Anesth Pain Med.
2023 Apr;18(2):123-131. 10.17085/apm.23014.
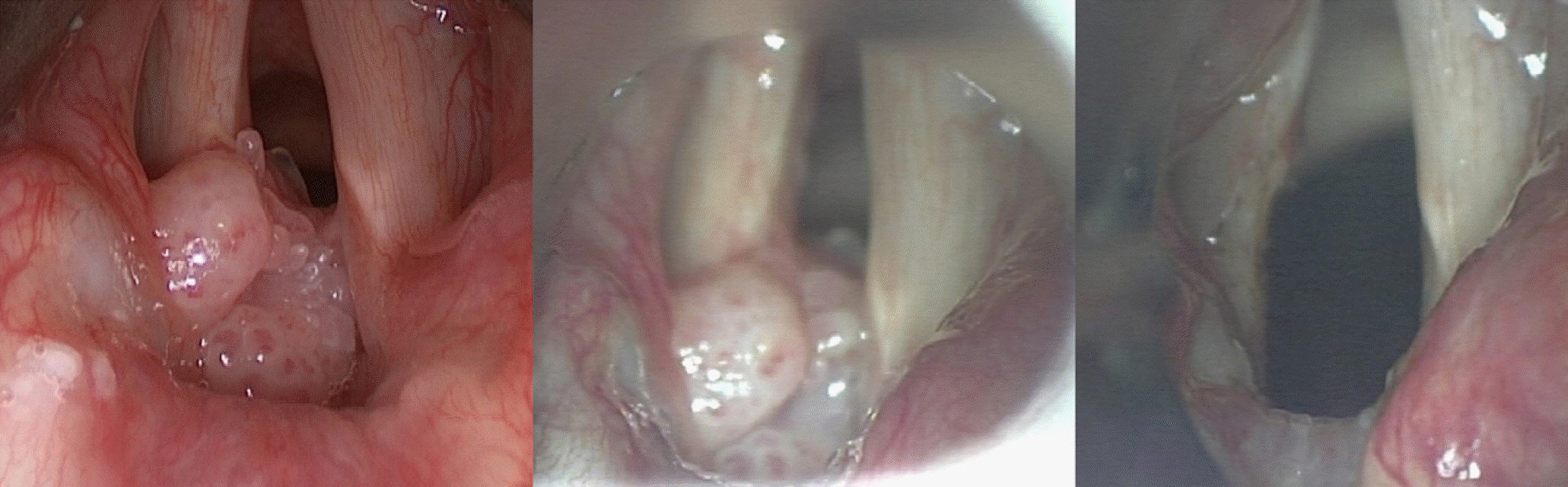
Tube or tubeless: an anesthetic strategy for upper airway surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2543653
- DOI: http://doi.org/10.17085/apm.23014
Abstract
- Since the patient’s airway is shared between an anesthesiologist and a surgeon, airway management during upper airway surgery can be challenging. Beyond the conventional method of general anesthesia, high-flow nasal oxygenation (HFNO) has recently been used as a key technique for tubeless anesthesia. HFNO provides humidified, heated oxygen up to 70 L/min, which promises improved oxygenation and ventilation, allowing for prolonged apneic oxygenation. In previous physiological and clinical studies, HFNO has been demonstrated that tubeless anesthesia safely provide an uninterrupted surgical field during laryngeal surgeries. Although tubeless anesthesia remains uncommon, it can be a good alternative to conventional anesthesia if an anesthesiologist and a surgeon select appropriate patients together with sufficient experience. A safe strategy for tubeless anesthesia, along with appropriate backup plans, including endotracheal intubation and high-frequency jet ventilation, should be considered for upper airway surgery.
Figure
Reference
-
1. Gleason JM, Christian BR, Barton ED. Nasal cannula apneic oxygenation prevents desaturation during endotracheal intubation: an integrative literature review. West J Emerg Med. 2018; 19:403–11.
Article2. Hua Z, Liu Z, Li Y, Zhang H, Yang M, Zuo M. Transnasal humidified rapid insufflation ventilatory exchange vs. facemask oxygenation in elderly patients undergoing general anaesthesia: a randomized controlled trial. Sci Rep. 2020; 10:5745.
Article3. Kim HJ, Asai T. High-flow nasal oxygenation for anesthetic management. Korean J Anesthesiol. 2019; 72:527–47.
Article4. Lee SJ, Quek KH. Facilitating airway surgery in a morbidly obese patient using transnasal humidified rapid insufflation ventilatory exchange (THRIVE). Case Rep Anesthesiol. 2018; 2018:5310342.
Article5. Lodenius Å, Piehl J, Östlund A, Ullman J, Jonsson Fagerlund M. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) vs. facemask breathing pre-oxygenation for rapid sequence induction in adults: a prospective randomised non-blinded clinical trial. Anaesthesia. 2018; 73:564–71.
Article6. Benninger MS, Zhang ES, Chen B, Tierney WS, Abdelmalak B, Bryson PC. Utility of transnasal humidified rapid insufflation ventilatory exchange for microlaryngeal surgery. Laryngoscope. 2021; 131:587–91.
Article7. Bharathi MB, Kumar MRA, Prakash BG, Shetty S, Sivapuram K, Madhan S. New visionary in upper airway surgeries-THRIVE, a tubeless ventilation. Indian J Otolaryngol Head Neck Surg. 2021; 73:246–51.
Article8. Gustafsson IM, Lodenius Å, Tunelli J, Ullman J, Jonsson Fagerlund M. Apnoeic oxygenation in adults under general anaesthesia using transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) - a physiological study. Br J Anaesth. 2017; 118:610–7.
Article9. Lyons C, Callaghan M. Apnoeic oxygenation with high-flow nasal oxygen for laryngeal surgery: a case series. Anaesthesia. 2017; 72:1379–87.
Article10. Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015; 70:323–9.
Article11. Min SH, Yoon H, Huh G, Kwon SK, Seo JH, Cho YJ. Efficacy of high-flow nasal oxygenation compared with tracheal intubation for oxygenation during laryngeal microsurgery: a randomised non-inferiority study. Br J Anaesth. 2022; 128:207–13.
Article12. To K, Harding F, Scott M, Milligan P, Nixon IJ, Adamson R, et al. The use of transnasal humidified rapid-insufflation ventilatory exchange in 17 cases of subglottic stenosis. Clin Otolaryngol. 2017; 42:1407–10.13. Waters E, Kellner M, Milligan P, Adamson RM, Nixon IJ, McNarry AF. The use of transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) in one hundred and five upper airway endoscopies. A case series. Clin Otolaryngol. 2019; 44:1115–9.14. Huh G, Min SH, Cho SD, Cho YJ, Kwon SK. Application and efficiency of transnasal humidified rapid-insufflation ventilatory exchange in laryngeal microsurgery. Laryngoscope. 2022; 132:1061–8.15. Aloy A, Schachner M, Cancura W. Tubeless translaryngeal superimposed jet ventilation. Eur Arch Otorhinolaryngol. 1991; 248:475–8.16. Babinski M, Smith RB, Klain M. High-frequency jet ventilation for laryngoscopy. Anesthesiology. 1980; 52:178–80.
Article17. Klain M, Keszler H. High-frequency jet ventilation. Surg Clin North Am. 1985; 65:917–30.
Article18. Janjević D, Jović R. [High frequency jet ventilation and laryngeal surgery, clinical practice]. Med Pregl. 2008; 61 Suppl 2:57–61. Serbian.19. Payne JP. Apnoeic oxygenation in anaesthetised man. Acta Anaesthesiol Scand. 1962; 6:129–42.
Article20. Frumin MJ, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology. 1959; 20:789–98.
Article21. Wong DT, Yee AJ, Leong SM, Chung F. The effectiveness of apneic oxygenation during tracheal intubation in various clinical settings: a narrative review. Can J Anaesth 2017; 64: 416-27. Erratum in: Can J Anaesth. 2017; 64:557.
Article22. O'Loughlin CJ, Phyland DJ, Vallance NA, Giddings C, Malkoutzis E, Gunasekera E, et al. Low-flow apnoeic oxygenation for laryngeal surgery: a prospective observational study. Anaesthesia. 2020; 75:1070–5.23. Eger EI, Severinghaus JW. The rate of rise of PaCO2 in the apneic anesthetized patient. Anesthesiology. 1961; 22:419–25.24. Spicuzza L, Schisano M. High-flow nasal cannula oxygen therapy as an emerging option for respiratory failure: the present and the future. Ther Adv Chronic Dis. 2020; 11:2040622320920106.
Article25. Drake MG. High-flow nasal cannula oxygen in adults: an evidence-based assessment. Ann Am Thorac Soc. 2018; 15:145–55.
Article26. Biselli P, Fricke K, Grote L, Braun AT, Kirkness J, Smith P, et al. Reductions in dead space ventilation with nasal high flow depend on physiological dead space volume: metabolic hood measurements during sleep in patients with COPD and controls. Eur Respir J. 2018; 51:1702251.
Article27. Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, et al. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015; 118:1525–32.
Article28. Rudlof B, Hohenhorst W. Use of apneic oxygenation for the performance of pan-endoscopy. Otolaryngol Head Neck Surg. 2013; 149:235–9.
Article29. Humphreys S, Lee-Archer P, Reyne G, Long D, Williams T, Schibler A. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) in children: a randomized controlled trial. Br J Anaesth. 2017; 118:232–8.
Article30. Huang L, Dharmawardana N, Badenoch A, Ooi EH. A review of the use of transnasal humidified rapid insufflation ventilatory exchange for patients undergoing surgery in the shared airway setting. J Anesth. 2020; 34:134–43.
Article31. Maupeu L, Raguin T, Hengen M, Diemunsch P, Schultz P. Indications of transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) in laryngoscopy, a prospective study of 19 cases. Clin Otolaryngol. 2019; 44:182–6.
Article32. Nekhendzy V, Saxena A, Mittal B, Sun E, Sung K, Dewan K, et al. The safety and efficacy of transnasal humidified rapid-insufflation ventilatory exchange for laryngologic surgery. Laryngoscope. 2020; 130:E874–81.
Article33. Tam K, Jeffery C, Sung CK. Surgical management of supraglottic stenosis using intubationless optiflow. Ann Otol Rhinol Laryngol. 2017; 126:669–72.
Article34. Yang SH, Wu CY, Tseng WH, Cherng WY, Hsiao TY, Cheng YJ, et al. Nonintubated laryngomicrosurgery with transnasal humidified rapid-insufflation ventilatory exchange: a case series. J Formos Med Assoc. 2019; 118:1138–43.
Article35. Srivastava R, Agarwal AC, Agarwal S, Pathak M. High flow nasal cannula: a game changer in airway surgery. Indian J Otolaryngol Head Neck Surg. 2019; 71:299–303.
Article36. Riva T, Seiler S, Stucki F, Greif R, Theiler L. High-flow nasal cannula therapy and apnea time in laryngeal surgery. Paediatr Anaesth. 2016; 26:1206–8.
Article37. Youssef DL, Paddle P. Tubeless anesthesia in subglottic stenosis: comparative review of apneic low-flow oxygenation with THRIVE. Laryngoscope. 2022; 132:1231–6.38. Booth AWG, Vidhani K, Lee PK, Coman SH, Pelecanos AM, Dimeski G, et al. The effect of high-flow nasal oxygen on carbon dioxide accumulation in apneic or spontaneously breathing adults during airway surgery: a randomized-controlled trial. Anesth Analg. 2021; 133:133–41.
Article39. Hermez LA, Spence CJ, Payton MJ, Nouraei SAR, Patel A, Barnes TH. A physiological study to determine the mechanism of carbon dioxide clearance during apnoea when using transnasal humidified rapid insufflation ventilatory exchange (THRIVE). Anaesthesia. 2019; 74:441–9.
Article40. Novakovic D, Sheth M, Fellner A, Zoszak A, Liew S, Nguyen DD. Microlaryngeal laser surgery using high-flow nasal ventilation at two oxygen concentration deliveries. Laryngoscope. 2023; 133:634–9.
Article41. Parameswaran K, Todd DC, Soth M. Altered respiratory physiology in obesity. Can Respir J. 2006; 13:203–10.
Article42. Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care. 2011; 56:1151–5.
Article43. Chang MY, Chen JH, Lin SP, Teng WN, Liao SW, Ting CK, et al. Fire safety study on high-flow nasal oxygen in shared-airway surgeries with diathermy and laser: simulation based on a physical model. J Clin Monit Comput. 2022; 36:649–55.
Article44. Baudouin R, Rigal T, Circiu M, Lechien JR, Couineau F, Guen MLE, et al. Feasibility and safety of THRIVE in transoral laser microsurgery. Am J Otolaryngol. 2022; 43:103605.
Article45. Reid CW, Martineau RJ, Miller DR, Hull KA, Baines J, Sullivan PJ. A comparison of transcutaneous end-tidal and arterial measurements of carbon dioxide during general anaesthesia. Can J Anaesth. 1992; 39:31–6.
Article46. Xue Q, Wu X, Jin J, Yu B, Zheng M. Transcutaneous carbon dioxide monitoring accurately predicts arterial carbon dioxide partial pressure in patients undergoing prolonged laparoscopic surgery. Anesth Analg. 2010; 111:417–20.
Article47. Casati A, Squicciarini G, Malagutti G, Baciarello M, Putzu M, Fanelli A. Transcutaneous monitoring of partial pressure of carbon dioxide in the elderly patient: a prospective, clinical comparison with end-tidal monitoring. J Clin Anesth 2006; 18: 436-40. Erratum in: J Clin Anesth. 2006; 18:559.48. Fujimoto S, Suzuki M, Sakamoto K, Ibusuki R, Tamura K, Shiozawa A, et al. Comparison of end-tidal, arterial, venous, and transcutaneous PCO2. Respir Care. 2019; 64:1208–14.
Article49. Yoshida K, Isosu T, Noji Y, Hasegawa M, Iseki Y, Oishi R, et al. Usefulness of oxygen reserve index (ORi™), a new parameter of oxygenation reserve potential, for rapid sequence induction of general anesthesia. J Clin Monit Comput. 2018; 32:687–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endotracheal Intubation Using Laryngeal Mask Airway in a Patient with a Difficult Airway: A case report
- A Comparative Study between Standard and Tubeless Percutaneous Nephrolithotomy
- Anesthetic Management for a Patient with a Silicon Tracheal T-tube
- Metric Study of Upper Airway and Trachea in Nomal Korean Adults uing Fiberoptic Bronchoscopy: Study of endotracheal tube fixation positioning in adults
- The use of the Montgomery T-tube in postprocedural subglottic stenosis repair