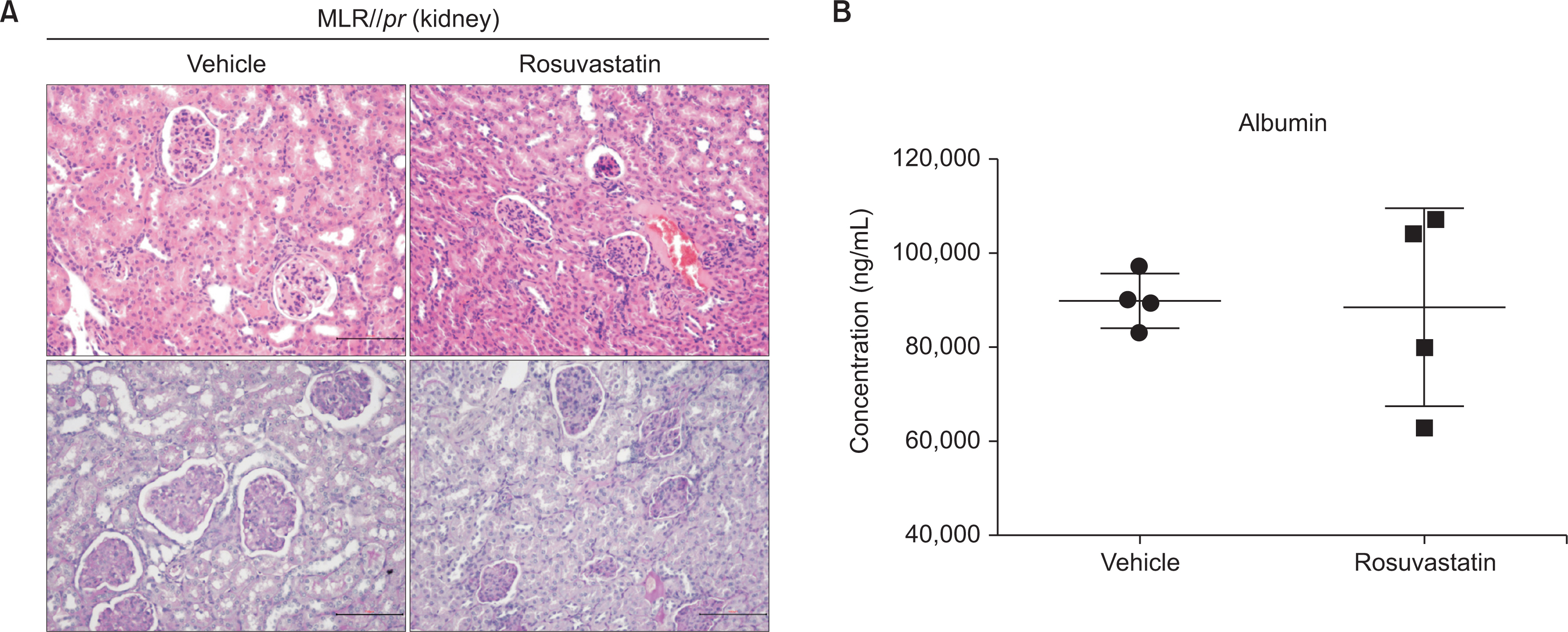
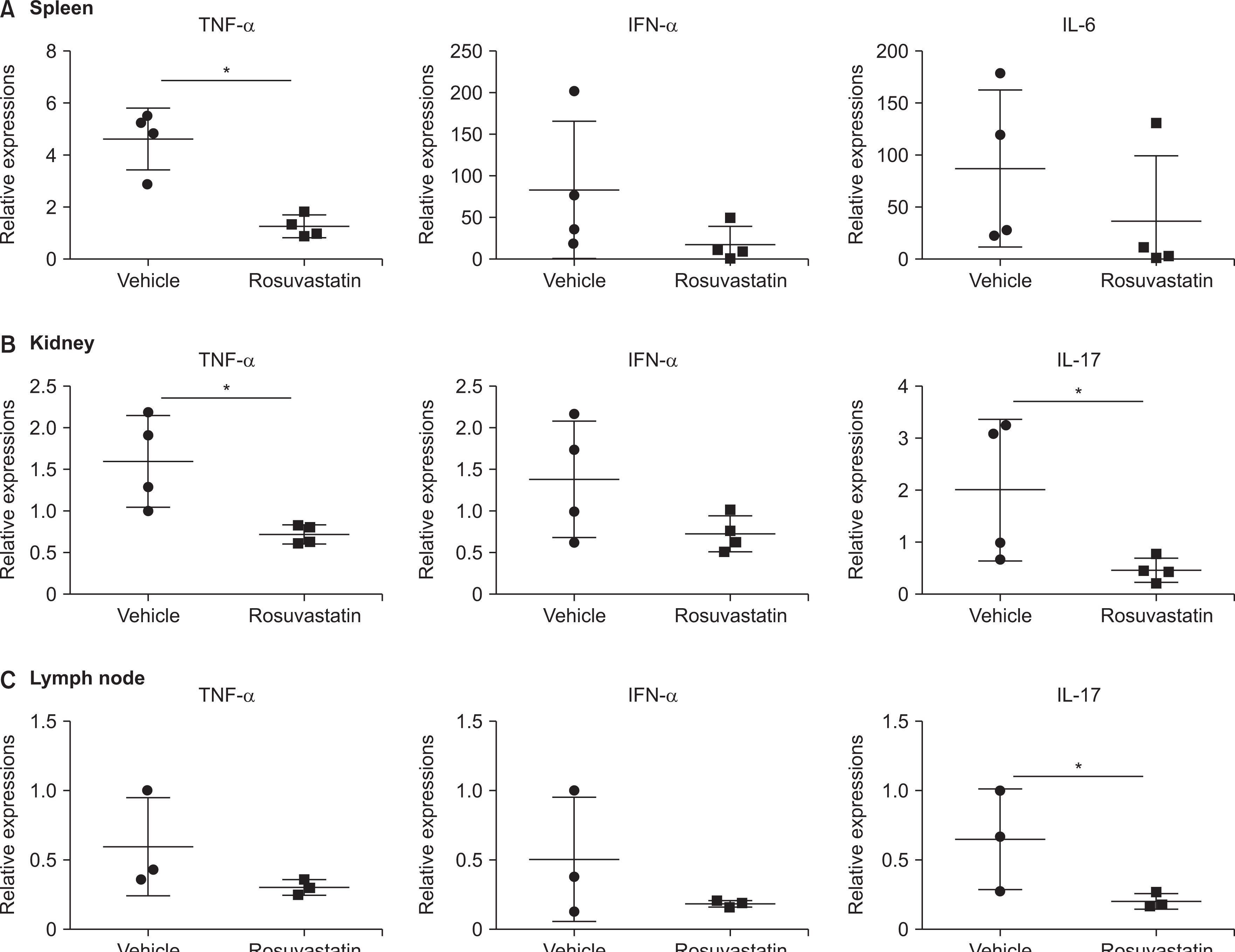
MRL/lpr mice were intraperitoneally injected with rosuvastatin (10 mg/kg, n=4) or vehicle (2% dimethyl sulfoxide, n=4) five times a week from 13 to 17 weeks of age. The serum levels of low-density lipoprotein (LDL) cholesterol and autoantibodies were measured, as well as the urine levels of albumin. Renal tissues were stained for histopathological analysis. Concentrations of key inflammatory cytokines were measured in the serum, and messenger RNA (mRNA) levels in target organs (kidney, spleen, and lymph nodes) were evaluated.
Results
Rosuvastatin treatment significantly decreased serum LDL cholesterol concentration in MRL/lpr mice. However, the clinical manifestations and autoantibody titres did not improve with rosuvastatin treatment. In addition, serum inflammatory cytokines and proteinuria did not change. Histopathological analysis of the kidneys revealed no improvement. When assessing the expression of mRNA, treatment with rosuvastatin decreased tumor necrosis alpha and interleukin-17 concentration in spleen and kidney tissue and in the kidneys and lymph nodes of MRL/lpr mice, respectively.
Conclusion
Although it can decrease inflammatory cytokines in the lymphoid organs and kidneys of MRL/lpr mice, treatment with rosuvastatin is insufficient to alleviate SLE.
Figure
Reference
-
1. D'Cruz DP, Khamashta MA, Hughes GR. 2007; Systemic lupus erythematosus. Lancet. 369:587–96. DOI: 10.1016/S0140-6736(07)60279-7. PMID: 17307106.2. Isenberg DA, Manson JJ, Ehrenstein MR, Rahman A. 2007; Fifty years of anti-ds DNA antibodies: are we approaching journey's end? Rheumatology (Oxford). 46:1052–6. DOI: 10.1093/rheumatology/kem112. PMID: 17500073.
Article3. Elkon K, Casali P. 2008; Nature and functions of autoantibodies. Nat Clin Pract Rheumatol. 4:491–8. DOI: 10.1038/ncprheum0895. PMID: 18756274. PMCID: PMC2703183.
Article4. Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. 1982; The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 25:1271–7. DOI: 10.1002/art.1780251101. PMID: 7138600.
Article5. Almaani S, Meara A, Rovin BH. 2017; Update on lupus nephritis. Clin J Am Soc Nephrol. 12:825–35. DOI: 10.2215/CJN.05780616. PMID: 27821390. PMCID: PMC5477208.
Article6. Gasparin AA, Pamplona Bueno de Andrade N, Hax V, Tres GL, Veronese FV, Monticielo OA. 2019; Urinary biomarkers for lupus nephritis: the role of the vascular cell adhesion molecule-1. Lupus. 28:265–72. DOI: 10.1177/0961203319826695. PMID: 30712490.
Article7. Ytterberg SR, Schnitzer TJ. 1982; Serum interferon levels in patients with systemic lupus erythematosus. Arthritis Rheum. 25:401–6. DOI: 10.1002/art.1780250407. PMID: 6176248.
Article8. Ohl K, Tenbrock K. 2011; Inflammatory cytokines in systemic lupus erythematosus. J Biomed Biotechnol. 2011:432595. DOI: 10.1155/2011/432595. PMID: 22028588. PMCID: PMC3196871.
Article9. Sinicato NA, da Silva Cardoso PA, Appenzeller S. 2013; Risk factors in cardiovascular disease in systemic lupus erythematosus. Curr Cardiol Rev. 9:15–9. DOI: 10.2174/1573403X11309010003.
Article10. Schönbeck U, Libby P. 2004; Inflammation, immunity, and HMG-CoA reductase inhibitors: statins as antiinflammatory agents? Circulation. 109(21 Suppl 1):II18–26. DOI: 10.1161/01.CIR.0000129505.34151.23. PMID: 15173059.11. Musial J, Undas A, Gajewski P, Jankowski M, Sydor W, Szczeklik A. 2001; Anti-inflammatory effects of simvastatin in subjects with hypercholesterolemia. Int J Cardiol. 77:247–53. DOI: 10.1016/S0167-5273(00)00439-3. PMID: 11182189.
Article12. White CM. 2002; A review of the pharmacologic and pharmacokinetic aspects of rosuvastatin. J Clin Pharmacol. 42:963–70. DOI: 10.1177/009127000204200902. PMID: 12211221.
Article13. Lu X, Wang Y, Zhang J, Pu D, Hu N, Luo J, et al. 2021; Patients with systemic lupus erythematosus face a high risk of cardiovascular disease: a systematic review and Meta-analysis. Int Immunopharmacol. 94:107466. DOI: 10.1016/j.intimp.2021.107466. PMID: 33636561.
Article14. Corsini A, Bellosta S, Baetta R, Fumagalli R, Paoletti R, Bernini F. 1999; New insights into the pharmacodynamic and pharmacokinetic properties of statins. Pharmacol Ther. 84:413–28. Erratum. DOI: 10.1016/S0163-7258(99)00045-5. PMID: 10665838.
Article15. de Pádua Borges R, Degobi NAH, Bertoluci MC. 2021; Choosing statins: a review to guide clinical practice. Arch Endocrinol Metab. 64:639–53. DOI: 10.20945/2359-3997000000306.16. Lawman S, Mauri C, Jury EC, Cook HT, Ehrenstein MR. 2004; Atorvastatin inhibits autoreactive B cell activation and delays lupus development in New Zealand black/white F1 mice. J Immunol. 173:7641–6. DOI: 10.4049/jimmunol.173.12.7641. PMID: 15585892.
Article17. Aprahamian T, Bonegio R, Rizzo J, Perlman H, Lefer DJ, Rifkin IR, et al. 2006; Simvastatin treatment ameliorates autoimmune disease associated with accelerated atherosclerosis in a murine lupus model. J Immunol. 177:3028–34. DOI: 10.4049/jimmunol.177.5.3028. PMID: 16920939. PMCID: PMC2752011.
Article18. Graham KL, Lee LY, Higgins JP, Steinman L, Utz PJ, Ho PP. 2008; Failure of oral atorvastatin to modulate a murine model of systemic lupus erythematosus. Arthritis Rheum. 58:2098–104. DOI: 10.1002/art.23605. PMID: 18576356. PMCID: PMC4143381.
Article19. Inaba K, Inaba M, Romani N, Aya H, Deguchi M, Ikehara S, et al. 1992; Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med. 176:1693–702. DOI: 10.1084/jem.176.6.1693. PMID: 1460426. PMCID: PMC2119469.
Article20. O'Grady S, Crown J, Duffy MJ. 2022; Statins inhibit proliferation and induce apoptosis in triple-negative breast cancer cells. Med Oncol. 39:142. DOI: 10.1007/s12032-022-01733-9. PMID: 35834073. PMCID: PMC9283343.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mixed?effects analysis of increased rosuvastatin absorption by coadministered telmisartan
- Rosuvastatin-induced Generalized Drug Eruption
- Physiologically-based pharmacokinetic predictions of intestinal BCRP-mediated drug interactions of rosuvastatin in Koreans
- Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)
- Response: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)