Ann Hepatobiliary Pancreat Surg.
2023 May;27(2):189-194. 10.14701/ahbps.22-083.
Potential clinical utility of intraoperative fluid amylase measurement during pancreaticoduodenectomy
- Affiliations
-
- 1Liver Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom
- KMID: 2542583
- DOI: http://doi.org/10.14701/ahbps.22-083
Abstract
- Backgrounds/Aims
Postoperative pancreatic fistula (POPF) after pancreaticoduodenectomy (PD) is a source of major morbidity and mortality. Early diagnosis and treatment of POPF is mandatory to improve patient outcomes and clinical risk scores may be ombined with postoperative drain fluid amylase (DFA) values to stratify patients. The aim of this pilot study was to etermine if intraoperative fluid amylase (IFA) values correlate with DFA1 and POPF.
Methods
In patients undergoing PD from February to November 2020, intraoperative samples of intra-abdominal fluid adjacent to the pancreatic anastomosis were taken and sent for fluid amylase measurement prior to abdominal closure. Data regarding patient demographics, postoperative DFA values, complications, and mortality were prospectively collected.
Results
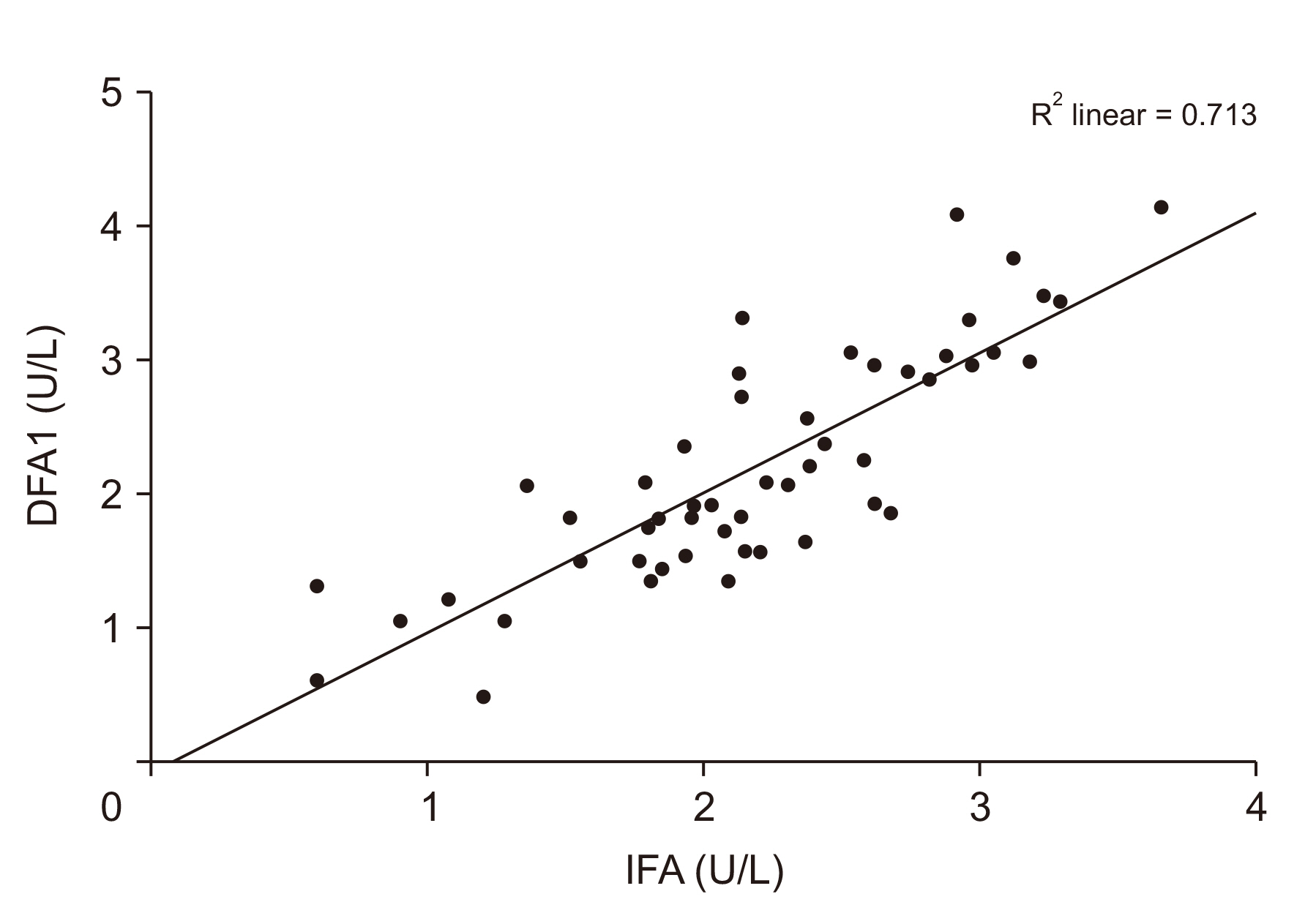
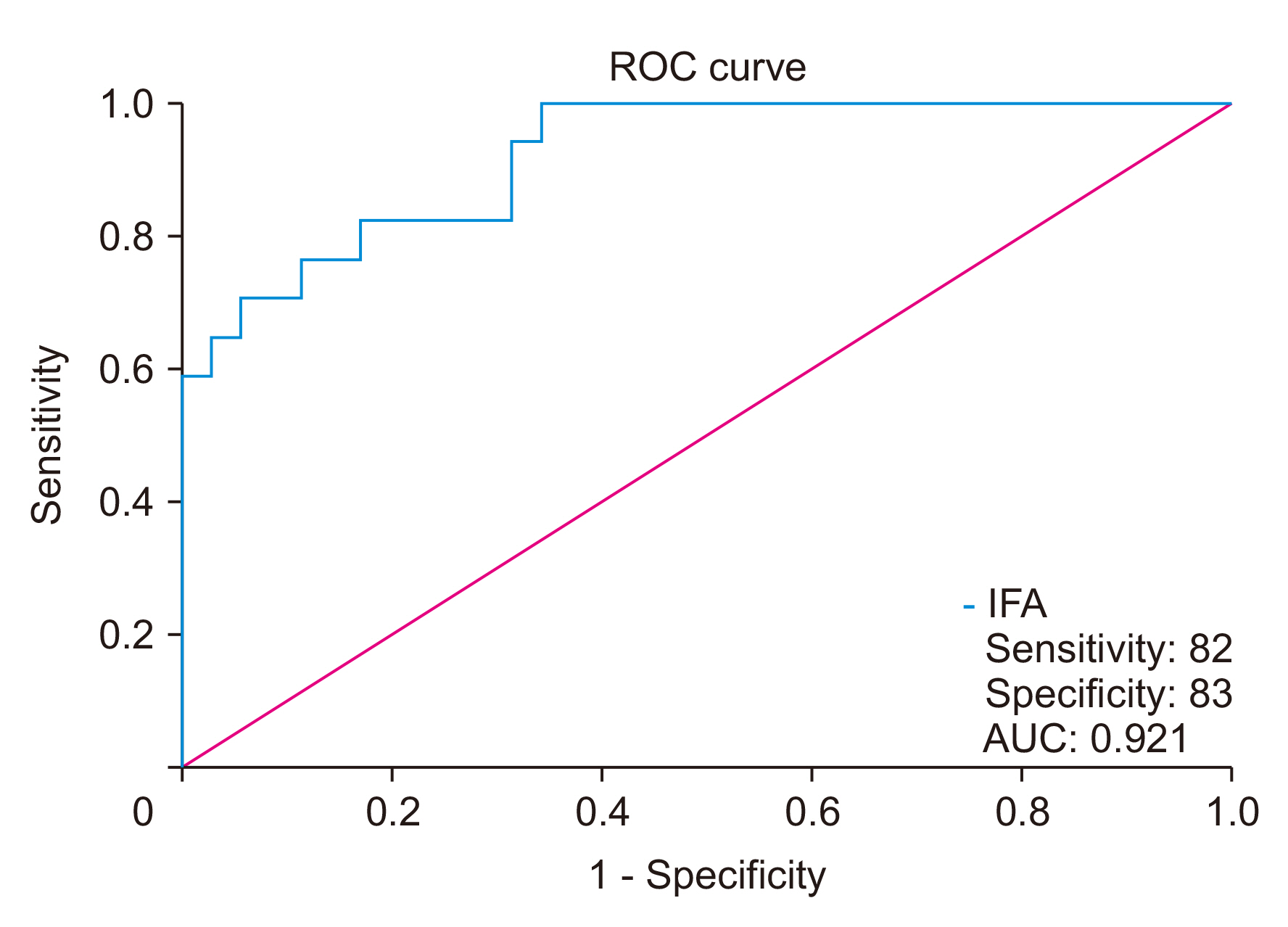
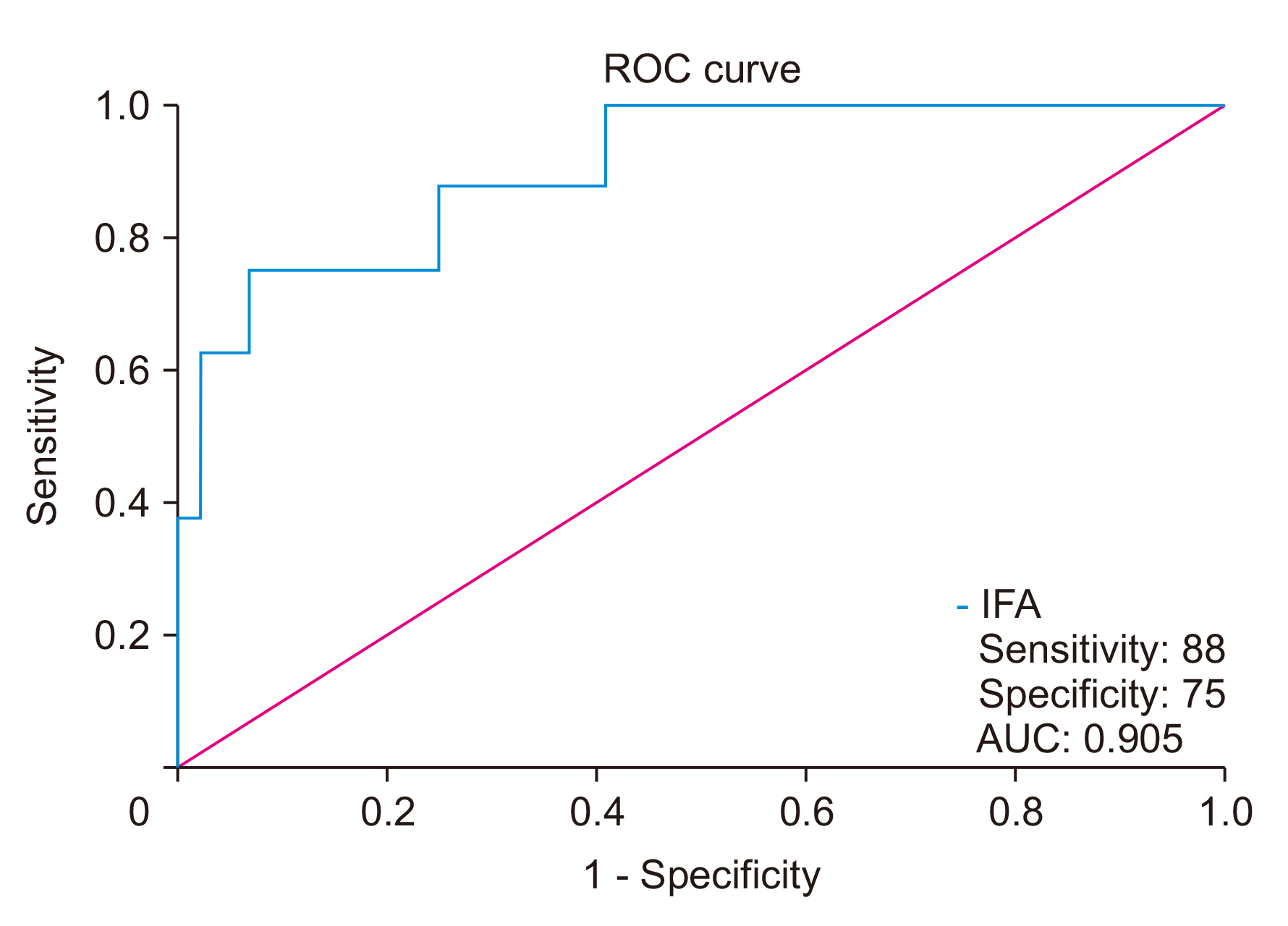
Data were obtained for 52 patients with a median alternative Fistula Risk Score (aFRS) of 9.9. Postoperative complications occurred in 20 (38.5%) patients (five Clavien grade ≥ 3). There were eight POPFs and two patients died (pneumonia/sepsis). There was a significant correlation between IFA and DFA1 (R2 = 0.713; p < 0.001) and DFA3 (p < 0.001), and the median IFA was higher in patients with POPF than patients without (1,232.5 vs. 122; p = 0.0003). IFA > 260 U/L predicted POPF with sensitivity, specificity, positive and negative predictive values of 88.0%, 75.0%, 39.0%, and 97.0%, respectively. The incidence of POPF was 43.0% in high-risk (high aFRS/ IFA) and 0% in lowrisk patients (low aFRS/IFA).
Conclusions
IFA correlated with POPF and may be a useful adjunct to clinical risk scores to stratify patients during PD. Larger, prospective studies are needed to determine whether IFA has clinical utility.
Keyword
Figure
Reference
-
1. Tsai CY, Lai BR, Wang SY, Liao CH, Liu YY, Kang SC, et al. 2017; The impact of preoperative etiology on emergent pancreaticoduodenectomy for non-traumatic patients. World J Emerg Surg. 12:21. DOI: 10.1186/s13017-017-0133-6. PMID: 28469698. PMCID: PMC5414322.
Article2. Whipple AO, Parsons WB, Mullins CR. 1935; Treatment of carcinoma of the ampulla of vater. Ann Surg. 102:763–779. DOI: 10.1097/00000658-193510000-00023. PMID: 17856666. PMCID: PMC1391173.3. Lubrano J, Bachelier P, Paye F, Le Treut YP, Chiche L, Sa-Cunha A, et al. 2018; Severe postoperative complications decrease overall and disease free survival in pancreatic ductal adenocarcinoma after pancreaticoduodenectomy. Eur J Surg Oncol. 44:1078–1082. DOI: 10.1016/j.ejso.2018.03.024. PMID: 29685757.
Article4. Khajanchee YS, Johnston WC, Cassera MA, Hansen PD, Hammill CW. 2017; Characterization of pancreaticojejunal anastomotic healing in a porcine survival model. Surg Innov. 24:15–22. DOI: 10.1177/1553350616674638. PMID: 27794116.
Article5. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. 2013; A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 216:1–14. DOI: 10.1016/j.jamcollsurg.2012.09.002. PMID: 23122535.
Article6. Ecker BL, McMillan MT, Asbun HJ, Ball CG, Bassi C, Beane JD, et al. 2018; Characterization and optimal management of high-risk pancreatic anastomoses during pancreatoduodenectomy. Ann Surg. 267:608–616. DOI: 10.1097/SLA.0000000000002327. PMID: 28594741.7. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. 2005; Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 138:8–13. DOI: 10.1016/j.surg.2005.05.001. PMID: 16003309.
Article8. Israel JS, Rettammel RJ, Leverson GE, Hanks LR, Cho CS, Winslow ER, et al. 2014; Does postoperative drain amylase predict pancreatic fistula after pancreatectomy? J Am Coll Surg. 218:978–987. DOI: 10.1016/j.jamcollsurg.2014.01.048. PMID: 24680573.
Article9. Bassi C, Molinari E, Malleo G, Crippa S, Butturini G, Salvia R, et al. 2010; Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg. 252:207–214. DOI: 10.1097/SLA.0b013e3181e61e88. PMID: 20622661.10. Petrowsky H, Demartines N, Rousson V, Clavien PA. 2004; Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg. 240:1074–1084. discussion 1084–1085. DOI: 10.1097/01.sla.0000146149.17411.c5. PMID: 15570212. PMCID: PMC1356522.11. Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, et al. 2014; A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 259:605–612. DOI: 10.1097/SLA.0000000000000460. PMID: 24374513.
Article12. Shukla PJ, Barreto SG, Fingerhut A, Bassi C, Büchler MW, Dervenis C, et al. 2010; Toward improving uniformity and standardization in the reporting of pancreatic anastomoses: a new classification system by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 147:144–153. DOI: 10.1016/j.surg.2009.09.003. PMID: 19879614.
Article13. Sutcliffe RP, Hamoui M, Isaac J, Marudanayagam R, Mirza DF, Muiesan P, et al. 2015; Implementation of an enhanced recovery pathway after pancreaticoduodenectomy in patients with low drain fluid amylase. World J Surg. 39:2023–2030. DOI: 10.1007/s00268-015-3051-3. PMID: 25809067.
Article14. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.15. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.
Article16. de Reuver PR, Gundara J, Hugh TJ, Samra JS, Mittal A. 2016; Intra-operative amylase in peri-pancreatic fluid independently predicts for pancreatic fistula post pancreaticoduodectomy. HPB (Oxford). 18:608–614. DOI: 10.1016/j.hpb.2016.05.007. PMID: 27346142. PMCID: PMC4925798.
Article17. Chen H, Wang W, Ying X, Deng X, Peng C, Cheng D, et al. 2020; Predictive factors for postoperative pancreatitis after pancreaticoduodenectomy: a single-center retrospective analysis of 1465 patients. Pancreatology. 20:211–216. DOI: 10.1016/j.pan.2019.11.014. PMID: 31831390.
Article18. Bannone E, Andrianello S, Marchegiani G, Masini G, Malleo G, Bassi C, et al. 2018; Postoperative acute pancreatitis following pancreaticoduodenectomy: a determinant of fistula potentially driven by the intraoperative fluid management. Ann Surg. 268:815–822. DOI: 10.1097/SLA.0000000000002900. PMID: 30004917.19. Yoo D, Park SY, Hwang DW, Lee JH, Song KB, Lee W, et al. 2021; Lack of association between postoperative pancreatitis and other postoperative complications following pancreaticoduodenectomy. J Clin Med. 10:1179. DOI: 10.3390/jcm10061179. PMID: 33799863. PMCID: PMC8001526.
Article20. Liu Y, Li Y, Wang L, Peng CJ. 2018; Predictive value of drain pancreatic amylase concentration for postoperative pancreatic fistula on postoperative day 1 after pancreatic resection: an updated meta-analysis. Medicine (Baltimore). 97:e12487. DOI: 10.1097/MD.0000000000012487. PMID: 30235751. PMCID: PMC6160246.21. Bertens KA, Crown A, Clanton J, Alemi F, Alseidi AA, Biehl T, et al. 2017; What is a better predictor of clinically relevant postoperative pancreatic fistula (CR-POPF) following pancreaticoduodenectomy (PD): postoperative day one drain amylase (POD1DA) or the fistula risk score (FRS)? HPB (Oxford). 19:75–81. DOI: 10.1016/j.hpb.2016.10.001. PMID: 27825541.
Article22. Sutcliffe RP, Battula N, Haque A, Ali A, inivasan P Sr, Atkinson SW, et al. 2012; Utility of drain fluid amylase measurement on the first postoperative day after pancreaticoduodenectomy. World J Surg. 36:879–883. DOI: 10.1007/s00268-012-1460-0. PMID: 22354484.
Article23. Conlon KC, Labow D, Leung D, Smith A, Jarnagin W, Coit DG, et al. 2001; Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg. 234:487–493. discussion 493–494. DOI: 10.1097/00000658-200110000-00008. PMID: 11573042. PMCID: PMC1422072.
Article24. Marchegiani G, Perri G, Burelli A, Zoccatelli F, Andrianello S, Luchini C, et al. 2022; High-risk pancreatic anastomosis versus total pancreatectomy after pancreatoduodenectomy: postoperative outcomes and quality of life analysis. Ann Surg. 276:e905–e913. DOI: 10.1097/SLA.0000000000004840. PMID: 33914471.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Result of Suction Pancreatic Stent in Pancreaticojejunostomy
- The Role of External Drainage and Octreotide in Preventing Complications after Pancreaticoduodenectomy
- Long Percutaneous Stent Insertion in Pancreatic Duct and Monitoring of Pancreaticojejunostomy Site Leakage in Periampullary Cancer Patients
- Changing patterns of Pancreatic enzyme after Distal Gastrectomy and the Effect of Protease Inhibitor Treatment
- Various retraction techniques for laparoscopic pancreaticoduodenectomy