Ann Surg Treat Res.
2023 Jun;104(6):325-331. 10.4174/astr.2023.104.6.325.
Trends and outcomes of emergency general surgery in elderly and highly elderly population in a single regional emergency center
- Affiliations
-
- 1Department of Surgery, Myongji Hospital, Hanyang University Medical Center, Goyang, Korea
- 2Department of Surgery, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- KMID: 2542796
- DOI: http://doi.org/10.4174/astr.2023.104.6.325
Abstract
- Purpose
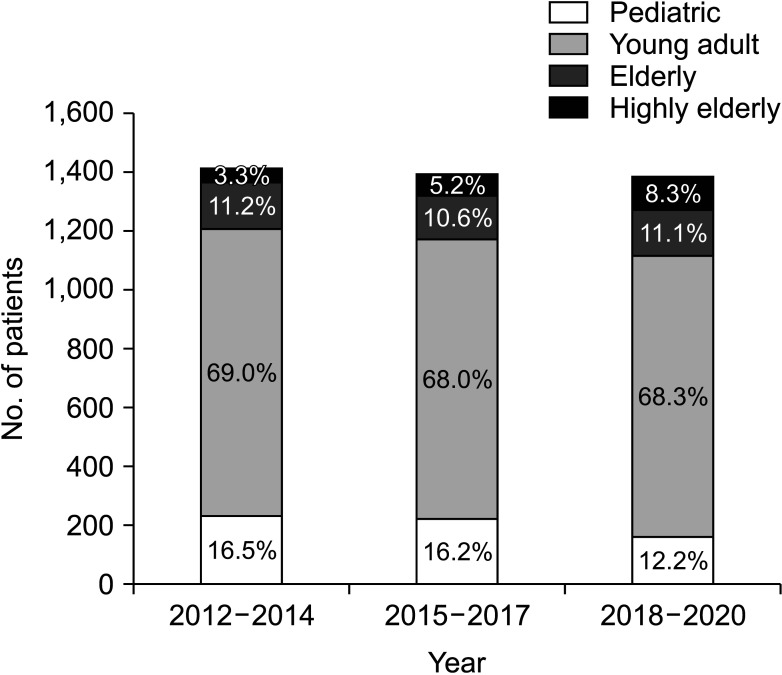
The number of elderly patients, especially aged ≥80 years, undergoing emergency surgery is gradually increasing. The aim of this study was to find out the trends and results of emergency general surgery for elderly patients over 9 years in an emergency medical center in South Korea, where the population is aging most rapidly.
Methods
The clinical characteristics, outcomes, and medical expenses of emergency general surgery for the elderly (aged 65–79 years) and highly elderly (aged ≥80 years) patients who visited to a regional emergency medical center from 2012 to 2020 were analyzed.
Results
The number of highly elderly patients increased with each 3-year interval, whereas the proportion of patients aged 19–79 years was similar, and that of pediatric patients was decreasing. The higher the age group, the higher the mortality (young adult vs. elderly vs. highly elderly: odds ratio [OR], 1 vs. 3.689 vs. 11.293; P < 0.001) and complication rates (OR, 1 vs. 2.840 vs. 4.633; P < 0.001), and longer length of hospital stay (β = 0.949, P = 0.001) even after adjusting for the type of surgery and the American Society of Anesthesiologists physical status classification. Non-covered medical expenses were significantly related to the age groups (β = 151,608.802, P < 0.001).
Conclusion
The higher age group was associated with increased number of unfavorable outcomes after emergency general surgery, along with increased medical cost. Efforts to prevent emergency surgery for elderly patients and a specialized treatment system are needed.
Keyword
Figure
Cited by 1 articles
-
National cancer screening program for colorectal cancer in Korea
Seung Min Baik, Ryung-Ah Lee
Ann Surg Treat Res. 2023;105(6):333-340. doi: 10.4174/astr.2023.105.6.333.
Reference
-
1. Baek JY, Lee E, Jung HW, Jang IY. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res. 2021; 25:65–71. PMID: 34187140.2. Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003; 238:170–177. PMID: 12894008.3. Ukkonen M, Jämsen E, Zeitlin R, Pauniaho SL. Emergency department visits in older patients: a population-based survey. BMC Emerg Med. 2019; 19:20. PMID: 30813898.4. Kuy S, Sosa JA, Roman SA, Desai R, Rosenthal RA. Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg. 2011; 201:789–796. PMID: 21741511.5. Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, et al. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015; 78:306–311. PMID: 25757115.6. Hadaya J, Sanaiha Y, Juillard C, Benharash P. Impact of frailty on clinical outcomes and resource use following emergency general surgery in the United States. PLoS One. 2021; 16:e0255122. PMID: 34297772.7. Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, Haider AH, et al. Use of national burden to define operative emergency general surgery. JAMA Surg. 2016; 151:e160480. PMID: 27120712.8. Ministry of the Interior and Safety (MOIS), Republic of Korea. Population status by age [Internet]. MOIS;2022. cited 2022 Jun 10. Available from: https://jumin.mois.go.kr/ageStatMonth.do .9. Cooper Z, Scott JW, Rosenthal RA, Mitchell SL. Emergency major abdominal surgical procedures in older adults: a systematic review of mortality and functional outcomes. J Am Geriatr Soc. 2015; 63:2563–2571. PMID: 26592523.10. Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Variation in quality of care after emergency general surgery procedures in the elderly. J Am Coll Surg. 2011; 212:1039–1048. PMID: 21620289.11. Lee SI, Na BG, Yoo YS, Mun SP, Choi NK. Clinical outcome for laparoscopic cholecystectomy in extremely elderly patients. Ann Surg Treat Res. 2015; 88:145–151. PMID: 25741494.12. Havens JM, Columbus AB, Seshadri AJ, Brown CV, Tominaga GT, Mowery NT, et al. Risk stratification tools in emergency general surgery. Trauma Surg Acute Care Open. 2018; 3:e000160. PMID: 29766138.13. Chua MS, Chan DK. Increased morbidity and mortality of emergency laparotomy in elderly patients. World J Surg. 2020; 44:711–720. PMID: 31646368.14. Joseph B, Zangbar B, Pandit V, Fain M, Mohler MJ, Kulvatunyou N, et al. Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg. 2016; 222:805–813. PMID: 27113515.15. Eamer GJ, Clement F, Pederson JL, Churchill TA, Khadaroo RG. Analysis of postdischarge costs following emergent general surgery in elderly patients. Can J Surg. 2018; 61:19–27. PMID: 29368673.16. McIsaac DI, Taljaard M, Bryson GL, Beaulé PE, Gagné S, Hamilton G, et al. Frailty as a predictor of death or new disability after surgery: a prospective cohort study. Ann Surg. 2020; 271:283–289. PMID: 30048320.17. Song YJ. The South Korean health care system. JMAJ. 2009; 52:206–209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the characteristics of elderly patients with respiratory symptoms who visited the emergency department
- The Clinical Characteristics of Elderly Suicide Attempters Visiting Emergency Room
- Is the bedside on-site ultrasonography for elderly patients with chest pain sufficiently performed?: focused on non-traumatic patients who visited EDs
- Regionalization of emergency medical system and re-establishment of regional emergency medical plan
- Comparison of Anatomical and Clinical Characteristics in Emergency Endotracheal Intubation Between Non-Elderly and Elderly Adults