Anesth Pain Med.
2022 Jan;17(1):67-74. 10.17085/apm.21030.
Analgesic efficacy of ultrasound-guided transversus abdominis plane block for laparoscopic gynecological surgery: a randomized controlled trial
- Affiliations
-
- 1Department of Anesthesia and Critical Care, Employees’ State Insurance Cooperation Postgraduate Institute of Medical Sciences and Research (ESIC-PGIMSR), New Delhi, India
- KMID: 2526530
- DOI: http://doi.org/10.17085/apm.21030
Abstract
- Background
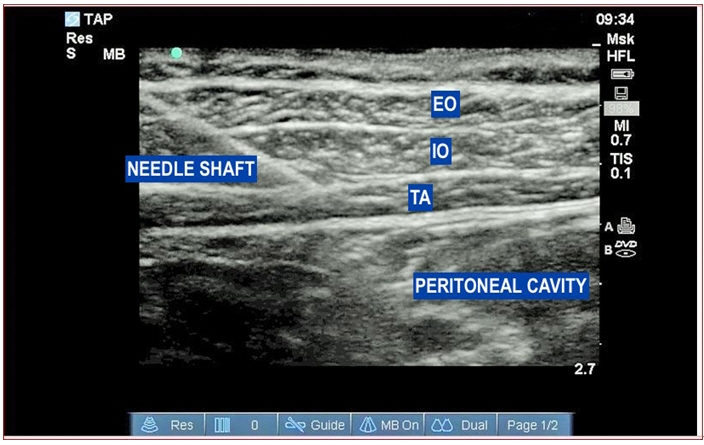
This study aimed to determine whether ultrasound-guided transversus abdominis plane (TAP) block is more effective in reducing postoperative pain and analgesic consumption than local anesthetic infiltration (LAI) at the port site for elective laparoscopic gynecological surgeries.
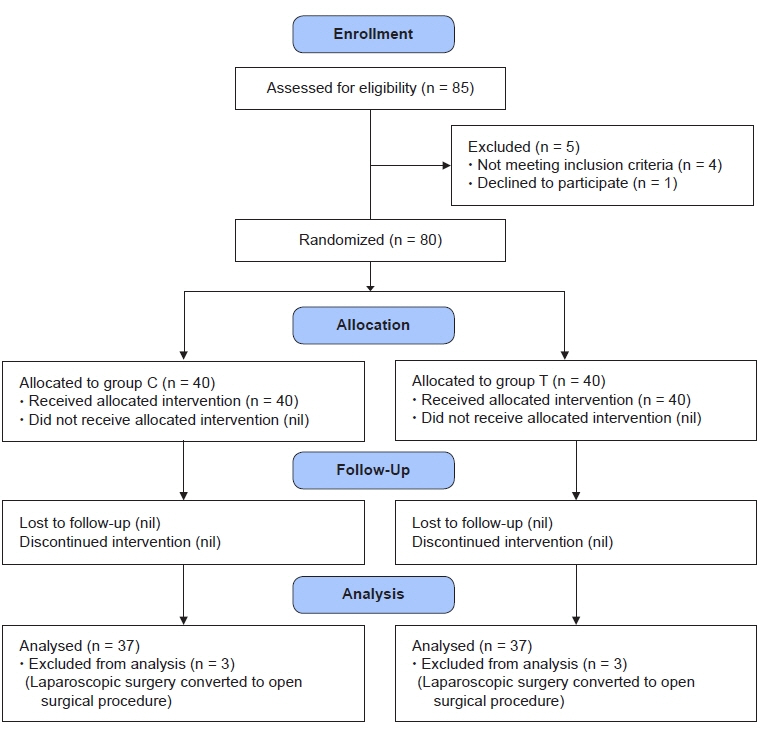
Methods
Eighty patients with the American Society of Anesthesiologists status I/II undergoing laparoscopic gynecology surgery were enrolled for this randomized control trial. After general anesthesia was administered, patients in group C received LAI at each port site, and patients in group T received bilateral ultrasound-guided TAP. Postoperative pain was assessed at time intervals of 1/2, 2, 4, 6, 8, and 24 h using the numeric pain scale (NPS). Clinical metrics such as postoperative analgesic diclofenac consumption, need for rescue fentanyl, nausea-vomiting scores, and antiemetic requirements were also recorded.
Results
Seventy-four patients were included in the final analysis. Postoperatively, patients in group T had significantly lower NPS than those in group C (P < 0.05). The highest difference in the postoperative NPS was observed at 2 h (median [1Q, 3Q]; group C = 3 [2, 4]; group T = 1 [0, 2]; P < 0.001). A statistically significant difference was observed in the frequency of diclofenac (75 mg intravenous) requirement between the groups (P = 0.010). No significant difference was observed between the groups in need of rescue fentanyl or antiemetic and the nausea-vomiting scores.
Conclusions
In patients undergoing laparoscopic gynecological surgery, ultrasound-guided TAP block provided greater postoperative analgesic benefits in terms of lower NPS and reduced analgesic requirements than port site LAI.
Figure
Reference
-
1. Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997; 79:369–78.2. Golzari SE, Nader ND, Mahmoodpoor A. Underlying mechanisms of postoperative pain after laparoscopic surgery. JAMA Surg. 2016; 151:295–6.3. Coughlin SM, Karanicolas PJ, Emmerton-Coughlin HM, Kanbur B, Kanbur S, Colquhoun PH. Better late than never? Impact of local analgesia timing on postoperative pain in laparoscopic surgery: a systematic review and metaanalysis. Surg Endosc. 2010; 24:3167–76.4. Marks JL, Ata B, Tulandi T. Systematic review and metaanalysis of intraperitoneal instillation of local anesthetics for reduction of pain after gynecologic laparoscopy. J Minim Invasive Gynecol. 2012; 19:545–53.5. Petersen PL, Mathiesen O, Torup H, Dahl JB. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010; 54:529–35.6. Lissauer J, Mancuso K, Merritt C, Prabhakar A, Kaye AD, Urman RD. Evolution of the transversus abdominis plane block and its role in postoperative analgesia. Best Pract Res Clin Anaesthesiol. 2014; 28:117–26.7. Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015; 121:1640–54.8. Koh WU, Lee JH. Ultrasound-guided truncal blocks for perioperative analgesia. Anesth Pain Med. 2018; 13:128–42.9. De Oliveira GS Jr, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2014; 118:454–63.10. Calle GA, López CC, Sánchez E, De Los Ríos JF, Vásquez EM, Serna E, et al. Transversus abdominis plane block after ambulatory total laparoscopic hysterectomy: randomized controlled trial. Acta Obstet Gynecol Scand. 2014; 93:345–50.11. Kane SM, Garcia-Tomas V, Alejandro-Rodriguez M, Astley B, Pollard RR. Randomized trial of transversus abdominis plane block at total laparoscopic hysterectomy: effect of regional analgesia on quality of recovery. Am J Obstet Gynecol. 2012; 207:419. e1-5.12. Kawahara R, Tamai Y, Yamasaki K, Okuno S, Hanada R, Funato T. The analgesic efficacy of ultrasound-guided transversus abdominis plane block with mid-axillary approach after gynecologic laparoscopic surgery: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015; 31:67–71.13. De Oliveira GS Jr, Fitzgerald PC, Marcus RJ, Ahmad S, McCarthy RJ. A dose-ranging study of the effect of transversus abdominis block on postoperative quality of recovery and analgesia after outpatient laparoscopy. Anesth Analg. 2011; 113:1218–25.14. El Hachem L, Small E, Chung P, Moshier EL, Friedman K, Fenske SS, et al. Randomized controlled double-blind trial of transversus abdominis plane block versus trocar site infiltration in gynecologic laparoscopy. Am J Obstet Gynecol. 2015; 212:182. e1-9.15. Sugihara M, Miyake T, Miyagi Y, Oda T, Hazama Y, Sano R, et al. Does local infiltration anesthesia on laparoscopic surgical wounds reduce postoperative pain? Randomized control study. Reprod Med Biol. 2018; 17:474–80.16. Selcuk S, Api M, Polat M, Arinkan A, Aksoy B, Akca T, et al. Effectiveness of local anesthetic on postoperative pain in different levels of laparoscopic gynecological surgery. Arch Gynecol Obstet. 2016; 293:1279–85.17. Pellicano M, Zullo F, Di Carlo C, Zupi E, Nappi C. Postoperative pain control after microlaparoscopy in patients with infertility: a prospective randomized study. Fertil Steril. 1998; 70:289–92.18. Ceyhan T, Teksoz E, Gungor S, Goktolga U, Pabuccu R. Effect of bupivacaine after operative laparoscopic gynecologic procedures. J Minim Invasive Gynecol. 2005; 12:326–9.19. Ghezzi F, Cromi A, Bergamini V, Raffaelli R, Crotti S, Segredini R, et al. Preemptive port site local anesthesia in gynecologic laparoscopy: a randomized, controlled trial. J Minim Invasive Gynecol. 2005; 12:210–5.20. Tam T, Harkins G, Wegrzyniak L, Ehrgood S, Kunselman A, Davies M. Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol. 2014; 21:1015–21.21. Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014; 14:121.22. Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013; 111:721–35.23. McDonnell JG, O'Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007; 32:399–404.24. Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011; 66:1023–30.25. Støving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrøm LH, Lange KH. Cutaneous sensory block area, muscle-relaxing effect, and block duration of the transversus abdominis plane block: a randomized, blinded, and placebo-controlled study in healthy volunteers. Reg Anesth Pain Med. 2015; 40:355–62.26. Gadsden J, Ayad S, Gonzales JJ, Mehta J, Boublik J, Hutchins J. Evolution of transversus abdominis plane infiltration techniques for postsurgical analgesia following abdominal surgeries. Local Reg Anesth. 2015; 8:113–7.27. Chen Q, Liu X, Zhong X, Yang B. Addition of dexmedetomidine or fentanyl to ropivacaine for transversus abdominis plane block: evaluation of effect on postoperative pain and quality of recovery in gynecological surgery. J Pain Res. 2018; 11:2897–903.28. Xue Y, Yuan H, Chen Y. Effects of dexmedetomidine as an adjunct in transversus abdominis plane block during gynecological laparoscopy. Exp Ther Med. 2018; 16:1131–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response to "Comment on Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"
- Comment on "Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"
- Wound infiltration or transversus abdominis plane block after laparoscopic radical prostatectomy: a randomized clinical trial
- A comparison of analgesic efficacy between oblique subcostal transversus abdominis plane block and intravenous morphine for laparascopic cholecystectomy. A prospective randomized controlled trial
- Transversus abdominis plane block as a sole anesthetic technique for evacuation of rectus abdominis muscle hematoma - A case report -