J Korean Med Sci.
2023 Jun;38(22):e169. 10.3346/jkms.2023.38.e169.
Moral Distress Regarding End-of-Life Care Among Healthcare Personnel in Korean University Hospitals: Features and Differences Between Physicians and Nurses
- Affiliations
-
- 1Department of Medical Humanities and Medical Education, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Anthropology, Seoul National University, Seoul, Korea
- 3Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 5Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 6Department of Pediatrics, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 8Department of Psychiatry, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2542801
- DOI: http://doi.org/10.3346/jkms.2023.38.e169
Abstract
- Background
Healthcare professionals often experience moral distress while providing endof-life care. This study explored how physicians and nurses experienced moral distress when they cared for critically and terminally ill patients in tertiary hospitals in South Korea.
Methods
This study used semi-structured in-depth interviews. A total of 22 people in two tertiary hospitals were interviewed, nine (40.9%) of which were physicians and 13 (59.1%) were nurses. The recorded interview files and memos were analyzed using grounded theory.
Results
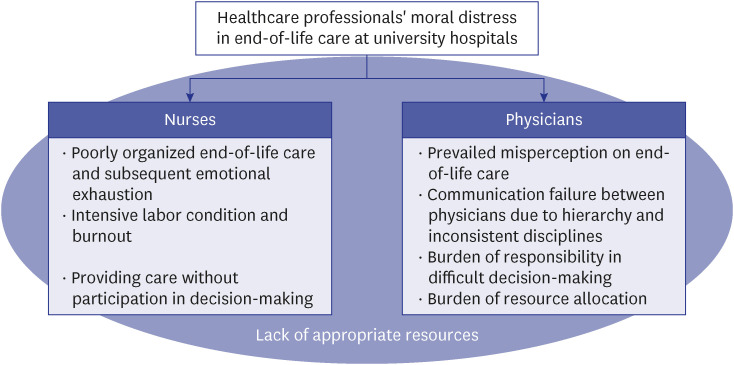
Most physicians and nurses encountered similar feelings of anger, helplessness, and burden owing to a lack of appropriate resources for end-of-life care. However, the factors and contexts of their moral distress differed. Nurses mainly addressed poorly organized end-of-life care, intensive labor conditions without support for nurses, and providing care without participation in decision-making. Meanwhile, physicians addressed the prevailing misperceptions on end-of-life care, communication failure between physicians owing to hierarchy and fragmented disciplines, the burden of responsibility in making difficult decisions, and the burden of resource allocation.
Conclusion
Differences in moral distress between physicians and nurses leave them isolated and can affect communication regarding healthcare. Mutual understanding between job disciplines will enhance their communication and help resolve conflicts in end-of-life care.
Keyword
Figure
Reference
-
1. Jameton A. Nursing Practice: The Ethical Issues. Englewood Cliffs, NJ, USA: Prentice-Hall;1984.2. Kälvemark S, Höglund AT, Hansson MG, Westerholm P, Arnetz B. Living with conflicts-ethical dilemmas and moral distress in the health care system. Soc Sci Med. 2004; 58(6):1075–1084. PMID: 14723903.
Article3. Wilkinson JM. Moral distress in nursing practice: experience and effect. Nurs Forum. 1987; 23(1):16–29. PMID: 3454003.
Article4. Oh Y, Gastmans C. Moral distress experienced by nurses: a quantitative literature review. Nurs Ethics. 2015; 22(1):15–31. PMID: 24091351.5. Bloomer MJ, Moss C, Cross WM. End-of-life care in acute hospitals: an integrative literature review. J Nurs Healthc Chronic Illn. 2011; 3(3):165–173.
Article6. Woo JA, Maytal G, Stern TA. Clinical challenges to the delivery of end-of-life care. Prim Care Companion J Clin Psychiatry. 2006; 8(6):367–372. PMID: 17245459.
Article7. Pauly BM, Varcoe C, Storch J. Framing the issues: moral distress in health care. HEC Forum. 2012; 24(1):1–11. PMID: 22446885.
Article8. Perni S. Moral distress: a call to action. AMA J Ethics. 2017; 19(6):533–536.
Article9. Moon JY, Lee HY, Lim CM, Koh Y. Medical residents’ perception and emotional stress on withdrawing life-sustaining therapy. Korean J Crit Care Med. 2012; 27(1):16–23.
Article10. Kang J, Choi EK, Seo M, Ahn GS, Park HY, Hong J, et al. Care for critically and terminally ill patients and moral distress of physicians and nurses in tertiary hospitals in South Korea: a qualitative study. PLoS One. 2021; 16(12):e0260343. PMID: 34914723.
Article11. Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Approaches. Lanham, MD, USA: Altamira Press;2006.12. Patton MQ. Qualitative Research and Evaluation Methods: Integrating Theory and Practice. Thousand Oaks, CA, USA: Sage Publications;2014.13. Strauss A, Corbin JM. Grounded Theory in Practice. Thousand Oaks, CA, USA: Sage;1997.14. Hamric AB, Davis WS, Childress MD. Moral distress in health care professionals. Pharos Alpha Omega Alpha Honor Med Soc. 2006; 69(1):16–23.15. Ulrich CM, Hamric AB, Grady C. Moral distress: a growing problem in the health professions? Hastings Cent Rep. 2010; 40(1):20–22.
Article16. Kim HR, Ahn SH. Moral sensitivity and moral distress among Korean hospital nurses. Korean J Med Ethics. 2010; 13(4):321–336.
Article17. Yoo MS. A study on the degree of moral distress of nurses in a city. J Korean Acad Nurs Adm. 2006; 12(1):131–139.18. Han SJ. Relationship between moral distress and turnover intention among hospital nurses. J Korea Cont Assoc. 2012; 12(3):276–284.
Article19. Balaban RB. A physician’s guide to talking about end-of-life care. J Gen Intern Med. 2000; 15(3):195–200. PMID: 10718901.
Article20. Institute of Medicine. Approaching Death. Washington, D.C., USA: National Academies Press;1997.21. Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003; 18(9):685–695. PMID: 12950476.22. Kang SY, Lee BS. The lived experience of nursing care for the dying patients in clinical nurses. J Korean Acad Nurs Adm. 2001; 7(2):237–251.23. Huffman DM, Rittenmeyer L. How professional nurses working in hospital environments experience moral distress: a systematic review. Crit Care Nurs Clin North Am. 2012; 24(1):91–100. PMID: 22405714.
Article24. Choe K, Kang Y, Park Y. Moral distress in critical care nurses: a phenomenological study. J Adv Nurs. 2015; 71(7):1684–1693. PMID: 25688835.
Article25. Walker RM, Miles SH, Stocking CB, Siegler M. Physicians’ and nurses’ perceptions of ethics problems on general medical services. J Gen Intern Med. 1991; 6(5):424–429. PMID: 1744757.
Article26. Angell M. The doctor as double agent. Kennedy Inst Ethics J. 1993; 3(3):279–286. PMID: 10127995.
Article28. Scheunemann LP, White DB. The ethics and reality of rationing in medicine. Chest. 2011; 140(6):1625–1632. PMID: 22147821.
Article29. Oberle K, Hughes D. Doctors’ and nurses’ perceptions of ethical problems in end-of-life decisions. J Adv Nurs. 2001; 33(6):707–715. PMID: 11298208.
Article30. Goethals S, Gastmans C, de Casterlé BD. Nurses’ ethical reasoning and behaviour: a literature review. Int J Nurs Stud. 2010; 47(5):635–650. PMID: 20096413.
Article31. Carse A, Rushton CH. Harnessing the promise of moral distress: a call for re-orientation. J Clin Ethics. 2017; 28(1):15–29. PMID: 28436924.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of ICU Nurses' Difficulties in End-of-Life Care to Moral Distress, Burnout and Job Satisfaction
- Lived experiences toward moral distress among long-term care hospital nurses: A phenomenological approach
- The Impact of Nurses' Attitude toward Dignified Death and Moral Sensitivity on Their End-of-Life Care Performance
- The relationships between moral distress and quality of nursing care in oncology nurses
- Pediatric Nurses' Perceptions related to End-of-Life Care and Turnover Intention