J Neurocrit Care.
2023 Jun;16(1):28-33. 10.18700/jnc.230011.
Delayed post-ischemic leukoencephalopathy in emergent large-vessel occlusive stroke after mechanical thrombectomy: case reports
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurology, Uijeongbu Eulji Medical Center, Eulji University School of Medicine, Uijeongbu, Korea
- 3Graduate School of Medicine, Kangwon National University, Chuncheon, Korea
- KMID: 2543389
- DOI: http://doi.org/10.18700/jnc.230011
Abstract
- Background
Delayed post-ischemic leukoencephalopathy (DPIL) is a rare complication after mechanical thrombectomy, with no well-established clinical characteristics and patho-mechanism. We explored the characteristics and possible mechanisms in three patients with DPIL.
Case Report
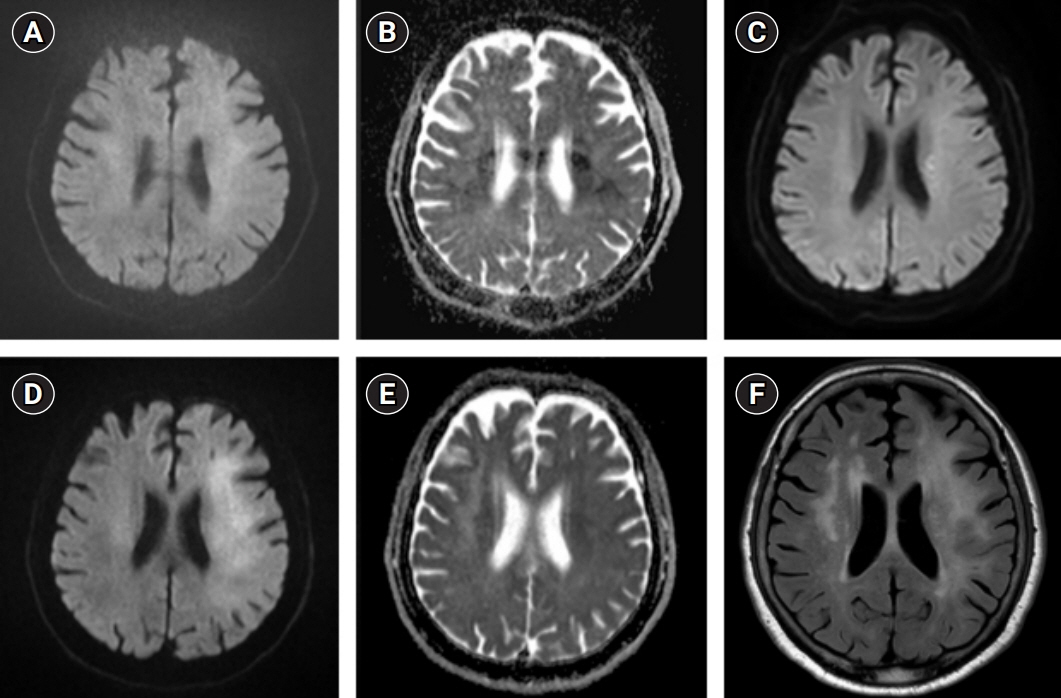
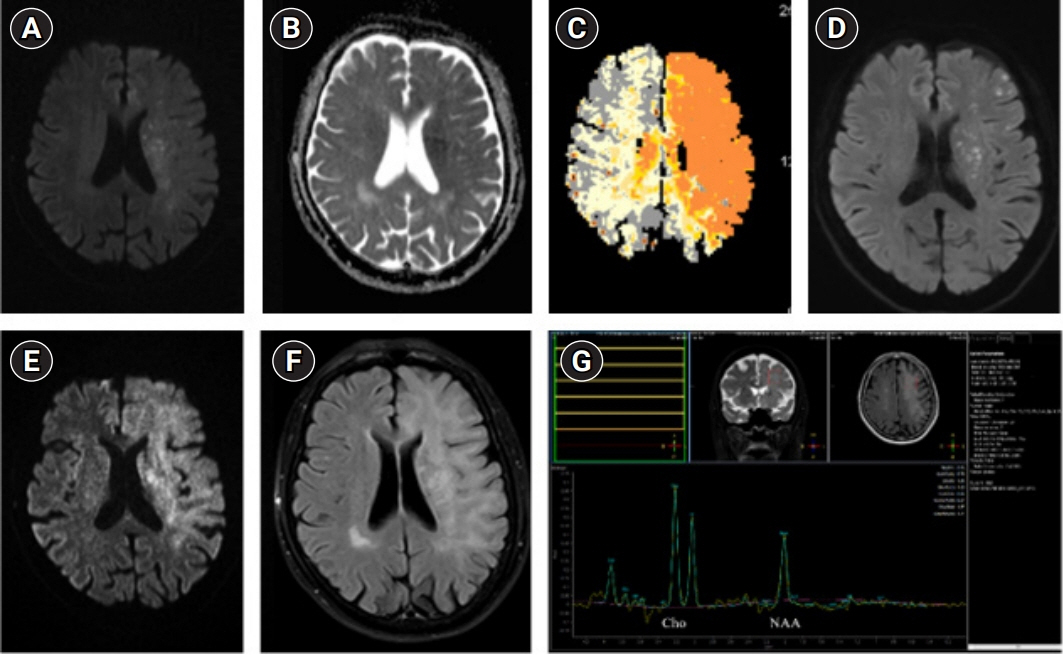
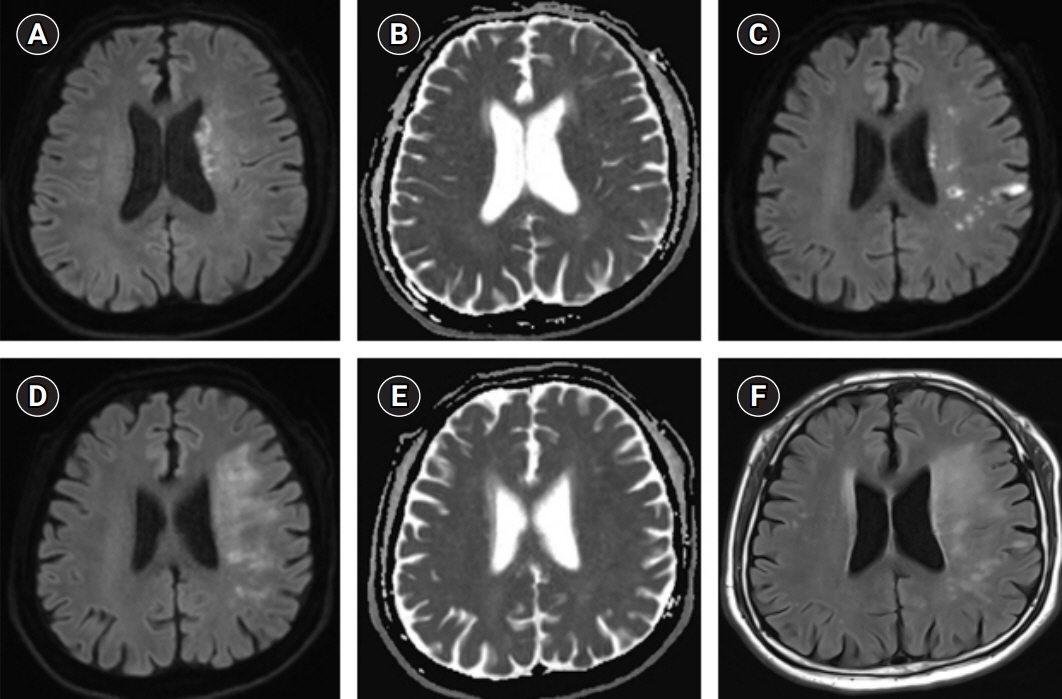
Based on the clinical manifestations and laboratory findings including magnetic-resonance imaging, magnetic resonance spectroscopy, electroencephalography, and lumbar puncture, DPIL was diagnosed in three patients. We administered antiplatelet agents and conservative treatment. Cardioembolism, successful recanalization using a balloon guiding catheter, and fluctuating or gradually worsening neurological symptoms in delayed phase between 13 and 70 days were common features of DPIL. Diffusion-weighted imaging and fluid-attenuated inversion recovery showed high-signal intensity in the affected subcortical white matter. Laboratory findings provided no evidence of an epileptic disorder, inflammatory demyelination, or tumorous conditions.
Conclusion
This report shows the characteristics and neuroradiologic images of DPIL. Among the various hypotheses, regional hypoxic-ischemic leukoencephalopathy and delayed reperfusion injury might be the patho-mechanism underlying DPIL.
Keyword
Figure
Reference
-
1. Sasaki T, Tomura N, Okada H, Tsuji E, Hayashi N, Kuwata T. A case of delayed white matter lesion after mechanical thrombectomy for middle cerebral artery occlusion. Jpn J Stroke. 2017; 40:270–4.2. Singu T, Inatomi Y, Yonehara T, Ando Y. Delayed leukoencephalopathy after recanalized cardioembolic stroke: two case reports. J Neurol Sci. 2017; 379:81–3.3. Nehme A, Pistono AA, Guilbert F, Stumpf É. Post-ischemic leukoencephalopathy after endovascular treatment for acute ischemic stroke. Can J Neurol Sci. 2019; 46:363–5.4. Iadecola C, Park L, Capone C. Threats to the mind: aging, amyloid, and hypertension. Stroke. 2009; 40(3 Suppl):S40–4.5. Zamora CA, Nauen D, Hynecek R, Ilica AT, Izbudak I, Sair HI, et al. Delayed posthypoxic leukoencephalopathy: a case series and review of the literature. Brain Behav. 2015; 5:e00364.6. Guglielmi V, LeCouffe NE, Zinkstok SM, Compagne KC, Eker R, Treurniet KM, et al. Collateral circulation and outcome in atherosclerotic versus cardioembolic cerebral large vessel occlusion. Stroke. 2019; 50:3360–8.7. Ferro JM. Cardioembolic stroke: an update. Lancet Neurol. 2003; 2:177–88.8. Lieb M, Shah U, Hines GL. Cerebral hyperperfusion syndrome after carotid intervention: a review. Cardiol Rev. 2012; 20:84–9.9. Lin YH, Liu HM. Update on cerebral hyperperfusion syndrome. J Neurointerv Surg. 2020; 12:788–93.10. Petersen NH, Silverman A, Strander SM, Kodali S, Wang A, Sansing LH, et al. Fixed compared with autoregulation-oriented blood pressure thresholds after mechanical thrombectomy for ischemic stroke. Stroke. 2020; 51:914–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
- Mechanical Thrombectomy for Large Vessel Occlusion via the Transbrachial Approach: Case Series
- Differences in mechanical thrombectomy for acute ischemic stroke on weekdays versus nights/ weekends in a Japanese primary stroke core center
- Delayed Development of Symptomatic Arterial Stenosis after a Mechanical Thrombectomy for an Acute Embolic Occlusion of the Middle Cerebral Artery
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series