Anesth Pain Med.
2023 Apr;18(2):190-197. 10.17085/apm.23005.
Wound infiltration or transversus abdominis plane block after laparoscopic radical prostatectomy: a randomized clinical trial
- Affiliations
-
- 1Departmentsof Anesthesiology, Hospital de Sant Joan Despí Moisès Broggi, Sant Joan Despí, Barcelona, Spain
- 2Department of Surgery, Hospital de Sant Joan Despí Moisès Broggi, Sant Joan Despí, Barcelona, Spain
- KMID: 2543660
- DOI: http://doi.org/10.17085/apm.23005
Abstract
- Background
Regional anesthesia techniques are commonly used for postoperative pain management during laparoscopic surgery. Our aim was to compare the analgesic efficacy of pre-incisional subcutaneous wound infiltration (WI) with that of the transversus abdominis plane (TAP) block as part of a multimodal analgesic approach in laparoscopic radical prostatectomy.
Methods
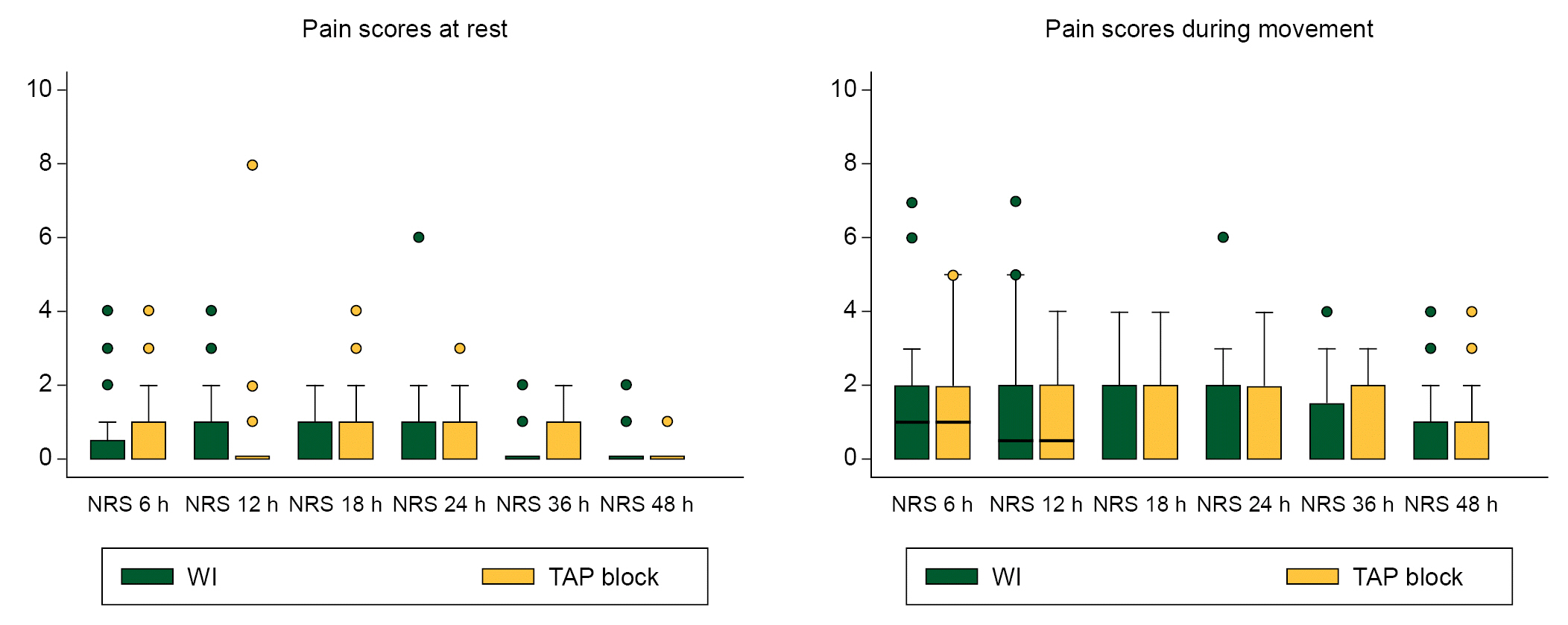
In this prospective, double-blinded, randomized controlled clinical trial, 60 patients were assigned to either TAP or WI group. The main outcome was acute postoperative pain control assessed using the mean numeric rating scale (NRS) at the 24 hours postoperatively. The secondary outcomes were opioid requirements, procedure-related complications, overall complications, and length of stay.
Results
In this study, 60 patients were randomized: 30 to TAP group and 28 to WI (two were excluded due to conversion to open surgery). We found no significant difference in the median (1Q, 3Q) NRS scores during the 24 h postoperatively neither at rest (TAP, 0 (0, 1) vs. WI, 0 (0, 1), P = 0.812), nor during movement (TAP, 1 (0, 2) vs. WI, 1 (0, 2), P = 0.708). There were no statistical differences in the postoperative intravenous morphine requirements in the TAP vs. WI groups during the same period (1.7 ± 3.1 vs. 1.8 ± 4.1 mg; P = 0.910). Only one patient in the TAP group presented with postoperative nausea and vomiting.
Conclusions
Both pre-incisional subcutaneous WI and TAP blockade were associated with very low pain scores as part of a non-opioid multimodal analgesic regimen in laparoscopic radical prostatectomy. This study did not demonstrate the benefits of WI over TAP.
Keyword
Figure
Reference
-
1. Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, Frydenberg M. Laparoscopic and robot-assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int. 2018; 121:845–53.
Article2. Wagenhoffer R, Gruner M, Schymik J, Schachtner L, Neagoe L, Berg C, et al. Switching from endoscopic extraperitoneal radical prostatectomy to robot-assisted laparoscopic prostatectomy: comparing outcomes and complications. Urol Int. 2015; 95:380–5.
Article3. Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001; 90:261–9.
Article4. Joshi GP, Rawal N, Kehlet H, Bonnet F, Camu F, Fischer HB, et al. Evidence-based management of postoperative pain in adults undergoing open inguinal hernia surgery. Br J Surg. 2012; 99:168–85.
Article5. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017; 152:691–7.
Article6. Petersen PL, Mathiesen O, Torup H, Dahl JB. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010; 54:529–35.
Article7. Rashid A, Gorissen KJ, Ris F, Gosselink MP, Shorthouse JR, Smith AD, et al. No benefit of ultrasound-guided transversus abdominis plane blocks over wound infiltration with local anaesthetic in elective laparoscopic colonic surgery: results of a double-blind randomized controlled trial. Colorectal Dis. 2017; 19:681–9.
Article8. Skjelsager A, Ruhnau B, Kistorp TK, Kridina I, Hvarness H, Mathiesen O, et al. Transversus abdominis plane block or subcutaneous wound infiltration after open radical prostatectomy: a randomized study. Acta Anaesthesiol Scand. 2013; 57:502–8.
Article9. Lancaster P, Chadwick M. Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010; 104:509–10.
Article10. Frigon C, Mai R, Valois-Gomez T, Desparmet J. Bowel hematoma following an iliohypogastric-ilioinguinal nerve block. Paediatr Anaesth. 2006; 16:993–6.
Article11. Jankovic Z, Ahmad N, Ravishankar N, Archer F. Transversus abdominis plane block: how safe is it? Anesth Analg. 2008; 107:1758–9.
Article12. Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015; 121:1640–54.13. El-Boghdadly K, Nair G, Pawa A, Onwochei DN. Impact of parallel processing of regional anesthesia with block rooms on resource utilization and clinical outcomes: a systematic review and meta-analysis. Reg Anesth Pain Med. 2020; 45:720–6.
Article14. Coughlin SM, Karanicolas PJ, Emmerton-Coughlin HM, Kanbur B, Kanbur S, Colquhoun PH. Better late than never? Impact of local analgesia timing on postoperative pain in laparoscopic surgery: a systematic review and metaanalysis. Surg Endosc. 2010; 24:3167–76.
Article15. Taha T, Sionov BV, Rosenberg P, Stein A, Tsivian M, Sidi A, et al. Pain control after laparoscopic radical prostatectomy: comparison between unilateral transversus abdominis plane block and wound infiltration. Urol Int. 2019; 103:19–24.
Article16. Park JS, Choi GS, Kwak KH, Jung H, Jeon Y, Park S, et al. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res. 2015; 195:61–6.
Article17. Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012; 37:188–92.
Article18. Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. European Palliative Care Research Collaborative (EPCRC). Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011; 41:1073–93.19. Kargar R, Minas V, Gorgin-Karaji A, Shadjoo K, Padmehr R, Mohazzab A, et al. Transversus abdominis plane block under laparoscopic guide versus port-site local anaesthetic infiltration in laparoscopic excision of endometriosis: a double-blind randomised placebo-controlled trial. BJOG. 2019; 126:647–54.
Article20. Rodrigues Pessoa R, Urkmez A, Kukreja N, Baack Kukreja J. Enhanced recovery after surgery review and urology applications in 2020. BJUI Compass. 2020; 1:5–14.
Article21. Stamenkovic DM, Bezmarevic M, Bojic S, Unic-Stojanovic D, Stojkovic D, Slavkovic DZ, et al. Updates on wound infiltration use for postoperative pain management: a narrative review. J Clin Med. 2021; 10:4659.22. Kato J, Ogawa S, Katz J, Nagai H, Kashiwazaki M, Saeki H, et al. Effects of presurgical local infiltration of bupivacaine in the surgical field on postsurgical wound pain in laparoscopic gynecologic examinations: a possible preemptive analgesic effect. Clin J Pain. 2000; 16:12–7.23. Hasaniya NW, Zayed FF, Faiz H, Severino R. Preinsertion local anesthesia at the trocar site improves perioperative pain and decreases costs of laparoscopic cholecystectomy. Surg Endosc. 2001; 15:962–4.24. Erdogru T, Teber D, Frede T, Marrero R, Hammady A, Seemann O, et al. Comparison of transperitoneal and extraperitoneal laparoscopic radical prostatectomy using match-pair analysis. Eur Urol. 2004; 46:312–9; discussion 320.25. Apfel CC, Turan A, Souza K, Pergolizzi J, Hornuss C. Intravenous acetaminophen reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain. 2013; 154:677–89.26. Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013; 111:721–35.
Article27. Guignard B. Monitoring analgesia. Best Pract Res Clin Anaesthesiol. 2006; 20:161–80.
Article28. Ventham NT, O'Neill S, Johns N, Brady RR, Fearon KC. Evaluation of novel local anesthetic wound infiltration techniques for postoperative pain following colorectal resection surgery: a meta-analysis. Dis Colon Rectum. 2014; 57:237–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response to "Comment on Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"
- Comment on "Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"
- Analgesic efficacy of ultrasound-guided transversus abdominis plane block for laparoscopic gynecological surgery: a randomized controlled trial
- Comparison of the effectiveness of subcostal transversus abdominis plane and rectus sheath blocks in postoperative analgesia in major open gynecological cancer surgeries: a prospective randomized study
- Transversus abdominis plane block as a sole anesthetic technique for evacuation of rectus abdominis muscle hematoma - A case report -