Ann Hepatobiliary Pancreat Surg.
2023 May;27(2):172-179. 10.14701/ahbps.22-084.
Effects of cancer stigma on quality of life of patients with hepatobiliary and pancreatic cancer
- Affiliations
-
- 1Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Clinical Research Design and Evaluation, SAIHST, Sungkyunkwan University, Seoul, Korea
- 4Center for Clinical Epidemiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2542581
- DOI: http://doi.org/10.14701/ahbps.22-084
Abstract
- Backgrounds/Aims
Cancer stigma (CS), a self-inflicted sense of hopelessness, has been identified as a major factor affecting cancer patients’ outcomes. However, few studies have investigated the CS-related outcomes in hepatobiliary and pancreatic (HBP) cancer. Thus, the aim of this study was to investigate effects of CS on quality of life (QoL) of HBP cancer.
Methods
From 2017 to 2018, 73 patients who underwent curative surgery for HBP tumor at a single intuitive were enrolled prospectively. The QoL was measured using the European Organization for Research and Treatment of Cancer QoL score, and CS was evaluated in three categories, “impossibility of recovery,” “cancer stereotypes,” and “social discrimination.” the stigma was defined by higher scores of attitudes compared with the median value.
Results
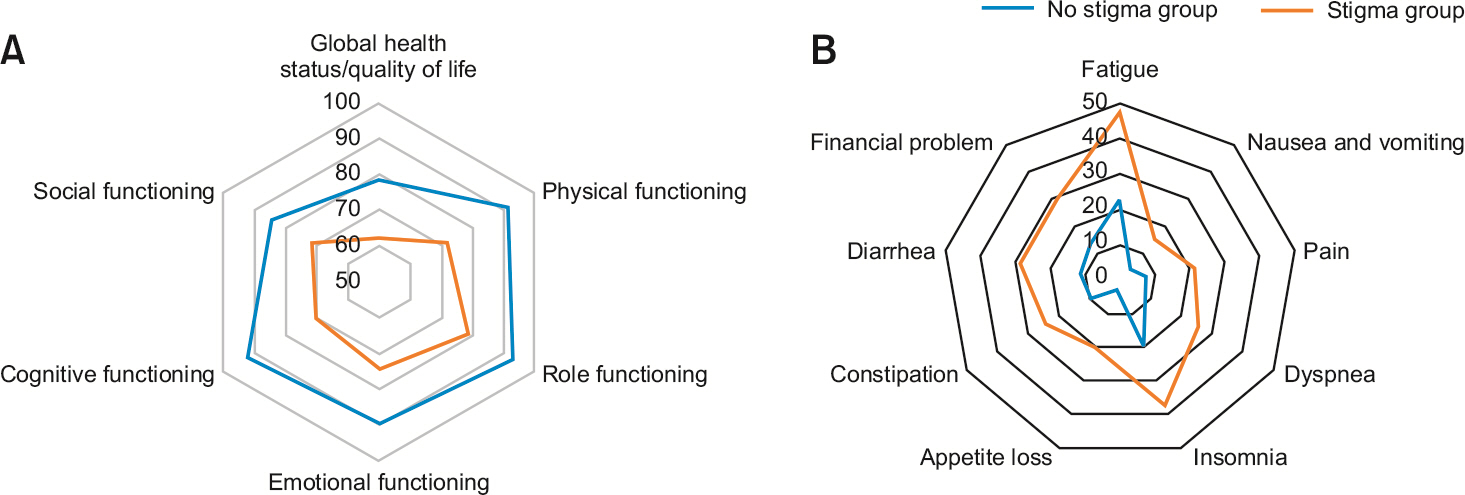
The stigma group showed a lower QoL (–17.67, 95% confidence interval [CI]: –26.75 to 8.60, p < 0.001) than the no stigma group. Similarly, most function and symptoms of the stigma group showed worse results than the no stigma group. The difference in function scores between the two groups according to CS was highest in cognitive function (–21.20, 95% CI: –30.36 to 12.04, p < 0.001). Fatigue showed the largest difference between the two groups at 22.84 (95% CI: 12.88–32.07, p < 0.001) and was the most severe symptom in stigma group.
Conclusions
CS was an important negative factor affecting the QoL, function, and symptoms of HBP cancer patients. Therefore, appropriate management of CS is crucial for improved postoperative QoL.
Keyword
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016; 66:7–30. DOI: 10.3322/caac.21332. PMID: 26742998.
Article2. Pulte D, Weberpals J, Schröder CC, Emrich K, Holleczek B, Katalinic A, et al. 2018; Survival of patients with hepatobiliary tract and duodenal cancer sites in Germany and the United States in the early 21st century. Int J Cancer. 143:324–332. DOI: 10.1002/ijc.31322. PMID: 29479701.
Article3. Carrato A, Falcone A, Ducreux M, Valle JW, Parnaby A, Djazouli K, et al. 2015; A systematic review of the burden of pancreatic cancer in Europe: real-world impact on survival, quality of life and costs. J Gastrointest Cancer. 46:201–211. DOI: 10.1007/s12029-015-9724-1. PMID: 25972062. PMCID: PMC4519613.
Article4. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH. Prediction of cancer incidence and mortality in Korea, 2017. Cancer Res Treat. 2017; 49:306–312. DOI: 10.4143/crt.2017.130. PMID: 28301926. PMCID: PMC5398390.
Article5. McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. 2018; Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 24:4846–4861. DOI: 10.3748/wjg.v24.i43.4846. PMID: 30487695. PMCID: PMC6250924.
Article6. Jia L, Jiang SM, Shang YY, Huang YX, Li YJ, Xie DR, et al. 2010; Investigation of the incidence of pancreatic cancer-related depression and its relationship with the quality of life of patients. Digestion. 82:4–9. DOI: 10.1159/000253864. PMID: 20145402.
Article7. Petzel MQ, Parker NH, Valentine AD, Simard S, Nogueras-Gonzalez GM, Lee JE, et al. 2012; Fear of cancer recurrence after curative pancreatectomy: a cross-sectional study in survivors of pancreatic and periampullary tumors. Ann Surg Oncol. 19:4078–4084. DOI: 10.1245/s10434-012-2566-1. PMID: 22875648.
Article8. Bauer MR, Bright EE, MacDonald JJ, Cleary EH, Hines OJ, Stanton AL. 2018; Quality of life in patients with pancreatic cancer and their caregivers: a systematic review. Pancreas. 47:368–375. DOI: 10.1097/MPA.0000000000001025. PMID: 29521939.
Article9. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009; 59:225–249. DOI: 10.3322/caac.20006. PMID: 19474385.
Article10. Cataldo JK, Jahan TM, Pongquan VL. 2012; Lung cancer stigma, depression, and quality of life among ever and never smokers. Eur J Oncol Nurs. 16:264–269. DOI: 10.1016/j.ejon.2011.06.008. PMID: 21803653. PMCID: PMC3360805.
Article11. Montazeri A, Milroy R, Hole D, McEwen J, Gillis CR. 2001; Quality of life in lung cancer patients: as an important prognostic factor. Lung Cancer. 31:233–240. DOI: 10.1016/S0169-5002(00)00179-3. PMID: 11165402.12. Montazeri A. 2009; Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008. Health Qual Life Outcomes. 7:102. DOI: 10.1186/1477-7525-7-102. PMID: 20030832. PMCID: PMC2805623.
Article13. Phelan SM, Griffin JM, Jackson GL, Zafar SY, Hellerstedt W, Stahre M, et al. 2013; Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psychooncology. 22:65–73. DOI: 10.1002/pon.2048. PMID: 21954081. PMCID: PMC6000725.
Article14. Stergiou-Kita M, Pritlove C, Kirsh B. 2016; The "Big C"-stigma, cancer, and workplace discrimination. J Cancer Surviv. 10:1035–1050. DOI: 10.1007/s11764-016-0547-2. PMID: 27170116.
Article15. Pinto AC, de Azambuja E. 2011; Improving quality of life after breast cancer: dealing with symptoms. Maturitas. 70:343–348. DOI: 10.1016/j.maturitas.2011.09.008. PMID: 22014722.
Article16. Chambers SK, Dunn J, Occhipinti S, Hughes S, Baade P, Sinclair S, et al. 2012; A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer. 12:184. DOI: 10.1186/1471-2407-12-184. PMID: 22607085. PMCID: PMC3517321.
Article17. Heijnders M, Van Der Meij S. 2006; The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 11:353–363. DOI: 10.1080/13548500600595327. PMID: 17130071.
Article18. Weiss MG, Ramakrishna J, Somma D. 2006; Health-related stigma: rethinking concepts and interventions. Psychol Health Med. 11:277–287. DOI: 10.1080/13548500600595053. PMID: 17130065.19. Ernst J, Mehnert A, Dietz A, Hornemann B, Esser P. 2017; Perceived stigmatization and its impact on quality of life - results from a large register-based study including breast, colon, prostate and lung cancer patients. BMC Cancer. 17:741. DOI: 10.1186/s12885-017-3742-2. PMID: 29121876. PMCID: PMC5680772.
Article20. Cho J, Smith K, Choi EK, Kim IR, Chang YJ, Park HY, et al. 2013; Public attitudes toward cancer and cancer patients: a national survey in Korea. Psychooncology. 22:605–613. DOI: 10.1002/pon.3041. PMID: 22344743.
Article21. Yun YH, Bae SH, Kang IO, Shin KH, Lee R, Kwon SI, et al. 2004; Cross-cultural application of the Korean version of the European Organization for Research and Treatment of Cancer (EORTC) Breast-Cancer-Specific Quality of Life Questionnaire (EORTC QLQ-BR23). Support Care Cancer. 12:441–445. DOI: 10.1007/s00520-004-0632-3. PMID: 15088137.
Article22. Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A. EORTC QLQ-C30 scoring manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer;2001.23. Ahles TA, Saykin AJ, McDonald BC, Li Y, Furstenberg CT, Hanscom BS, et al. 2010; Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol. 28:4434–4440. DOI: 10.1200/JCO.2009.27.0827. PMID: 20837957. PMCID: PMC2988635.
Article24. Jacobs W, Das E, Schagen SB. 2017; Increased cognitive problem reporting after information about chemotherapy-induced cognitive decline: the moderating role of stigma consciousness. Psychol Health. 32:78–93. DOI: 10.1080/08870446.2016.1244535. PMID: 27701901.
Article25. Burstein HJ. 2007; Cognitive side-effects of adjuvant treatments. Breast. 16 Suppl 2:S166–S168. DOI: 10.1016/j.breast.2007.07.027. PMID: 17719225.
Article26. Brown Johnson CG, Brodsky JL, Cataldo JK. 2014; Lung cancer stigma, anxiety, depression, and quality of life. J Psychosoc Oncol. 32:59–73. DOI: 10.1080/07347332.2013.855963. PMID: 24428251. PMCID: PMC4634635.
Article27. Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. 2000; Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 5:353–360. DOI: 10.1634/theoncologist.5-5-353. PMID: 11040270.
Article28. Daniell HW. 2004; Cancer-related fatigue: evolving concepts in evaluation and treatment. Cancer. 100:2484author reply 2484–2485. DOI: 10.1002/cncr.20246. PMID: 15160357.
Article29. Wang XS, Zhao F, Fisch MJ, O'Mara AM, Cella D, Mendoza TR, et al. 2014; Prevalence and characteristics of moderate to severe fatigue: a multicenter study in cancer patients and survivors. Cancer. 120:425–432. DOI: 10.1002/cncr.28434. PMID: 24436136. PMCID: PMC3949157.
Article30. Money S, Garber B. 2018; Management of cancer pain. Curr Emerg Hosp Med Rep. 6:141–146. DOI: 10.1007/s40138-018-0170-9.
Article31. Cataldo JK, Brodsky JL. 2013; Lung cancer stigma, anxiety, depression and symptom severity. Oncology. 85:33–40. DOI: 10.1159/000350834. PMID: 23816853.
Article32. Caffo O, Amichetti M, Ferro A, Lucenti A, Valduga F, Galligioni E. 2003; Pain and quality of life after surgery for breast cancer. Breast Cancer Res Treat. 80:39–48. DOI: 10.1023/A:1024435101619. PMID: 12889597.
Article33. Steel JL, Geller DA, Robinson TL, Savkova AY, Brower DS, Marsh JW, et al. 2014; Health-related quality of life as a prognostic factor in patients with advanced cancer. Cancer. 120:3717–3721. DOI: 10.1002/cncr.28902. PMID: 25104581. PMCID: PMC4239171.
Article34. Kramer JA, Curran D, Piccart M, de Haes JC, Bruning P, Klijn J, et al. 2000; Identification and interpretation of clinical and quality of life prognostic factors for survival and response to treatment in first-line chemotherapy in advanced breast cancer. Eur J Cancer. 36:1498–1506. DOI: 10.1016/S0959-8049(00)00144-1. PMID: 10930797.
Article35. Meyers CA, Hess KR, Yung WK, Levin VA. 2000; Cognitive function as a predictor of survival in patients with recurrent malignant glioma. J Clin Oncol. 18:646–650. DOI: 10.1200/JCO.2000.18.3.646. PMID: 10653880.
Article36. Poon RT, Fan ST, Yu WC, Lam BK, Chan FY, Wong J. 2001; A prospective longitudinal study of quality of life after resection of hepatocellular carcinoma. Arch Surg. 136:693–699. DOI: 10.1001/archsurg.136.6.693. PMID: 11387012.
Article37. Lis CG, Gupta D, Granick J, Grutsch JF. 2006; Can patient satisfaction with quality of life predict survival in advanced colorectal cancer? Support Care Cancer. 14:1104–1110. DOI: 10.1007/s00520-006-0100-3. PMID: 16819630.
Article38. Coates A, Porzsolt F, Osoba D. 1997; Quality of life in oncology practice: prognostic value of EORTC QLQ-C30 scores in patients with advanced malignancy. Eur J Cancer. 33:1025–1030. DOI: 10.1016/S0959-8049(97)00049-X. PMID: 9376182.
Article39. Dancey J, Zee B, Osoba D, Whitehead M, Lu F, Kaizer L, et al. 1997; Quality of life scores: an independent prognostic variable in a general population of cancer patients receiving chemotherapy. The National Cancer Institute of Canada Clinical Trials Group. Qual Life Res. 6:151–158. DOI: 10.1023/A:1026442201191. PMID: 9161115.40. Steffen LE, Vowles KE, Smith BW, Gan GN, Edelman MJ. 2018; Daily diary study of hope, stigma, and functioning in lung cancer patients. Health Psychol. 37:218–227. DOI: 10.1037/hea0000570. PMID: 29172604. PMCID: PMC5837918.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Pain, Sleep Disturbance, and Fatigue on the Quality of Life in Patients with Pancreatic Cancer Undergoing Chemotherapy
- Disease Perception, Stigma, Distress, Physical Symptom Experience and Quality of Life in Colorectal Cancer Patients Undergoing Chemotherapy: A Cross-Sectional Study
- Subjective Health Status, Mental Health, and Cancer Stigma in Long-term Cancer Survivors after Gastric Surgery
- The Relationships between Stigma, Distress, and Quality of Life in Patients with Lung Cancer
- Structural Equation Model of the Quality of Working Life among Cancer Survivors Returning to Work