Clin Endosc.
2023 May;56(3):268-282. 10.5946/ce.2022.270.
Sex/gender differences in gastrointestinal endoscopy from the perspective of patients and gastroenterologists
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2542452
- DOI: http://doi.org/10.5946/ce.2022.270
Abstract
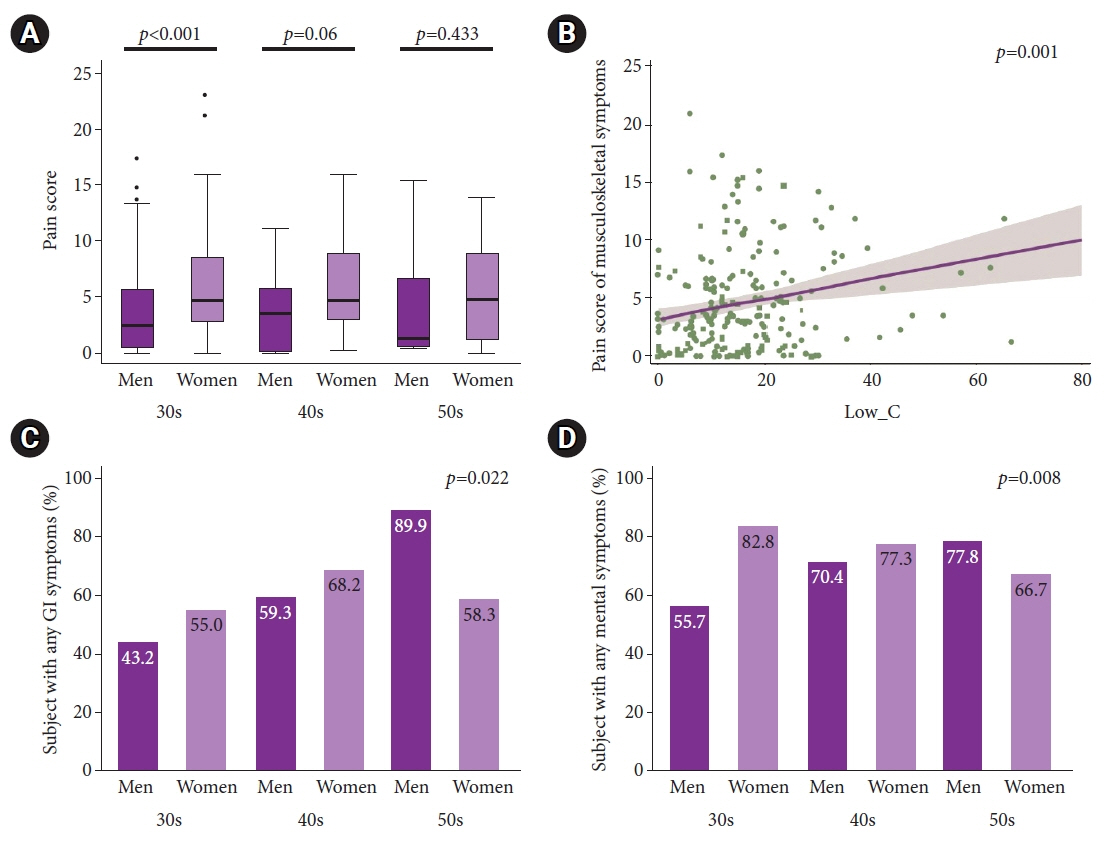
- The sex/gender of gastroenterologists impact patients’ satisfaction, compliance, and clinical outcomes. For instance, female gastrointestinal (GI) endoscopist–patient gender concordance improves health-related outcomes. This finding suggests that it is important to increase the number of female GI endoscopists. While the number of women in the field of gastroenterology is increasing in the United States and Korea by over 28.3%, it is not enough to account for the gender preferences of female patients. GI endoscopists are at a high risk of endoscopy-related injuries. However, there is a different distribution of muscle and fat; male endoscopists are more affected in their back, while females are more affected in the upper extremities. Women are more susceptible to endoscopy-related injuries than men. There is a correlation between the number of colonoscopies performed and musculoskeletal pain. Job satisfaction is lower in young female gastroenterologists (30’ and 40’) than in the opposite gender and other ages. Thus, it is important to address these issues in the development of GI endoscopy.
Keyword
Figure
Cited by 1 articles
-
How to Achieve Diversity, Equity, and Inclusion in The Korean Society of Gastroenterology?
Nayoung Kim, Kwangwoo Nam, Ki-Nam Shim, Hyo Jung Kim, Su Youn Nam, Sae Kyung Joo, Seun Ja Park, Yonghoon Choi, Yoon Ju Jung, Yong Sung Kim, Ja Kyung Kim, Seon Mee Park
Korean J Gastroenterol. 2025;85(1):22-30. doi: 10.4166/kjg.2024.092.
Reference
-
1. American Board of Internal Medicine. Percentage of first-year fellows by type of medical school attended [Internet]. Philadelphia: American Board of Internal Medicine;2023. [cited 2020 Aug 6]. Available from: https://www.abim.org/about/statistics-data/resident-fellow-workforce-data/first-year-fellows-by-type-of-medical-school-attended.aspx.2. Anglade P, Ibrahim H, Abdel-Razig S. Does provider gender matter in endoscopy?: an international perspective. Gastrointest Endosc. 2021; 93:1160–1168.3. Farraye FA, Wong M, Hurwitz S, et al. Barriers to endoscopic colorectal cancer screening: are women different from men? Am J Gastroenterol. 2004; 99:341–349.4. Varadarajulu S, Petruff C, Ramsey WH. Patient preferences for gender of endoscopists. Gastrointest Endosc. 2002; 56:170–173.5. Fidler H, Hartnett A, Cheng Man K, et al. Sex and familiarity of colonoscopists: patient preferences. Endoscopy. 2000; 32:481–482.6. Lee JM, Kim ES, Chun HJ, et al. Is there a change in patient preference for a female colonoscopist during the last decade in Korea? Clin Endosc. 2018; 51:72–79.7. Schneider A, Kanagarajan N, Anjelly D, et al. Importance of gender, socioeconomic status, and history of abuse on patient preference for endoscopist. Am J Gastroenterol. 2009; 104:340–348.8. Shah DK, Karasek V, Gerkin RD, et al. Sex preferences for colonoscopists and GI physicians among patients and health care professionals. Gastrointest Endosc. 2011; 74:122–127.9. Zapatier JA, Kumar AR, Perez A, et al. Preferences for ethnicity and sex of endoscopists in a Hispanic population in the United States. Gastrointest Endosc. 2011; 73:89–97.10. Varia A, Patel MK, Tanikella R, et al. Gender preference for the endoscopist among Hispanics: the results of a prospective study. J Immigr Minor Health. 2014; 16:990–993.11. Menees SB, Inadomi JM, Korsnes S, et al. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc. 2005; 62:219–223.12. Lee SY, Yu SK, Kim JH, et al. Link between a preference for women colonoscopists and social status in Korean women. Gastrointest Endosc. 2008; 67:273–277.13. Chong VH. Gender preference and implications for screening colonoscopy: impact of endoscopy nurses. World J Gastroenterol. 2012; 18:3590–3594.14. Lahat A, Assouline-Dayan Y, Katz LH, et al. The preference for an endoscopist specific sex: a link between ethnic origin, religious belief, socioeconomic status, and procedure type. Patient Prefer Adherence. 2013; 7:897–903.15. Pawa S, Banerjee P, Kothari S, et al. Are all endoscopy-related musculoskeletal injuries created equal?: results of a national gender-based survey. Am J Gastroenterol. 2021; 116:530–538.16. Janssen I, Heymsfield SB, Wang ZM, et al. Skeletal muscle mass and distribution in 468 men and women aged 18-88 yr. J Appl Physiol (1985). 2000; 89:81–88.17. Jang ES, Park SM, Park YS, et al. Work-life conflict and its health effects on Korean gastroenterologists according to age and sex. Dig Dis Sci. 2020; 65:86–95.18. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016; 388:2272–2281.19. Okagawa Y, Abe S, Yamada M, et al. Artificial intelligence in endoscopy. Dig Dis Sci. 2022; 67:1553–1572.20. Stoffel ST, Hirst Y, Ghanouni A, et al. Testing active choice for screening practitioner’s gender in endoscopy among disinclined women: an online experiment. J Med Screen. 2019; 26:98–103.21. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017; 177:206–213.22. Dahrouge S, Seale E, Hogg W, et al. A comprehensive assessment of family physician gender and quality of care: a cross-sectional analysis in Ontario, Canada. Med Care. 2016; 54:277–286.23. Janssen SM, Lagro-Janssen AL. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: a systematic review. Patient Educ Couns. 2012; 89:221–226.24. Hoke TP, Berger AA, Pan CC, et al. Assessing patients’ preferences for gender, age, and experience of their urogynecologic provider. Int Urogynecol J. 2020; 31:1203–1208.25. Nolen HA, Moore JX, Rodgers JB, et al. Patient preference for physician gender in the emergency department. Yale J Biol Med. 2016; 89:131–142.26. Reid I. Patients’ preference for male or female breast surgeons: questionnaire study. BMJ. 1998; 317:1051.27. Kerrison RS, McGregor LM, Marshall S, et al. Use of a 12 months’ self-referral reminder to facilitate uptake of bowel scope (flexible sigmoidoscopy) screening in previous non-responders: a London-based feasibility study. Br J Cancer. 2016; 114:751–758.28. Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018; 115:8569–8574.29. Marlicz W, Koulaouzidis A, Koulaouzidis G. Future endoscopy-related injuries will be of different types and gender-equal. Am J Gastroenterol. 2021; 116:1960–1961.30. Kokosis G, Dellon LA, Lidsky ME, et al. Prevalence of musculoskeletal symptoms and ergonomics among plastic surgery residents: results of a national survey and analysis of contributing factors. Ann Plast Surg. 2020; 85:310–315.31. Salvagioni DA, Melanda FN, Mesas AE, et al. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. 2017; 12:e0185781.32. Morais R, Vilas-Boas F, Pereira P, et al. Prevalence, risk factors and global impact of musculoskeletal injuries among endoscopists: a nationwide European study. Endosc Int Open. 2020; 8:E470–E480.33. Menees SB, Elta GH. Is the glass ceiling in gastroenterology gone? Gastrointest Endosc. 2016; 83:734–735.34. Association of American Medical Colleges. Active physicians by sex and specialty, 2017 [Internet]. Association of American Medical Colleges;2017. [cited 2020 Dec 20]. Available from: https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2017.35. Mohamed NA, Abdulhadi NN, Al-Maniri AA, et al. The trend of feminization of doctors’ workforce in Oman: is it a phenomenon that could rouse the health system? Hum Resour Health. 2018; 16:19.36. Diamond SJ, Thomas CR Jr, Desai S, et al. Gender differences in publication productivity, academic rank, and career duration among U.S. academic gastroenterology faculty. Acad Med. 2016; 91:1158–1163.37. Yung DE, Banfi T, Ciuti G, et al. Musculoskeletal injuries in gastrointestinal endoscopists: a systematic review. Expert Rev Gastroenterol Hepatol. 2017; 11:939–947.38. Marlicz W, Ren X, Robertson A, et al. Frontiers of robotic gastroscopy: a comprehensive review of robotic gastroscopes and technologies. Cancers (Basel). 2020; 12:2775.39. Nam SY, Nam K, Shim KN, et al. Rehabilitation program for improved musculoskeletal pain in gastrointestinal endoscopists: multicenter prospective cohort study. Gut Liver. 2023; Jan. 2. [Epub]. https://www.doi.org/10.5009/gnl220103.40. Coe IR, Wiley R, Bekker LG. Organisational best practices towards gender equality in science and medicine. Lancet. 2019; 393:587–593.41. Ibrahim H, Stadler DJ, Archuleta S, et al. Twelve tips to promote gender equity in international academic medicine. Med Teach. 2018; 40:962–968.42. Lyu HG, Davids JS, Scully RE, et al. Association of domestic responsibilities with career satisfaction for physician mothers in procedural vs nonprocedural fields. JAMA Surg. 2019; 154:689–695.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Gastroenterologists in Management of Obesity
- Sex and Gender Medicine in Pancreatobiliary Diseases
- Arterial Oxygen Desaturation during Non-sedated Diagnostic Gastrointestinal Endoscopy
- Female Endoscopists in Gastroenterology
- Gender Difference in Gallbladder Cancer: Focusing on the Clinical Characteristics, Treatment, and Prognosis of Korean Patients