Arch Hand Microsurg.
2023 Jun;28(2):110-113. 10.12790/ahm.23.0008.
Reconstruction of an abdominal wall defect using a latissimus dorsi musculocutaneous free flap after high-intensity focused ultrasound: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2542562
- DOI: http://doi.org/10.12790/ahm.23.0008
Abstract
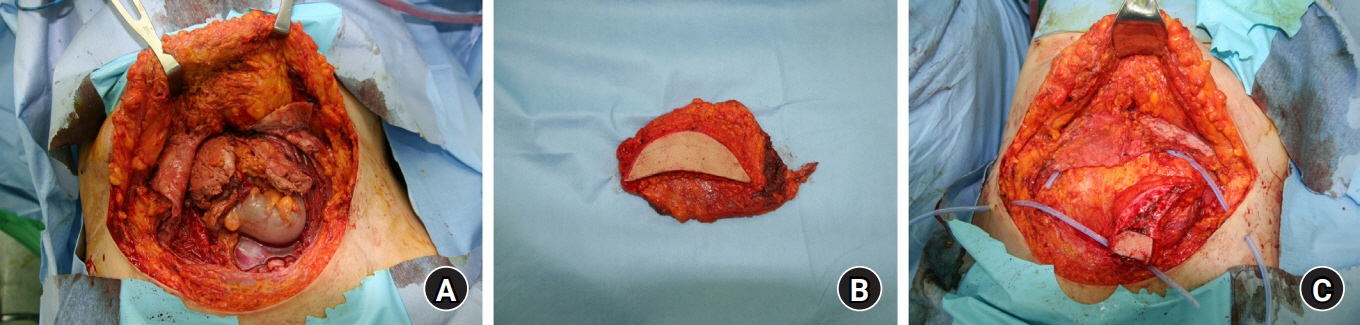
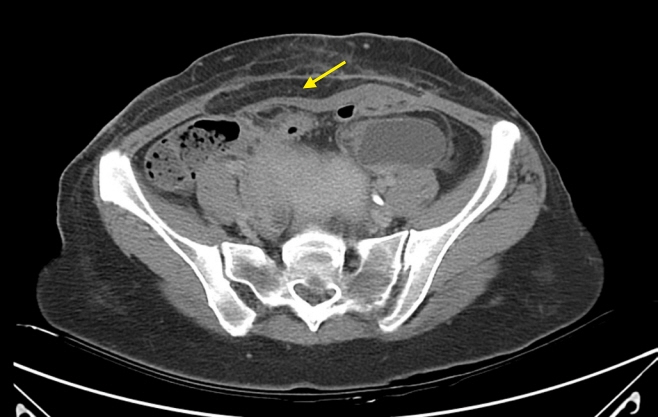
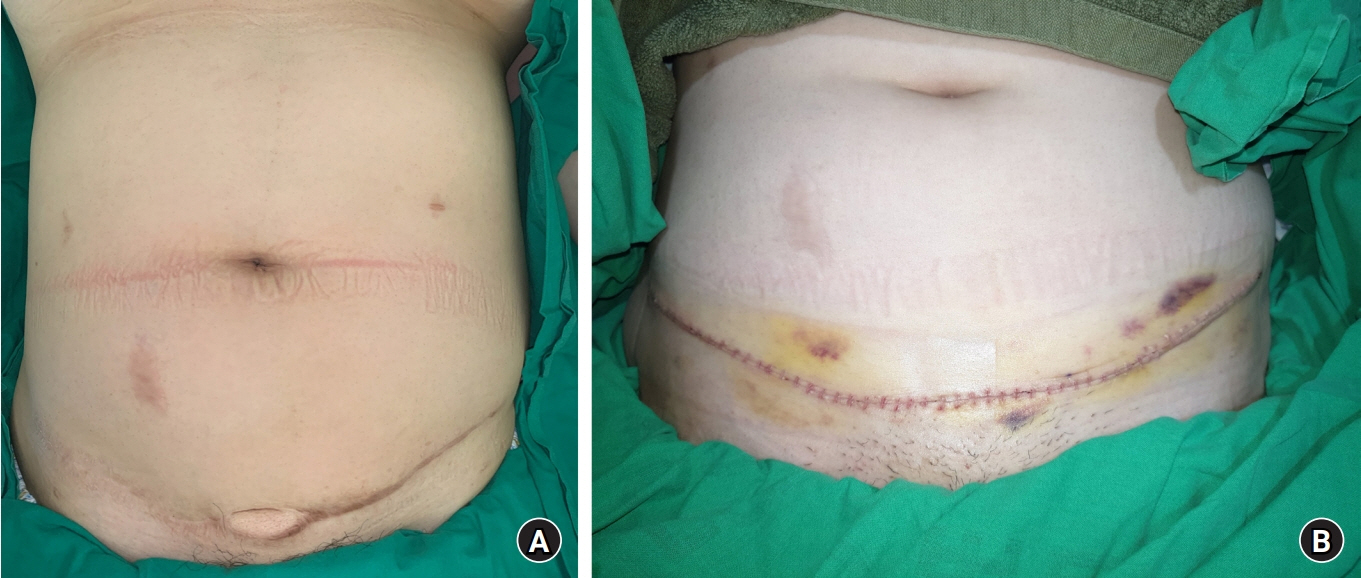
- High-intensity focused ultrasound (HIFU) ablation is a safe and effective minimally invasive option for treating uterine fibromas, but it can cause complications such as abdominal wall defects. Reconstruction of such defects can be challenging, but a latissimus dorsi musculocutaneous free flap can be used to restore the integrity of the myofascial layer and provide external cutaneous coverage. Herein, we present a case report of a 37-year-old woman who underwent HIFU for an 8-cm uterine fibroma and subsequently developed a large abdominal wall defect with necrosis of the rectus muscle. The latissimus dorsi musculocutaneous free flap was used to reconstruct the rectus muscle and cover the abdominal soft tissue, resulting in successful engraftment without complications. We present our experience using a latissimus dorsi musculocutaneous free flap to reconstruct a large HIFU-induced composite defect in the abdominal wall.
Figure
Reference
-
References
1. Kim HK, Kim D, Lee MK, et al. Three cases of complications after high-intensity focused ultrasound treatment in unmarried women. Obstet Gynecol Sci. 2015; 58:542–6.
Article2. Hwang DW, Song HS, Kim HS, Chun KC, Koh JW, Kim YA. Delayed intestinal perforation and vertebral osteomyelitis after high-intensity focused ultrasound treatment for uterine leiomyoma. Obstet Gynecol Sci. 2017; 60:490–3.
Article3. Clemens MW II, Butler CE. Abdominal wall reconstruction. In : Song DH, Neligan PC, editors. Plastic surgery. Vol. 4: Trunk and lower extremity. 4th ed. New York: Elsevier;2017. p. 275–89.4. Kim JJ, Moon JH, Lee NH, Kyung Moo Yang. Reconstruction of abdominal wall defects using periumbilical perforator-based island skin flap. Arch Hand Microsurg. 2001; 10:163–8.5. Hamrick MW, McGee-Lawrence ME, Frechette DM. Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne). 2016; 7:69.
Article6. Yang KM, Hahn HM. Reconstruction of a high-energy penetrating injury from the abdomen to the sacral area using a latissimus dorsi free flap with monofilament polypropylene mesh and pedicled flap rotation: a case report. Arch Hand Microsurg. 2022; 27:359–63.
Article7. Lee KT, Wiraatmadja ES, Mun GH. Free latissimus dorsi muscle-chimeric thoracodorsal artery perforator flaps for reconstruction of complicated defects: does muscle still have a place in the domain of perforator flaps? Ann Plast Surg. 2015; 74:565–72.8. Kim SW, Han SC, Hwang KT, Ahn BK, Kim JT, Kim YH. Reconstruction of infected abdominal wall defects using latissimus dorsi free flap. ANZ J Surg. 2013; 83:948–53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scalp Reconstruction and Cranioplasty using the Latissimus Dorsi Musculocutaneous Flap in a Patient with Recurrent Wound Dehiscence Accompanied by MRSA Infection
- Reconstruction of Extensive Lower Extermity Soft Tissue Defect Using Free Latissimus Dorsi Muscle Flap with STSG
- Reconstruction of Midface Defect with Latissimus Dorsi Myocutaneous Free Flap
- Reconstruction of a Large Infected Midline Abdominal Wall Defect Using a Latissimus Dorsi Free Flap
- Reconstruction of a temporal scalp defect without ipsilateral donor vessel possibilities using a local transposition flap and a latissimus dorsi free flap anastomosed to the contralateral side: a case report