Ann Surg Treat Res.
2023 Jun;104(6):348-357. 10.4174/astr.2023.104.6.348.
Hepatic venous territory mapping in living donor liver transplantation using right liver graft: an objective parameter for venous reconstruction
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- KMID: 2542799
- DOI: http://doi.org/10.4174/astr.2023.104.6.348
Abstract
- Purpose
This study evaluated the clinical implication of hepatic venous territory mapping in living donor liver transplantation.
Methods
Living donor liver transplantations performed using right graft since 2017 were included. Hepatic venous volume mapping was started in 2019. Risk factors for graft failure and overall survival were analyzed. Analysis for factors related to occlusion of reconstructed vein was performed.
Results
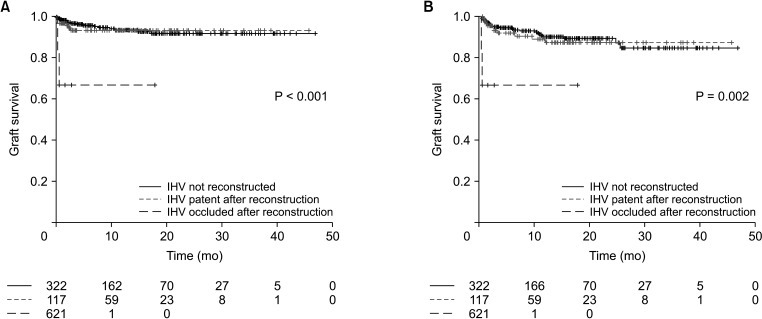
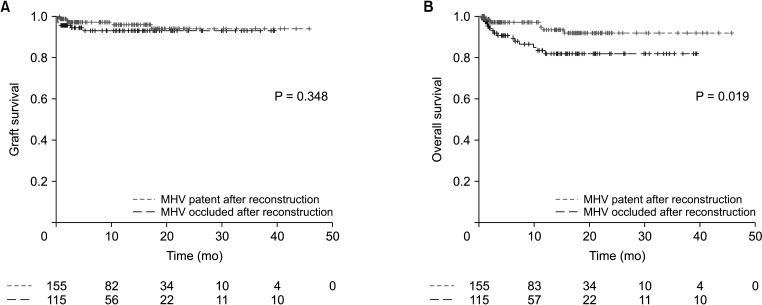
Among 445 patients included, 213 underwent hepatic venous mapping. Hepatic venous mapping itself was not a significant factor for graft (hazard ratio [HR], 0.958; 95% confidence interval [CI], 0.441–2.082; P = 0.913) and overall survival (HR, 0.627; 95% CI, 0.315–1.247; P = 0.183). Inferior hepatic vein occlusion was a significant risk factor for both graft survival (HR, 8.795; 95% CI, 1.628–47.523; P = 0.012) and overall survival (HR, 11.13; 95% CI, 2.460–50.300; P = 0.002). In a subgroup with middle hepatic vein reconstruction, occlusion was a significant risk factor for overall survival (HR, 3.289; 95% CI, 1.304–8.296; P = 0.012). In patients with middle hepatic vein reconstruction whose venous territory volumes were measured, right anterior volume of ≥300 cm 3 was protective for vein occlusion (OR, 0.317; 95% CI, 0.152–0.662; P = 0.002). In patients with V5 reconstruction, V5 volume of ≥150 cm 3 was protective for vein occlusion (OR, 0.253; 95% CI, 0.087–0.734; P = 0.011).
Conclusion
Inferior and middle hepatic vein reconstruction has significant impact on clinical outcome. Hepatic venous territory mapping can provide an objective measure for successful reconstruction of venous branches.
Figure
Reference
-
1. Gang S, Choi Y, Lee B, Yoon KC, Hong SY, Suh S, et al. Long-term outcomes of liver transplantation using grafts from donors with active hepatitis B virus replication: a multicenter cohort study. Ann Surg Treat Res. 2023; 104:183–194. PMID: 37051154.2. Lee SG. Techniques of reconstruction of hepatic veins in living-donor liver transplantation, especially for right hepatic vein and major short hepatic veins of right-lobe graft. J Hepatobiliary Pancreat Surg. 2006; 13:131–138. PMID: 16547674.3. Hwang S, Ha TY, Ahn CS, Moon DB, Kim KH, Song GW, et al. Reconstruction of inferior right hepatic veins in living donor liver transplantation using right liver grafts. Liver Transpl. 2012; 18:238–247. PMID: 22140053.4. Rhu J, Kim JM, Jeong WK, Choi GS, Joh JW. Venous outflow congestion is related to poor recurrence-free survival of living donor liver transplantation recipients with hepatocellular carcinoma: a retrospective study. Transpl Int. 2021; 34:272–280. PMID: 33253442.5. Kim SJ, Kim JM, Yi NJ, Choi GS, Lee KW, Suh KS, et al. Validation for models for tumor recurrence after liver transplantation in hepatectomy patients. Ann Surg Treat Res. 2022; 102:131–138. PMID: 35317356.6. Kim M, Rhu J, Choi GS, Kim JM, Joh JW. Risk factors for poor survival after recurrence of hepatocellular carcinoma after liver transplantation. Ann Surg Treat Res. 2021; 101:28–36. PMID: 34235114.7. Ito K, Akamatsu N, Tani K, Ito D, Kaneko J, Arita J, et al. Reconstruction of hepatic venous tributary in right liver living donor liver transplantation: the importance of the inferior right hepatic vein. Liver Transpl. 2016; 22:410–419. PMID: 26684079.8. Suh SW, Lee JM, You T, Choi YR, Yi NJ, Lee KW, et al. Hepatic venous congestion in living donor grafts in liver transplantation: is there an effect on hepatocellular carcinoma recurrence? Liver Transpl. 2014; 20:784–790. PMID: 24668935.9. Grąt M, Krawczyk M, Wronka KM, Stypułkowski J, Lewandowski Z, Wasilewicz M, et al. Ischemia-reperfusion injury and the risk of hepatocellular carcinoma recurrence after deceased donor liver transplantation. Sci Rep. 2018; 8:8935. PMID: 29895820.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The clinical implication of hepatic venous territory mapping in living donor liver transplantation using right liver graft
- Hepatic Artery Reconstruction Using the Right Gastroepiploic Artery for Hepatic Artery Inflow in a Living Donor Liver Transplantation
- Revolution and Refinement of Surgical Techniques for Living Donor Partial Liver Transplantation
- Salvage aorto-hepatic jump graft for hepatic artery thrombosis following living donor liver transplantation: a case report with 10-year follow-up
- Hepatic Vein Reconstruction for Living Donor Liver Transplantation using a Modified Right lobe Graft: Experience at Asan Medical Center and focused on Middle Hepatic Vein Reconstruction