J Stroke.
2023 May;25(2):199-213. 10.5853/jos.2022.03552.
Occurrence of Ischemic Stroke in Patients With Atrial Fibrillation Receiving Non-Vitamin K Oral Anticoagulants: Causes and Prevention Strategies
- Affiliations
-
- 1Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Heart Vascular and Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2542471
- DOI: http://doi.org/10.5853/jos.2022.03552
Abstract
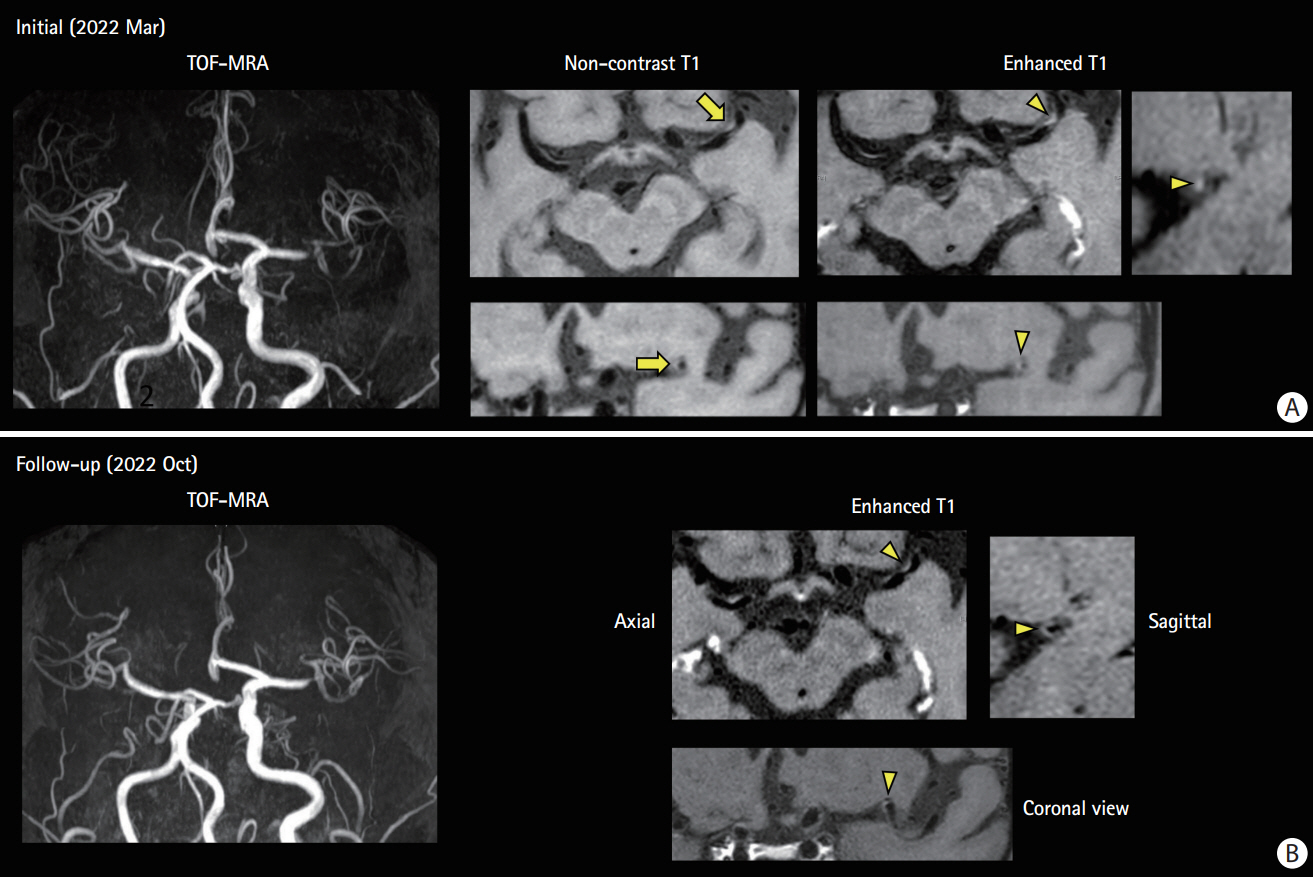
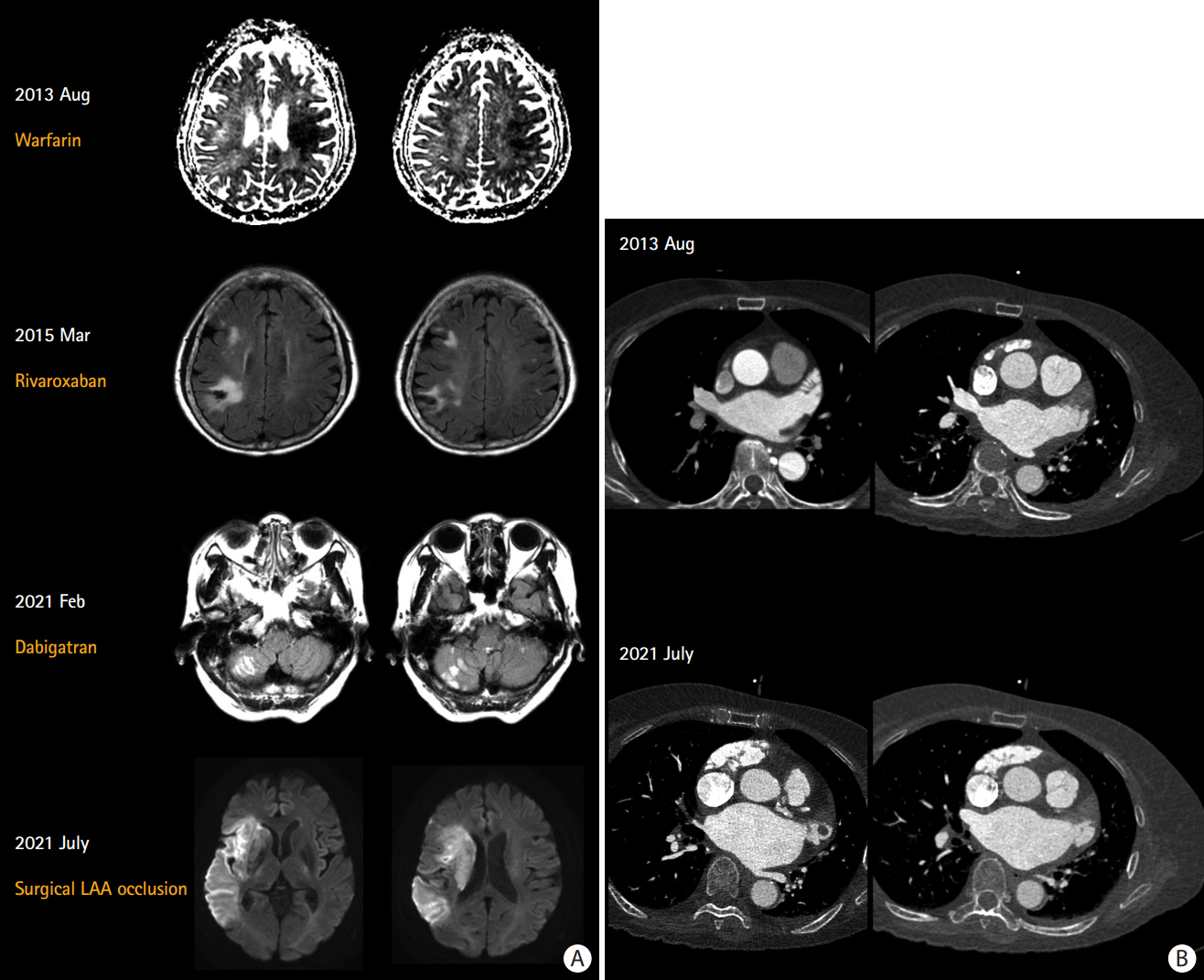
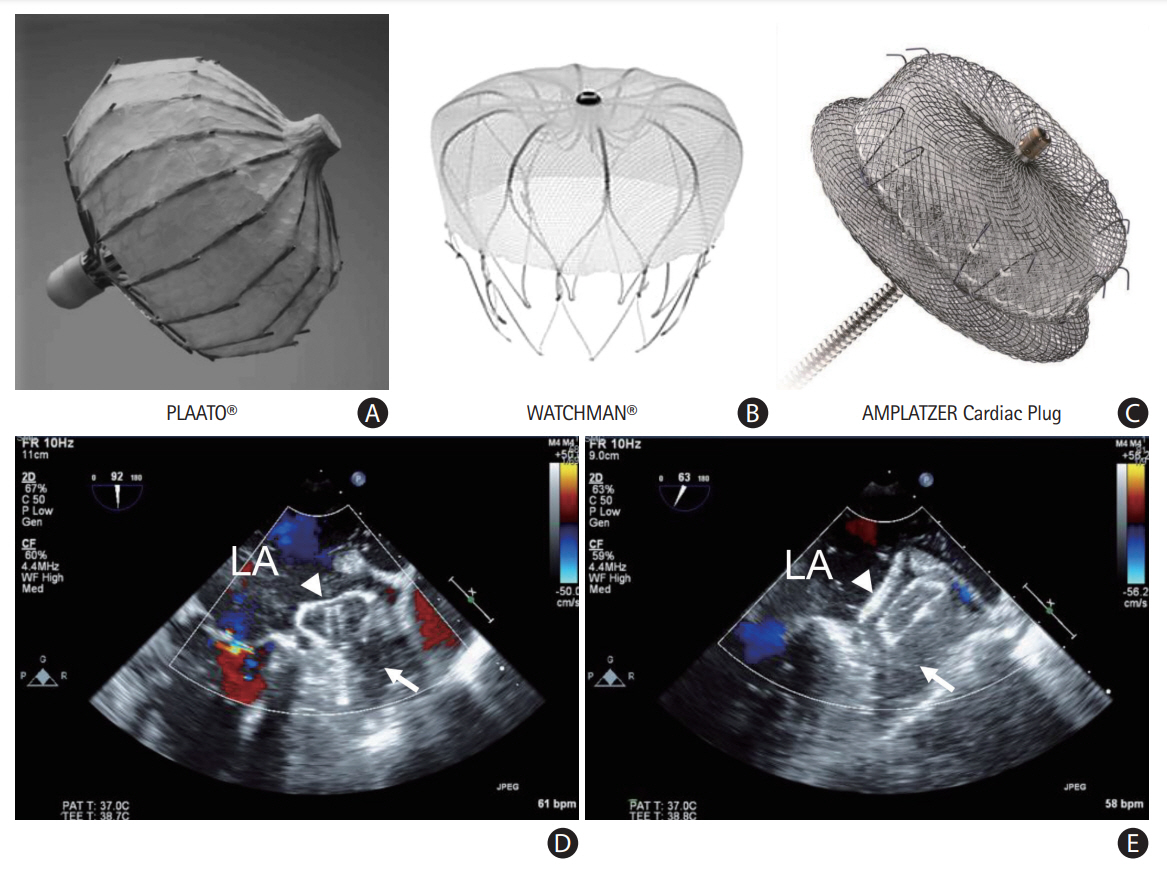
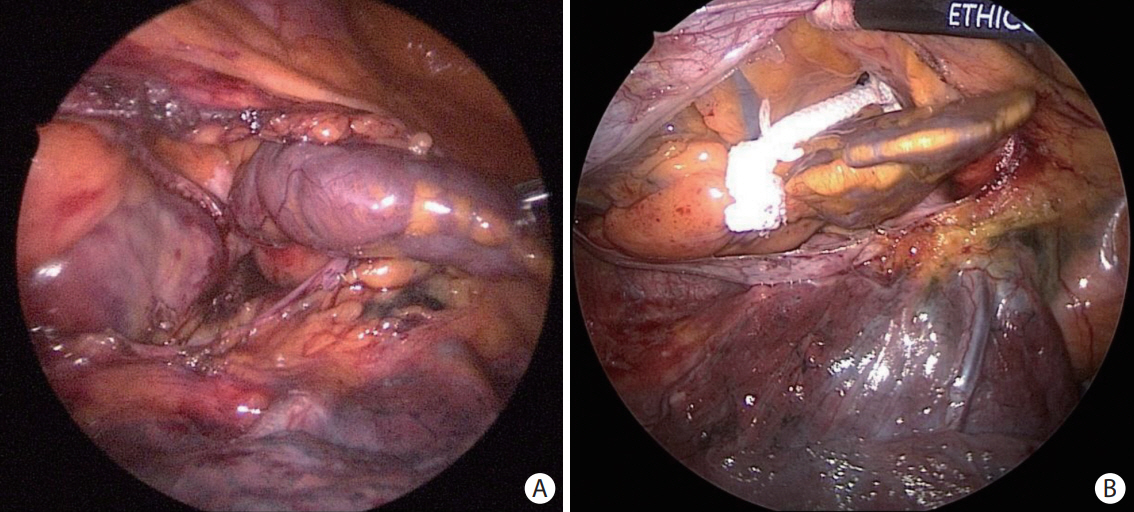
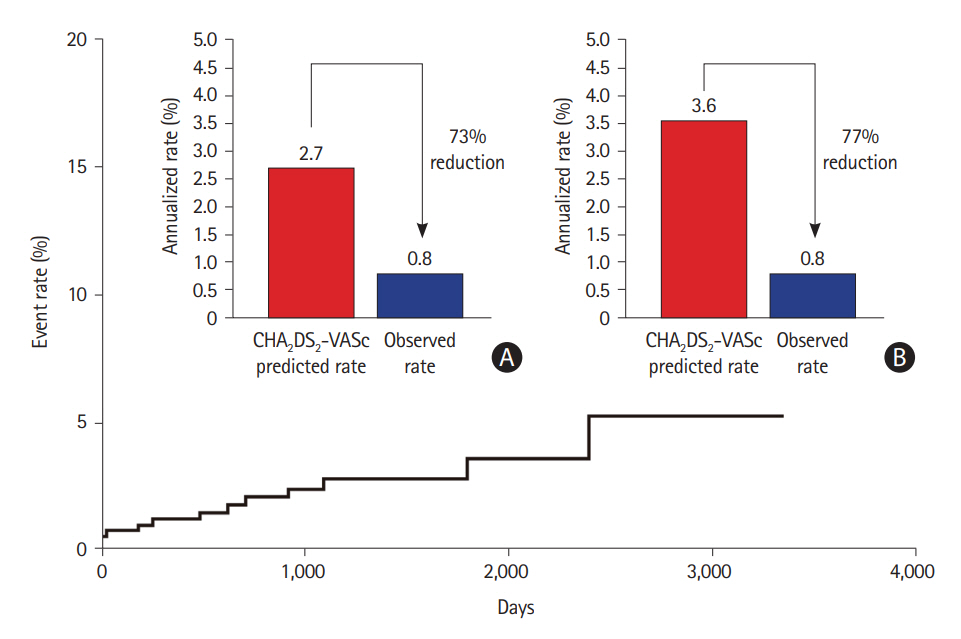
- Atrial fibrillation (AF) is a leading cause of cardioembolic stroke, which is often fatal or disabling. Prevention of stroke is crucial in AF management, and anticoagulation with non-vitamin K oral anticoagulants (NOACs) is the mainstay of AF management for stroke prevention. Because NOAC prescriptions have been surging worldwide, the development of acute ischemic stroke in patients with AF who receive NOAC treatment is an increasingly important issue in clinical practice. Moreover, these patients show a high risk of recurrence, with more than a 50% higher risk, than do patients with AF and no prior anticoagulation therapy. Careful evaluation is mandatory to determine possible causes of ischemic stroke during NOAC therapy. Differentiation of AF-unrelated stroke and demonstration of combined cardiac disease/systemic coagulopathy are important in these patients and may provide improved results in their treatment. In addition, ensuring appropriate dosing and good adherence to NOAC treatment is important. Cardioembolism, despite sufficient anticoagulation and no other causes, is the most common and challenging complication because switching to anticoagulants or adding antiplatelets to the treatment regimen does not reduce the risk of recurrent stroke, and there are no guidelines for this specific situation. This review article aimed to present the most updated data on the prevalence, causes, and secondary prevention strategies, specifically focusing on non-pharmacological approaches, together with relevant cases of AF in patients who developed ischemic stroke on NOAC therapy.
Keyword
Figure
Reference
-
References
1. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article2. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article3. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.
Article4. Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.
Article5. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021; 42:373–498.6. January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation. 2019; 140:e125–e151.
Article7. Tanaka K, Koga M, Lee KJ, Kim BJ, Park EL, Lee J, et al. Atrial fibrillation-associated ischemic stroke patients with prior anticoagulation have higher risk for recurrent stroke. Stroke. 2020; 51:1150–1157.
Article8. Yaghi S, Henninger N, Giles JA, Leon Guerrero C, Mistry E, Liberman AL, et al. Ischaemic stroke on anticoagulation therapy and early recurrence in acute cardioembolic stroke: the IAC study. J Neurol Neurosurg Psychiatry. 2021; 92:1062–1067.
Article9. Seiffge DJ, De Marchis GM, Koga M, Paciaroni M, Wilson D, Cappellari M, et al. Ischemic stroke despite oral anticoagulant therapy in patients with atrial fibrillation. Ann Neurol. 2020; 87:677–687.
Article10. Auer E, Frey S, Kaesmacher J, Hakim A, Seiffge DJ, Goeldlin M, et al. Stroke severity in patients with preceding direct oral anticoagulant therapy as compared to vitamin K antagonists. J Neurol. 2019; 266:2263–2272.
Article11. Grymonprez M, Simoens C, Steurbaut S, De Backer TL, Lahousse L. Worldwide trends in oral anticoagulant use in patients with atrial fibrillation from 2010 to 2018: a systematic review and meta-analysis. Europace. 2022; 24:887–898.
Article12. Yu Z, Yu L, Shan C. Trends of ambulatory oral anticoagulant prescription in five major cities of China, 2012-2017. BMC Health Serv Res. 2020; 20:209.
Article13. Bang OY, Hong KS, Heo JH. Asian patients with stroke plus atrial fibrillation and the dose of non-vitamin K oral anticoagulants. J Stroke. 2016; 18:169–178.
Article14. Paciaroni M, Caso V, Agnelli G, Mosconi MG, Giustozzi M, Seiffge DJ, et al. Recurrent ischemic stroke and bleeding in patients with atrial fibrillation who suffered an acute stroke while on treatment with nonvitamin K antagonist oral anticoagulants: the RENO-EXTEND study. Stroke. 2022; 53:2620–2627.15. Kim JS, Koo J, Shin DI, Kim BS, Kim J, Kim EG, et al. Apixaban for secondary stroke prevention: coexistant cerebral atherosclerosis may increase recurrent strokes. J Stroke. 2022; 24:118–127.
Article16. Kim SJ, Ryoo S, Kwon S, Park YK, Kim JP, Lee GY, et al. Is atrial fibrillation always a culprit of stroke in patients with atrial fibrillation plus stroke? Cerebrovasc Dis. 2013; 36:373–382.
Article17. Paciaroni M, Agnelli G, Caso V, Silvestrelli G, Seiffge DJ, Engelter S, et al. Causes and risk factors of cerebral ischemic events in patients with atrial fibrillation treated with non-vitamin K antagonist oral anticoagulants for stroke prevention. Stroke. 2019; 50:2168–2174.18. Jeong WK, Choi JH, Son JP, Lee S, Lee MJ, Choe YH, et al. Volume and morphology of left atrial appendage as determinants of stroke subtype in patients with atrial fibrillation. Heart Rhythm. 2016; 13:820–827.
Article19. Yao X, Abraham NS, Alexander GC, Crown W, Montori VM, Sangaralingham LR, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. 2016; 5:e003074.
Article20. Gabet A, Chatignoux E, Grave C, Vallée A, Tuppin P, Béjot Y, et al. Stroke incidence and death in atrial fibrillation patients newly treated with direct oral anticoagulants. Clin Epidemiol. 2021; 13:131–140.
Article21. Weitz JI, Eikelboom JW. Urgent need to measure effects of direct oral anticoagulants. Circulation. 2016; 134:186–188.
Article22. Kajy M, Mathew A, Ramappa P. Treatment failures of direct oral anticoagulants. Am J Ther. 2021; 28:e87–e95.
Article23. Steinberg BA, Shrader P, Pieper K, Thomas L, Allen LA, Ansell J, et al. Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes registry for better informed treatment of atrial fibrillation II). J Am Heart Assoc. 2018; 7:e007633.
Article24. Wang KL, Lip GY, Lin SJ, Chiang CE. Non–vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015; 46:2555–2561.
Article25. Heidbuchel H, Verhamme P, Alings M, Antz M, Diener HC, Hacke W, et al. Updated European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2015; 17:1467–1507.
Article26. Lin SY, Tang SC, Tsai LK, Yeh SJ, Huang CF, Jeng JS. Factors for recurrent stroke among Asian patients with non-valvular atrial fibrillation under non-vitamin K antagonist oral anticoagulant therapy. J Formos Med Assoc. 2020; 119:1799–1806.
Article27. Avezum A, Lopes RD, Schulte PJ, Lanas F, Gersh BJ, Hanna M, et al. Apixaban in comparison with warfarin in patients with atrial fibrillation and valvular heart disease: findings from the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial. Circulation. 2015; 132:624–632.
Article28. Ezekowitz MD, Nagarakanti R, Noack H, Brueckmann M, Litherland C, Jacobs M, et al. Comparison of dabigatran and warfarin in patients with atrial fibrillation and valvular heart disease: the RE-LY trial (Randomized Evaluation of Long-Term Anticoagulant Therapy). Circulation. 2016; 134:589–598.
Article29. Connolly SJ, Karthikeyan G, Ntsekhe M, Haileamlak A, El Sayed A, El Ghamrawy A, et al. Rivaroxaban in rheumatic heart disease-associated atrial fibrillation. N Engl J Med. 2022; 387:978–988.
Article30. Deitelzweig S, Keshishian AV, Zhang Y, Kang A, Dhamane AD, Luo X, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients with active cancer. JACC CardioOncol. 2021; 3:411–424.
Article31. Chan YH, Chao TF, Lee HF, Chen SW, Li PR, Liu JR, et al. Clinical outcomes in atrial fibrillation patients with a history of cancer treated with non-vitamin K antagonist oral anticoagulants: a nationwide cohort study. Stroke. 2021; 52:3132–3141.
Article32. Ordi-Ros J, Sáez-Comet L, Pérez-Conesa M, Vidal X, Riera-Mestre A, Castro-Salomó A, et al. Rivaroxaban versus vitamin K antagonist in antiphospholipid syndrome: a randomized non-inferiority trial. Ann Intern Med. 2019; 171:685–694.
Article33. Khairani CD, Bejjani A, Piazza G, Jimenez D, Monreal M, Chatterjee S, et al. Direct oral anticoagulants vs vitamin-K antagonists in thrombotic antiphospholipid syndrome: meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2022; Oct. 15. [Epub]. https://doi.org/10.1016/j.jacc.2022.10.008.
Article34. Polymeris AA, Meinel TR, Oehler H, Hölscher K, Zietz A, Scheitz JF, et al. Aetiology, secondary prevention strategies and outcomes of ischaemic stroke despite oral anticoagulant therapy in patients with atrial fibrillation. J Neurol Neurosurg Psychiatry. 2022; 93:588–598.
Article35. Ay H, Arsava EM, Gungor L, Greer D, Singhal AB, Furie KL, et al. Admission international normalized ratio and acute infarct volume in ischemic stroke. Ann Neurol. 2008; 64:499–506.
Article36. Macha K, Marsch A, Siedler G, Breuer L, Strasser EF, Engelhorn T, et al. Cerebral ischemia in patients on direct oral anticoagulants. Stroke. 2019; 50:873–879.
Article37. Xian Y, O’Brien EC, Liang L, Xu H, Schwamm LH, Fonarow GC, et al. Association of preceding antithrombotic treatment with acute ischemic stroke severity and in-hospital outcomes among patients with atrial fibrillation. JAMA. 2017; 317:1057–1067.
Article38. Rohla M, Weiss TW, Pecen L, Patti G, Siller-Matula JM, Schnabel RB, et al. Risk factors for thromboembolic and bleeding events in anticoagulated patients with atrial fibrillation: the prospective, multicentre observational PREvention oF thromboembolic events - European Registry in Atrial Fibrillation (PREFER in AF). BMJ Open. 2019; 9:e022478.
Article39. Budnik M, Gawałko M, Gorczyca I, Uzie¸bło-Z· yczkowska B, Krzesin´ski P, Kochanowski J, et al. Risk of left atrial appendage thrombus in patients with atrial fibrillation and chronic kidney disease. Cardiol J. 2022; 29:205–215.
Article40. Michalska A, Gorczyca I, Chrapek M, Kapłon-Cies´licka A, Uzie¸bło-Z· yczkowska B, Starzyk K, et al. Does the CHA2DS2-VASc scale sufficiently predict the risk of left atrial appendage thrombus in patients with diagnosed atrial fibrillation treated with non-vitamin K oral anticoagulants? Medicine (Baltimore). 2020; 99:e20570.
Article41. Shah M, Mobaligh N, Niku A, Shiota T, Siegel RJ, Rader F. Predictors of left atrial appendage thrombus despite NOAC use in nonvalvular atrial fibrillation and flutter. Int J Cardiol. 2020; 317:86–90.
Article42. Durmaz E, Karpuz MH, Bilgehan K, Ikitimur B, Ozmen E, Ebren C, et al. Left atrial thrombus in patients with atrial fibrillation and under oral anticoagulant therapy; 3-D transesophageal echocardiographic study. Int J Cardiovasc Imaging. 2020; 36:1097–1103.
Article43. Gawałko M, Budnik M, Uzie¸bło-Z· yczkowska B, Krzesin´ski P, Scisło P, Kochanowski J, et al. Decreased left atrial appendage emptying velocity as a link between atrial fibrillation type, heart failure and older age and the risk of left atrial thrombus in atrial fibrillation. Int J Clin Pract. 2020; 74:e13609.
Article44. Yamamoto M, Seo Y, Kawamatsu N, Sato K, Sugano A, Machino-Ohtsuka T, et al. Complex left atrial appendage morphology and left atrial appendage thrombus formation in patients with atrial fibrillation. Circ Cardiovasc Imaging. 2014; 7:337–343.
Article45. Fastner C, Szabo K, Samartzi M, Kruska M, Akin I, Platten M, et al. Treatment standards for direct oral anticoagulants in patients with acute ischemic stroke and non-valvular atrial fibrillation: a survey among German stroke units. PLoS One. 2022; 17:e0264122.
Article46. Sun H, Zhao Q, Wang Y, Lakin R, Liu X, Yu M, et al. Dabigatran as an alternative for atrial thrombosis resistant to rivaroxaban: a case report. Medicine (Baltimore). 2018; 97:e13623.47. Watanabe T, Shinoda Y, Ikeoka K, Minamisaka T, Fukuoka H, Inui H, et al. Dabigatran therapy resulting in the resolution of rivaroxaban-resistant left atrial appendage thrombi in patients with atrial fibrillation. Intern Med. 2017; 56:1977–1980.
Article48. Tokunaga K, Koga M, Itabashi R, Yamagami H, Todo K, Yoshimura S, et al. Prior anticoagulation and short–or long-term clinical outcomes in ischemic stroke or transient ischemic attack patients with nonvalvular atrial fibrillation. J Am Heart Assoc. 2019; 8:e010593.
Article49. Park YK, Lee MJ, Kim JH, Lee JS, Park RW, Kim GM, et al. Genetic and non-genetic factors affecting the quality of anticoagulation control and vascular events in atrial fibrillation. J Stroke Cerebrovasc Dis. 2017; 26:1383–1390.
Article50. Mocini D, Di Fusco SA, De Luca L, Caldarola P, Cipriani M, Corda M, et al. ANMCO position paper ‘appropriateness of prescribing direct oral anticoagulants in stroke and systemic thromboembolism prevention in adult patients with non-valvular atrial fibrillation’. Eur Heart J Suppl. 2022; 24(Suppl C):C278–C288.
Article51. Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996; 61:755–759.
Article52. Mahajan R, Brooks AG, Sullivan T, Lim HS, Alasady M, Abed HS, et al. Importance of the underlying substrate in determining thrombus location in atrial fibrillation: implications for left atrial appendage closure. Heart. 2012; 98:1120–1126.
Article53. Sievert H, Lesh MD, Trepels T, Omran H, Bartorelli A, Della Bella P, et al. Percutaneous left atrial appendage transcatheter occlusion to prevent stroke in high-risk patients with atrial fibrillation: early clinical experience. Circulation. 2002; 105:1887–1889.
Article54. Glikson M, Wolff R, Hindricks G, Mandrola J, Camm AJ, Lip GYH, et al. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion - an update. EuroIntervention. 2020; 15:1133–1180.
Article55. Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009; 374:534–542.
Article56. Holmes DR Jr, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, et al. Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014; 64:1–12.57. Boersma LV, Schmidt B, Betts TR, Sievert H, Tamburino C, Teiger E, et al. Implant success and safety of left atrial appendage closure with the WATCHMAN device: peri-procedural outcomes from the EWOLUTION registry. Eur Heart J. 2016; 37:2465–2474.
Article58. Reddy VY, Möbius-Winkler S, Miller MA, Neuzil P, Schuler G, Wiebe J, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with Watchman left atrial appendage closure technology). J Am Coll Cardiol. 2013; 61:2551–2556.
Article59. Kar S, Doshi SK, Sadhu A, Horton R, Osorio J, Ellis C, et al. Primary outcome evaluation of a next-generation left atrial appendage closure device: results from the PINNACLE FLX trial. Circulation. 2021; 143:1754–1762.
Article60. Lakkireddy D, Thaler D, Ellis CR, Swarup V, Sondergaard L, Carroll J, et al. Amplatzer amulet left atrial appendage occluder versus Watchman device for stroke prophylaxis (Amulet IDE): a randomized, controlled trial. Circulation. 2021; 144:1543–1552.
Article61. Osmancik P, Herman D, Neuzil P, Hala P, Taborsky M, Kala P, et al. Left atrial appendage closure versus direct oral anticoagulants in high-risk patients with atrial fibrillation. J Am Coll Cardiol. 2020; 75:3122–3135.
Article62. Wilber D, Lakkireddy DJ. Outcomes of adjunctive left atrial appendage ligation utilizing the LARIAT compared to pulmonary vein antral isolation alone: the aMAZE trial. American Heart Association’s Scientific Sessions (AHA) 2021 Nov 13-15; Boston, MA. Wilber D, Lakkireddy DJ. Outcomes of adjunctive left atrial appendage ligation utilizing the LARIAT compared to pulmonary vein antral isolation alone: the aMAZE trial. In : American Heart Association’s Scientific Sessions (AHA); 2021 Nov 13-15; Boston, MA.63. Fauchier L, Cinaud A, Brigadeau F, Lepillier A, Pierre B, Abbey S, et al. Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol. 2018; 71:1528–1536.
Article64. Holmes DR Jr, Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H, et al. Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll Cardiol. 2015; 65:2614–2623.
Article65. Galloo X, Carmeliet T, Prihadi EA, Lochy S, Scott B, Verheye S, et al. Left atrial appendage occlusion in recurrent ischaemic stroke, a multicentre experience. Acta Clin Belg. 2022; 77:255–260.
Article66. Katz ES, Tsiamtsiouris T, Applebaum RM, Schwartzbard A, Tunick PA, Kronzon I. Surgical left atrial appendage ligation is frequently incomplete: a transesophageal echocardiograhic study. J Am Coll Cardiol. 2000; 36:468–471.
Article67. Kanderian AS, Gillinov AM, Pettersson GB, Blackstone E, Klein AL. Success of surgical left atrial appendage closure: assessment by transesophageal echocardiography. J Am Coll Cardiol. 2008; 52:924–929.68. Ellis CR, Aznaurov SG, Patel NJ, Williams JR, Sandler KL, Hoff SJ, et al. Angiographic efficacy of the Atriclip left atrial appendage exclusion device placed by minimally invasive thoracoscopic approach. JACC Clin Electrophysiol. 2017; 3:1356–1365.
Article69. Toale C, Fitzmaurice GJ, Eaton D, Lyne J, Redmond KC. Outcomes of left atrial appendage occlusion using the AtriClip device: a systematic review. Interact Cardiovasc Thorac Surg. 2019; 29:655–662.
Article70. Caliskan E, Sahin A, Yilmaz M, Seifert B, Hinzpeter R, Alkadhi H, et al. Epicardial left atrial appendage AtriClip occlusion reduces the incidence of stroke in patients with atrial fibrillation undergoing cardiac surgery. Europace. 2018; 20:e105–e114.
Article71. Kim JY, Jeong DS, Park SJ, Park KM, Kim JS, On YK. Long-term efficacy and anticoagulation strategy of left atrial appendage occlusion during total thoracoscopic ablation of atrial fibrillation to prevent ischemic stroke. Front Cardiovasc Med. 2022; 9:853299.
Article72. Whitlock RP, Belley-Cote EP, Paparella D, Healey JS, Brady K, Sharma M, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med. 2021; 384:2081–2091.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-Vitamin K Oral Anticoagulants in Stroke Patients: Practical Issues
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- Stroke Prevention in Atrial Fibrillation
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation
- New oral anticoagulants