J Neurocrit Care.
2023 Jun;16(1):10-17. 10.18700/jnc.230008.
The etiology and mortality of altered level of consciousness in the emergency room: before and after coronavirus disease
- Affiliations
-
- 1Department of Emergency Medicine, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Neurology, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2543387
- DOI: http://doi.org/10.18700/jnc.230008
Abstract
- Background
Coronavirus disease 2019 (COVID-19) has resulted in social, economic, medical, and psychological changes. New-onset altered level of consciousness (ALC) is a classical presentation in real-world medicine. This study investigated changes in ALC in the emergency room (ER) in the periods before (BC) and after (AC) COVID-19.
Methods
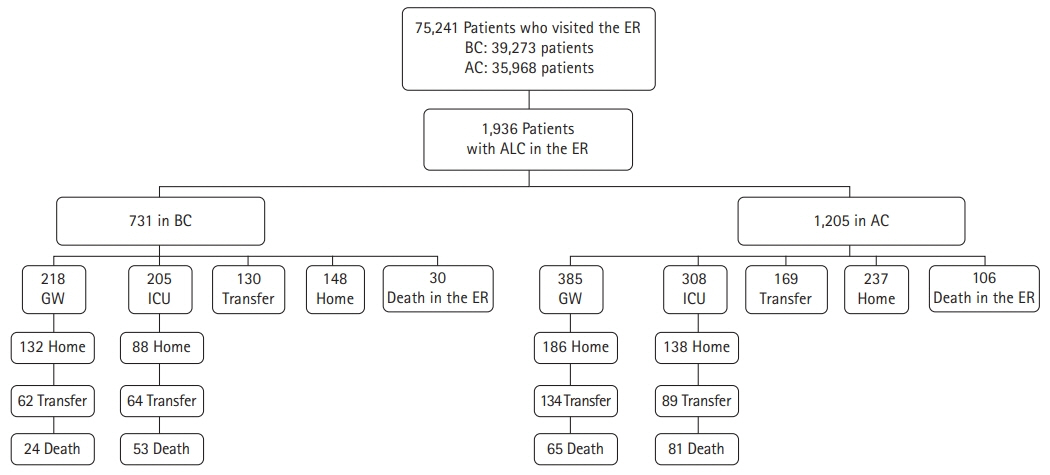
This was a retrospective study of patients with ALCs who visited the ER of a tertiary referral center, and their medical records BC and AC were compared. A consortium allocated and analyzed the etiologies of ALC in a case-by-case discussion. The time point for etiological assessment was the time of discharge from the ER.
Results
In total, 1,936 patients with ALCs (731 and 1,205 in BC and AC, respectively) were investigated. The most common etiology was systemic infection (25.9%), followed by metabolic causes (20.8%). Systemic infections (22.9% vs. 30.8%, P<0.001) and stroke (14.6% vs. 18.2%, P=0.037) were lower in AC than in BC, respectively, whereas rates of toxicity (15.4% vs. 6.0%, P<0.001) and traumatic brain injury (TBI; 5.9% vs. 0.8%, P<0.001) were higher in AC than in BC. The overall mortality rate of ALC in the ER was 18.5%.
Conclusion
This study demonstrated that the major etiologies of ALC in the ER were extra-cranial (58.5%). The mortality of ALC in the ER and the incidence of toxic cause and TBI increased in AC, suggesting a change in medical circumstances after the Pandemic.
Keyword
Figure
Reference
-
1. Kanich W, Brady WJ, Huff JS, Perron AD, Holstege C, Lindbeck G, et al. Altered mental status: evaluation and etiology in the ED. Am J Emerg Med. 2002; 20:613–7.2. Kim KT, Jeon JC, Jung CG, Park JA, Seo JG, Kwon DH. Etiologies of altered level of consciousness in the emergency room. Sci Rep. 2022; 12:4972.3. Kekec Z, Senol V, Koc F, Seydaoglu G. Analysis of altered mental status in Turkey. Int J Neurosci. 2008; 118:609–17.4. Xiao HY, Wang YX, Xu TD, Zhu HD, Guo SB, Wang Z, et al. Evaluation and treatment of altered mental status patients in the emergency department: life in the fast lane. World J Emerg Med. 2012; 3:270–7.5. Völk S, Koedel U, Pfister HW, Schwankhart R, Op den Winkel M, Mühlbauer K, et al. Impaired consciousness in the emergency department. Eur Neurol. 2018; 80:179–86.6. Forsberg S, Höjer J, Enander C, Ludwigs U. Coma and impaired consciousness in the emergency room: characteristics of poisoning versus other causes. Emerg Med J. 2009; 26:100–2.7. Jung S, Jeon JC, Jung CG, Cho YW, Kim KT. The etiologies of altered level of consciousness in the emergency department. J Neurocrit Care. 2020; 13:86–92.8. Kim KT, Kwon DH, Jeon JC, Kim IC, Park JA, Seo JG. A multicenter study of altered level of consciousness in the emergency room. Intern Emerg Med. 2022; 17:2329–37.9. Ristau P, Wnent J, Gräsner JT, Fischer M, Bohn A, Bein B, et al. Impact of COVID-19 on out-of-hospital cardiac arrest: a registry-based cohort-study from the German Resuscitation Registry. PLoS One. 2022; 17:e0274314.10. Lu M, Liao X. Access to care through telehealth among U.S. Medicare beneficiaries in the wake of the COVID-19 pandemic. Front Public Health. 2022; 10:946944.11. Richards JR, Derlet RW. Emergency department hallway care from the millennium to the pandemic: a clear and present danger. J Emerg Med. 2022; 63:565–8.12. Adjemian J, Hartnett KP, Kite-Powell A, DeVies J, Azondekon R, Radhakrishnan L, et al. Update: COVID-19 pandemic-associated changes in emergency department visits: United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021; 70:552–6.13. Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020; 76:595–601.14. Reschen ME, Bowen J, Novak A, Giles M, Singh S, Lasserson D, et al. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg Med. 2021; 21:143.15. Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE 3rd, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020; 180:1328–33.16. Laukkanen L, Lahtinen S, Liisanantti J, Kaakinen T, Ehrola A, Raatiniemi L. Early impact of the COVID-19 pandemic and social restrictions on ambulance missions. Eur J Public Health. 2021; 31:1090–5.17. Kim YS, Kim IB, Kim SR, Cho BJ. Changes in emergency department case severity and length of stay before and after COVID-19 outbreak in Korea. Healthcare (Basel). 2022; 10:1540.18. Chang H, Kang MW, Paek SH. Impact of the COVID-19 pandemic on emergency department utilization patterns in South Korea: a retrospective observational study. Medicine (Baltimore). 2022; 101:e29009.19. Melnick G, O’Leary JF, Zaniello BA, Abrishamian L. COVID-19 driven decline in emergency visits: has it continued, is it permanent, and what does it mean for emergency physicians? Am J Emerg Med. 2022; 61:64–7.20. Ghaderi H, Stowell JR, Akhter M, Norquist C, Pugsley P, Subbian V. Impact of COVID-19 pandemic on emergency department visits: a regional case study of informatics challenges and opportunities. AMIA Annu Symp Proc. 2022; 2021:496–505.21. Antoniello D, Milstein MJ, Dardick J, Fernandez-Torres J, Lu J, Patel N, et al. Altered mental status in COVID-19. J Neurol. 2022; 269:12–8.22. Ha JY, Sung WY. Impact of COVID-19 pandemic on emergency department length of stay and clinical outcomes of patients with severe pneumonia: a single-center observational study. Medicine (Baltimore). 2022; 101:e30633.23. Tani T, Imai S, Fushimi K. Impact of the COVID-19 pandemic on emergency admission for patients with stroke: a time series study in Japan. Neurol Res Pract. 2021; 3:64.24. Park B, Bae W, Kim HJ, Lim JY, Oh SH, Youn CS, et al. Impact of COVID-19 pandemic on patients with cardio/cerebrovascular disease who visit the emergency department. Am J Emerg Med. 2022; 58:100–5.25. Kang JH, Lee SW, Ji JG, Yu JK, Jang YD, Kim SJ, et al. Changes in the pattern of suicide attempters visiting the emergency room after COVID-19 pandemic: an observational cross sectional study. BMC Psychiatry. 2021; 21:571.26. Holland KM, Jones C, Vivolo-Kantor AM, Idaikkadar N, Zwald M, Hoots B, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021; 78:372–9.27. Farooq S, Tunmore J, Wajid Ali M, Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. 2021; 306:114228.28. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021; 398:1700–12.29. Kim J, Kim C, Park SY. Impact of COVID-19 on emergency medical services for patients with acute stroke presentation in Busan, South Korea. J Clin Med. 2021; 11:94.30. Sedova P, Kent JA, Bryndziar T, Jarkovsky J, Tomek A, Sramek M, et al. The decline in stroke hospitalization due to COVID-19 is unrelated to COVID-19 intensity. Eur J Neurol. 2023; 30:943–50.31. Damara FA, Muchamad GR, Anton A, Ramdhani AN, Channel IC, Faried A. Epidemiological pattern of traumatic brain injury in the COVID-19 pandemic: a systematic review and meta-analysis. World Neurosurg. 2022; 161:e698–709.32. Prawiroharjo P, Pangeran D, Supriawan H, Lastri D, Mayza A, Zairinal RA, et al. Increasing traumatic brain injury incidence during COVID-19 pandemic in the emergency department of Cipto Mangunkusumo National General Hospital: a national referral hospital in Indonesia. Neurology. 2020; 95(12 Suppl 2):S11.33. Thai PQ, Toan DT, Son DT, Van HT, Minh LN, Hung LX, et al. Factors associated with the duration of hospitalisation among COVID-19 patients in Vietnam: a survival analysis. Epidemiol Infect. 2020; 148:e114.34. Martí-Fàbregas J, Guisado-Alonso D, Delgado-Mederos R, Martínez-Domeño A, Prats-Sánchez L, Guasch-Jiménez M, et al. Impact of COVID-19 infection on the outcome of patients with ischemic stroke. Stroke. 2021; 52:3908–17.35. Teixeira-Vaz A, Rocha JA, Costa A, Simões Moreira T, Almeida E Reis D, Oliveira M, et al. What is the impact of previous cerebrovascular disease on critical COVID-19 patients’ mortality?: a prospective cohort study. J Neurol Sci. 2022; 442:120382.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis on Patients Presenting with Altered Consciousness in the Emergency Room of S. N. U. H
- The etiologies of altered level of consciousness in the emergency department
- The Etiologies of Altered Level of Consciousness in the Emergency Department: Before versus after Coronavirus Disease-19
- Bedside Ultrasound for the Diagnosis of Bowel Necrosis in a Patient with an Altered Mental Status
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic