Ann Hepatobiliary Pancreat Surg.
2023 May;27(2):195-200. 10.14701/ahbps.22-107.
IPMN-LEARN: A linear support vector machine learning model for predicting low-grade intraductal papillary mucinous neoplasms
- Affiliations
-
- 1Division of Gastroenterology, Massachusetts General Hospital, Boston, MA, United States
- 2Division of Radiology, Massachusetts General Hospital, Boston, MA, United States
- 3Department of Surgical Oncology, Massachusetts General Hospital, Boston, MA, United States
- 4Harvard Medical School, Boston, MA, United States
- KMID: 2542584
- DOI: http://doi.org/10.14701/ahbps.22-107
Abstract
- Backgrounds/Aims
We aimed to build a machine learning tool to help predict low-grade intraductal papillary mucinous neoplasms (IPMNs) in order to avoid unnecessary surgical resection. IPMNs are precursors to pancreatic cancer. Surgical resection remains the only recognized treatment for IPMNs yet carries some risks of morbidity and potential mortality. Existing clinical guidelines are imperfect in distinguishing low-risk cysts from high-risk cysts that warrant resection.
Methods
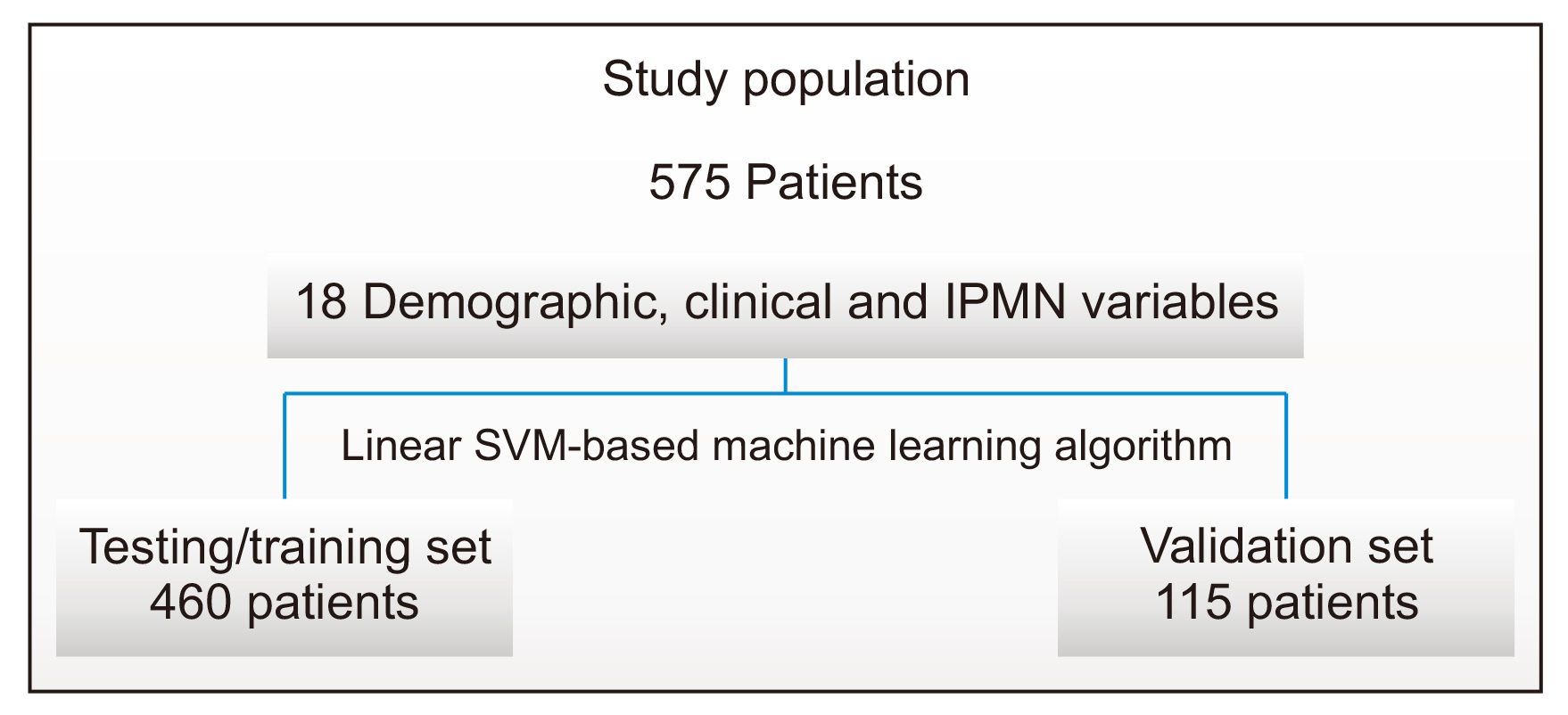
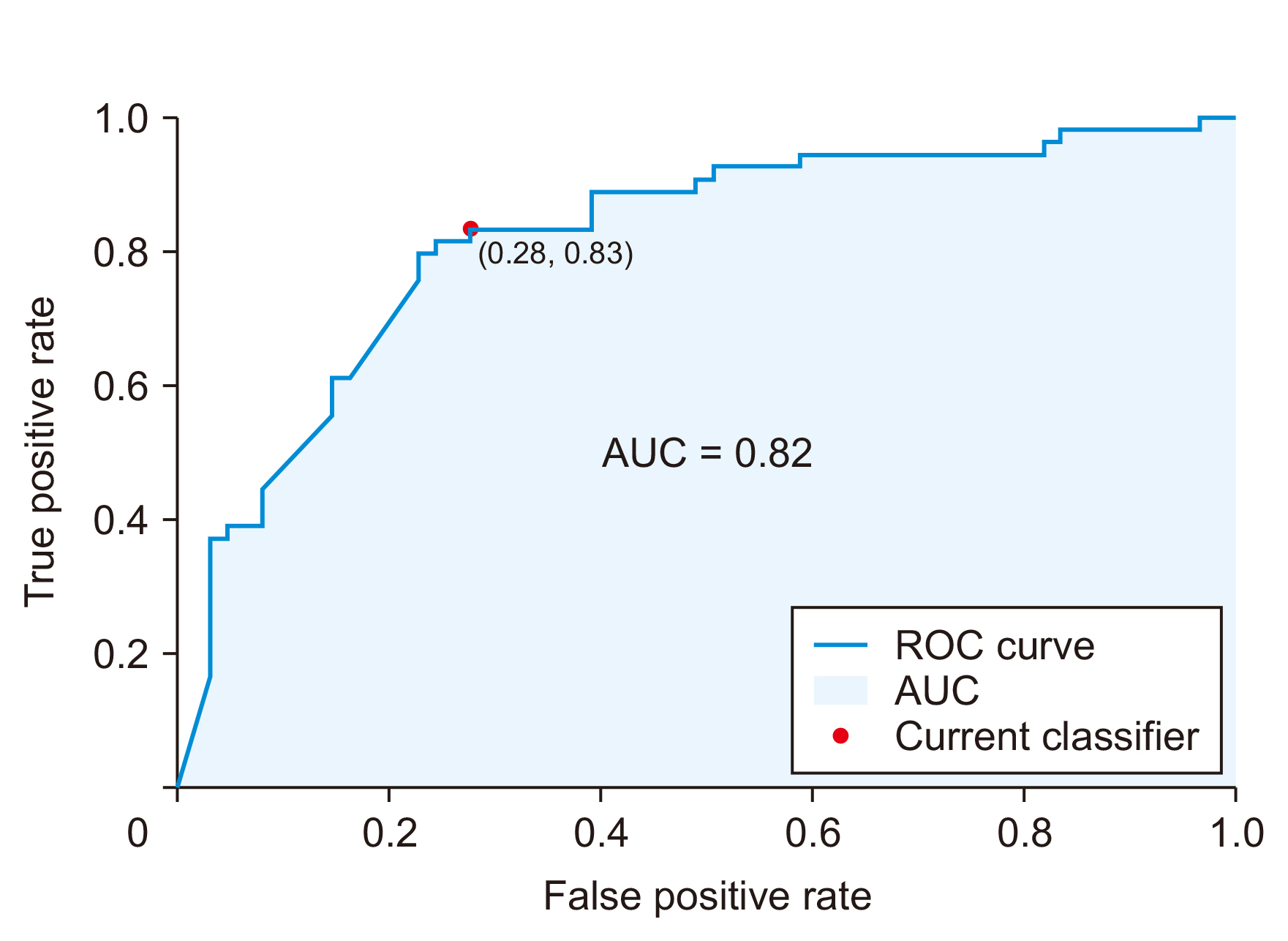
We built a linear support vector machine (SVM) learning model using a prospectively maintained surgical database of patients with resected IPMNs. Input variables included 18 demographic, clinical, and imaging characteristics. The outcome variable was the presence of low-grade or high-grade IPMN based on post-operative pathology results. Data were divided into a training/validation set and a testing set at a ratio of 4:1. Receiver operating characteristics analysis was used to assess classification performance.
Results
A total of 575 patients with resected IPMNs were identified. Of them, 53.4% had low-grade disease on final pathology. After classifier training and testing, a linear SVM-based model (IPMN-LEARN) was applied on the validation set. It achieved an accuracy of 77.4%, with a positive predictive value of 83%, a specificity of 72%, and a sensitivity of 83% in predicting low-grade disease in patients with IPMN. The model predicted low-grade lesions with an area under the curve of 0.82.
Conclusions
A linear SVM learning model can identify low-grade IPMNs with good sensitivity and specificity. It may be used as a complement to existing guidelines to identify patients who could avoid unnecessary surgical resection.
Keyword
Figure
Reference
-
1. American Cancer Society. 2021. Cancer Facts & Figures 2021. American Cancer Society.2. Kromrey ML, Bülow R, Hübner J, Paperlein C, Lerch MM, Ittermann T, et al. 2018; Prospective study on the incidence, prevalence and 5-year pancreatic-related mortality of pancreatic cysts in a population-based study. Gut. 67:138–145. DOI: 10.1136/gutjnl-2016-313127. PMID: 28877981.
Article3. Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, et al. 2008; Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 191:802–807. DOI: 10.2214/AJR.07.3340. PMID: 18716113. PMCID: PMC2692243.
Article4. Kleeff J, Michalski C, Kong B, Erkan M, Roth S, Siveke J, et al. 2015; Surgery for cystic pancreatic lesions in the post-sendai era: a single institution experience. HPB Surg. 2015:847837. DOI: 10.1155/2015/847837. PMID: 25873753. PMCID: PMC4383461.
Article5. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. 2017; Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 17:738–753. DOI: 10.1016/j.pan.2017.07.007. PMID: 28735806.
Article6. Vege SS, Ziring B, Jain R, Moayyedi P. 2015; American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 148:819–822. quize12–13. DOI: 10.1053/j.gastro.2015.01.015. PMID: 25805375.
Article7. Elta GH, Enestvedt BK, Sauer BG, Lennon AM. 2018; ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 113:464–479. DOI: 10.1038/ajg.2018.14. PMID: 29485131.8. European Study Group on Cystic Tumours of the Pancreas. 2018; European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 67:789–804. DOI: 10.1136/gutjnl-2018-316027. PMID: 29574408. PMCID: PMC5890653.9. Lekkerkerker SJ, Besselink MG, Busch OR, Verheij J, Engelbrecht MR, Rauws EA, et al. 2017; Comparing 3 guidelines on the management of surgically removed pancreatic cysts with regard to pathological outcome. Gastrointest Endosc. 85:1025–1031. DOI: 10.1016/j.gie.2016.09.027. PMID: 27693645.
Article10. DiMaio CJ. 2018; Current guideline controversies in the management of pancreatic cystic neoplasms. Gastrointest Endosc Clin N Am. 28:529–547. DOI: 10.1016/j.giec.2018.05.005. PMID: 30241642.
Article11. Singhi AD, Zeh HJ, Brand RE, Nikiforova MN, Chennat JS, Fasanella KE, et al. 2016; American Gastroenterological Association guidelines are inaccurate in detecting pancreatic cysts with advanced neoplasia: a clinicopathologic study of 225 patients with supporting molecular data. Gastrointest Endosc. 83:1107–1117.e2. DOI: 10.1016/j.gie.2015.12.009. PMID: 26709110.
Article12. Ruffle JK, Farmer AD, Aziz Q. 2019; Artificial intelligence-assisted gastroenterology- promises and pitfalls. Am J Gastroenterol. 114:422–428. DOI: 10.1038/s41395-018-0268-4. PMID: 30315284.
Article13. Jović S, Miljković M, Ivanović M, Šaranović M, Arsić M. 2017; Prostate cancer probability prediction by machine learning technique. Cancer Invest. 35:647–651. DOI: 10.1080/07357907.2017.1406496. PMID: 29243988.
Article14. Burki TK. 2016; Predicting lung cancer prognosis using machine learning. Lancet Oncol. 17:e421. DOI: 10.1016/S1470-2045(16)30436-3. PMID: 27569440.
Article15. Rodriguez-Ruiz A, Lång K, Gubern-Merida A, Broeders M, Gennaro G, Clauser P, et al. 2019; Stand-alone artificial intelligence for breast cancer detection in mammography: comparison with 101 radiologists. J Natl Cancer Inst. 111:916–922. DOI: 10.1093/jnci/djy222. PMID: 30834436. PMCID: PMC6748773.
Article16. Noble WS. 2006; What is a support vector machine? Nat Biotechnol. 24:1565–1567. DOI: 10.1038/nbt1206-1565. PMID: 17160063.
Article17. Basturk O, Hong SM, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AV, et al. 2015; A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 39:1730–1741. DOI: 10.1097/PAS.0000000000000533. PMID: 26559377. PMCID: PMC4646710.
Article18. Dalal V, Carmicheal J, Dhaliwal A, Jain M, Kaur S, Batra SK. 2020; Radiomics in stratification of pancreatic cystic lesions: machine learning in action. Cancer Lett. 469:228–237. DOI: 10.1016/j.canlet.2019.10.023. PMID: 31629933. PMCID: PMC6927395.
Article19. Barua S, Solis L, Parra ER, Uraoka N, Jiang M, Wang H, et al. 2018; A functional spatial analysis platform for discovery of immunological interactions predictive of low-grade to high-grade transition of pancreatic intraductal papillary mucinous neoplasms. Cancer Inform. 17:1176935118782880. DOI: 10.1177/1176935118782880. PMID: 30013304. PMCID: PMC6043922.
Article20. Springer S, Masica DL, Dal Molin M, Douville C, Thoburn CJ, Afsari B, et al. 2019; A multimodality test to guide the management of patients with a pancreatic cyst. Sci Transl Med. 11:eaav4772. DOI: 10.1126/scitranslmed.aav4772. PMID: 31316009. PMCID: PMC7859881.
Article21. Amato E, Molin MD, Mafficini A, Yu J, Malleo G, Rusev B, et al. 2014; Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J Pathol. 233:217–227. DOI: 10.1002/path.4344. PMID: 24604757. PMCID: PMC4057302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Pancreatic Intraductal Papillary Mucinous Neoplasm with Splenic Invasion: A Case Report
- Pathologic View of Intraductal Papillary Mucinous Neoplasm
- Squamous cell carcinoma of the pancreas with a pancreatic intraductal papillary mucinous neoplasm: a case report
- Surgical Management of Intraductal Papillary Mucinous Neoplasms
- Medical Management of Intraductal Papillary Mucinous Neoplasm