J Stroke.
2023 May;25(2):282-290. 10.5853/jos.2023.00017.
Tissue Clock Beyond Time Clock: Endovascular Thrombectomy for Patients With Large Vessel Occlusion Stroke Beyond 24 Hours
- Affiliations
-
- 1Department of Neurology, Medical University of South Carolina (MUSC), Charleston, SC, USA
- 2Department of Neurology and Neurosurgery, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
- 3Department of Neurosurgery, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA
- 4Department of Neurology, Emory University School of Medicine, Atlanta, GA, USA
- 5Department of Neurosurgery, Hospital of the University of Pennsylvania, Penn Medicine, Philadelphia, PA, USA
- 6Department of Neurology, Cooper University Medical Center, Camden, NJ, USA
- 7Department of Neurology, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
- 8Departments of Neurology and Radiology, Boston University School of Medicine, Boston, MA, USA
- 9Department of Neurology, University of Miami, Miami, FL, USA
- 10Department of Neurology, Henry Ford Health, Detroit, MI, USA
- 11Department of Neurosurgery, University of Illinois at Chicago, Chicago, IL, USA
- 12Department of Neurosurgery, Baylor School of Medicine, Houston, TX, USA
- 13Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, NYC, NY, USA
- 14Departments of Neurology and Neurosurgery, Westchester Medical Center, Westchester, NY, USA
- KMID: 2542479
- DOI: http://doi.org/10.5853/jos.2023.00017
Abstract
- Background and Purpose
Randomized trials proved the benefits of mechanical thrombectomy (MT) for select patients with large vessel occlusion (LVO) within 24 hours of last-known-well (LKW). Recent data suggest that LVO patients may benefit from MT beyond 24 hours. This study reports the safety and outcomes of MT beyond 24 hours of LKW compared to standard medical therapy (SMT).
Methods
This is a retrospective analysis of LVO patients presented to 11 comprehensive stroke centers in the United States beyond 24 hours from LKW between January 2015 and December 2021. We assessed 90-day outcomes using the modified Rankin Scale (mRS).
Results
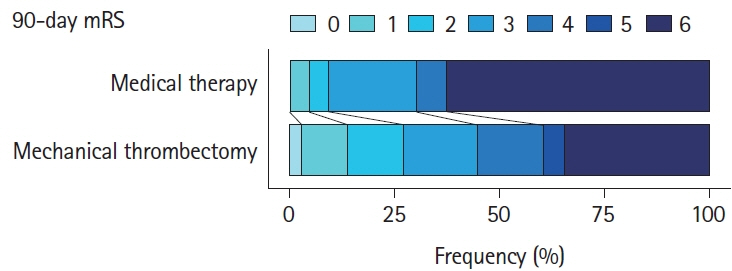
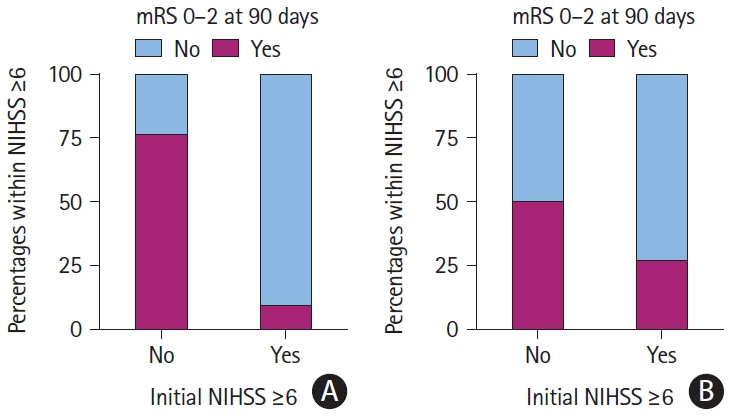
Of 334 patients presented with LVO beyond 24 hours, 64% received MT and 36% received SMT only. Patients who received MT were older (67±15 vs. 64±15 years, P=0.047) and had a higher baseline National Institutes of Health Stroke Scale (NIHSS; 16±7 vs.10±9, P<0.001). Successful recanalization (modified thrombolysis in cerebral infarction score 2b-3) was achieved in 83%, and 5.6% had symptomatic intracranial hemorrhage compared to 2.5% in the SMT group (P=0.19). MT was associated with mRS 0–2 at 90 days (adjusted odds ratio [aOR] 5.73, P=0.026), less mortality (34% vs. 63%, P<0.001), and better discharge NIHSS (P<0.001) compared to SMT in patients with baseline NIHSS ≥6. This treatment benefit remained after matching both groups. Age (aOR 0.94, P<0.001), baseline NIHSS (aOR 0.91, P=0.017), Alberta Stroke Program Early Computed Tomography (ASPECTS) score ≥8 (aOR 3.06, P=0.041), and collaterals scores (aOR 1.41, P=0.027) were associated with 90-day functional independence.
Conclusion
In patients with salvageable brain tissue, MT for LVO beyond 24 hours appears to improve outcomes compared to SMT, especially in patients with severe strokes. Patients’ age, ASPECTS, collaterals, and baseline NIHSS score should be considered before discounting MT merely based on LKW.
Keyword
Figure
Reference
-
References
1. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.2. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.
Article3. Haussen DC, Al-Bayati AR, Mohammaden MH, Sheth SA, Salazar-Marioni S, Linfante I, et al. The Society of Vascular and Interventional Neurology (SVIN) mechanical thrombectomy registry: methods and primary results. Stroke Vasc Interv Neurol. 2022; 2:e000234.
Article4. Dhillon PS, Butt W, Podlasek A, Barrett E, McConachie N, Lenthall R, et al. Endovascular thrombectomy beyond 24 hours from ischemic stroke onset: a propensity score matched cohort study. J Neurointerv Surg. 2023; 15:233–237.
Article5. Abou-Chebl A. Endovascular treatment of acute ischemic stroke may be safely performed with no time window limit in appropriately selected patients. Stroke. 2010; 41:1996–2000.
Article6. Purrucker JC, Ringleb PA, Seker F, Potreck A, Nagel S, Schönenberger S, et al. Leaving the day behind: endovascular therapy beyond 24h in acute stroke of the anterior and posterior circulation. Ther Adv Neurol Disord. 2022; 15:17562864221101083.
Article7. Heiss WD, Rosner G. Functional recovery of cortical neurons as related to degree and duration of ischemia. Ann Neurol. 1983; 14:294–301.
Article8. Rocha M, Jovin TG. Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke. 2018; 48:2621–2627.
Article9. Lee KJ, Kim BJ, Kim DE, Ryu WS, Han MK, Kim JT, et al. Nationwide estimation of eligibility for endovascular thrombectomy based on the DAWN trial. J Stroke. 2018; 20:277–279.
Article10. Filep RC, Marginean L, Stoian A, Bajko Z. Diagnostic and prognostic computed tomography imaging markers in basilar artery occlusion (review). Exp Ther Med. 2021; 22:954.
Article11. Souza LC, Yoo AJ, Chaudhry ZA, Payabvash S, Kemmling A, Schaefer PW, et al. Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol. 2012; 33:1331–1336.
Article12. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article13. Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007; 369:275–282.
Article14. Desai SM, Haussen DC, Aghaebrahim A, Al-Bayati AR, Santos R, Nogueira RG, et al. Thrombectomy 24 hours after stroke: beyond DAWN. J Neurointerv Surg. 2018; 10:1039–1042.
Article15. Sarraj A, Kleinig TJ, Hassan AE, Portela PC, Ortega-Gutierrez S, Abraham MG, et al. Association of endovascular thrombectomy vs medical management with functional and safety outcomes in patients treated beyond 24 hours of last known well: The SELECT Late Study. JAMA Neurol. 2023; 80:172–182.
Article16. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.17. Tiedt S, Herzberg M, Küpper C, Feil K, Kellert L, Dorn F, et al. Stroke etiology modifies the effect of endovascular treatment in acute stroke. Stroke. 2020; 51:1014–1016.18. Guglielmi V, LeCouffe NE, Zinkstok SM, Compagne KCJ, Eker R, Treurniet KM, et al. Collateral circulation and outcome in atherosclerotic versus cardioembolic cerebral large vessel occlusion. Stroke. 2019; 50:3360–3368.19. Lee D, Lee DH, Suh DC, Kim BJ, Kwon SU, Kwon HS, et al. Endovascular treatment in patients with cerebral artery occlusion of three different etiologies. J Stroke. 2020; 22:234–244.
Article20. McCarthy DJ, Tonetti DA, Stone J, Starke RM, Narayanan S, Lang MJ, et al. More expansive horizons: a review of endovascular therapy for patients with low NIHSS scores. J Neurointerv Surg. 2021; 13:146–151.
Article21. Goyal N, Tsivgoulis G, Malhotra K, Ishfaq MF, Pandhi A, Frohler MT, et al. Medical management vs mechanical thrombectomy for mild strokes: an international multicenter study and systematic review and meta-analysis. JAMA Neurol. 2020; 77:16–24.
Article22. Haussen DC, Bouslama M, Grossberg JA, Anderson A, Belagage S, Frankel M, et al. Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: an intention-to-treat analysis. J Neurointerv Surg. 2017; 9:917–921.
Article23. Sarraj A, Hassan A, Savitz SI, Grotta JC, Cai C, Parsha KN, et al. Endovascular thrombectomy for mild strokes: how low should we go? A multicenter cohort study. Stroke. 2018; 49:2398–2405.
Article24. Nguyen TN, Abdalkader M, Nagel S, Qureshi MM, Ribo M, Caparros F, et al. Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with large-vessel occlusion. JAMA Neurol. 2022; 79:22–31.
Article25. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article26. Bouslama M, Haussen DC, Rodrigues G, Barreira C, Frankel M, Nogueira RG. Novel selection paradigms for endovascular stroke treatment in the extended time window. J Neurol Neurosurg Psychiatry. 2021; 92:1152–1157.
Article27. Bouslama M, Bowen MT, Haussen DC, Dehkharghani S, Grossberg JA, Rebello LC, et al. Selection paradigms for large vessel occlusion acute ischemic stroke endovascular therapy. Cerebrovasc Dis. 2017; 44:277–284.
Article28. Albers GW, Lansberg MG, Brown S, Jadhav AP, Haussen DC, Martins SO, et al. Assessment of optimal patient selection for endovascular thrombectomy beyond 6 hours after symptom onset: a pooled analysis of the AURORA database. JAMA Neurol. 2021; 78:1064–1071.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Differences in mechanical thrombectomy for acute ischemic stroke on weekdays versus nights/ weekends in a Japanese primary stroke core center
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials