Clin Exp Otorhinolaryngol.
2023 May;16(2):132-140. 10.21053/ceo.2022.01557.
Characteristics of Hearing Loss Among Older Adults in the Korean Genome and Epidemiology Study: A Community-Based Longitudinal Cohort Study With an 8-Year Follow-up
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2BK 21 Four R&E Center for Learning Health Systems, Korea University, Seoul, Korea
- 3Institute of Human Genomic Study, Korea University College of Medicine, Ansan, Korea
- 4Biomedical Research Center, Korea University Ansan Hospital, Ansan, Korea
- 5Department of Medical Informatics, Korea University College of Medicine, Seoul, Korea
- KMID: 2542354
- DOI: http://doi.org/10.21053/ceo.2022.01557
Abstract
Objectives
. This study investigated the 8-year incidence and progression of hearing loss (HL) and its types and examined the risk factors for changes in HL.
Methods
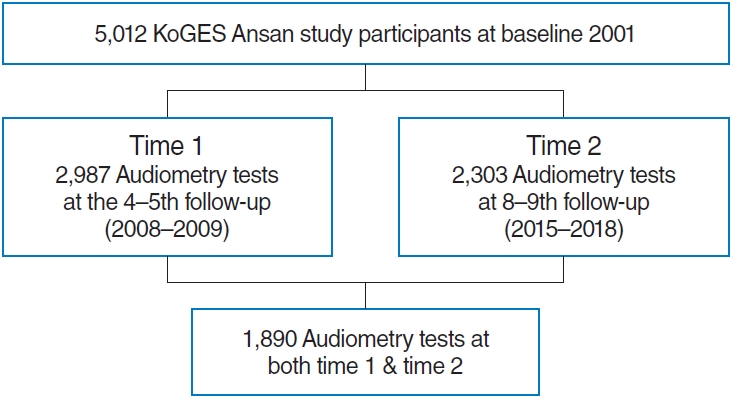
. This longitudinal cohort study analyzed data from the Korean Genome and Epidemiology Study (KoGES), an ongoing, prospective, community-based cohort study that has been conducted since 2001. Altogether, 1,890 residents of urban areas in Korea aged 45–75 years at time 1 (baseline) were included in the study. Pure-tone audiometry (PTA) testing was performed twice, at time 1 (2008–2009) and time 2 (2015–2018, follow-up), 8 years apart. HL grades were defined as seven mutually exclusive categories following the revised World Health Organization classification. Incidence was defined as PTA >20 dB HL in the better ear at time 2 among those without HL at time 1. Progression was defined as the progressive deterioration of HL among those with HL at time 1. The three types of HL constituted sensorineural (SNHL), conductive, and mixed HL.
Results
. At time 1, 36.40% of patients were diagnosed with HL, which increased to 51.64% at time 2. The 8-year incidence of HL was 27.20%, and progressive deterioration of HL occurred in 23.11% of those with HL. SNHL was the most common type of HL, and its prevalence markedly increased at time 2. Multivariate analysis demonstrated that the incidence of HL was significantly associated with increasing age, male sex (odds ratio [OR], 1.73; 95% confidence interval [CI], 1.07–2.81), and diabetes mellitus (OR, 1.43; 95% CI, 1.04–1.96). Alcohol consumption was a risk factor for HL deterioration among those with HL at time 1.
Conclusion
. The prevalence and deterioration of HL were extremely high among older adults, and age was the strongest risk factor for these changes. Therefore, timely screening and intervention are necessary to prevent HL and delay its deterioration among older adults.
Keyword
Figure
Reference
-
1. World Health Organization. WHO: 1 in 4 people projected to have hearing problems by 2050. World Health Organization;[cited 2023 April 10]. Available from: https://www.who.int/news/item/02-03-2021-who-1-in-4-people-projected-to-have-hearing-problems-by2050.2. Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009; Feb. 30(2):139–45.3. Ward WD. Endogenous factors related to susceptibility to damage from noise. Occup Med. 1995; Jul-Aug. 10(3):561–75.4. Contrera KJ, Betz J, Genther DJ, Lin FR. Association of hearing impairment and mortality in the National Health and Nutrition Examination Survey. JAMA Otolaryngol Head Neck Surg. 2015; Oct. 141(10):944–6.
Article5. Lawrence BJ, Jayakody DM, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing loss and depression in older adults: a systematic review and meta-analysis. Gerontologist. 2020; Apr. 60(3):e137–54.
Article6. Mick P, Kawachi I, Lin FR. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. 2014; Mar. 150(3):378–84.
Article7. Pronk M, Deeg DJ, Kramer SE. Hearing status in older persons: a significant determinant of depression and loneliness?: results from the longitudinal aging study amsterdam. Am J Audiol. 2013; Dec. 22(2):316–20.
Article8. Sung YK, Li L, Blake C, Betz J, Lin FR. Association of hearing loss and loneliness in older adults. J Aging Health. 2016; Sep. 28(6):979–94.
Article9. Liu CM, Lee CT. Association of hearing loss with dementia. JAMA Netw Open. 2019; Jul. 2(7):e198112.
Article10. Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018; Feb. 144(2):115–26.
Article11. Tseng YC, Liu SH, Lou MF, Huang GS. Quality of life in older adults with sensory impairments: a systematic review. Qual Life Res. 2018; Aug. 27(8):1957–71.
Article12. Nolan LS. Age-related hearing loss: why we need to think about sex as a biological variable. J Neurosci Res. 2020; Sep. 98(9):1705–20.
Article13. Cruickshanks KJ, Tweed TS, Wiley TL, Klein BE, Klein R, Chappell R, et al. The 5-year incidence and progression of hearing loss: the epidemiology of hearing loss study. Arch Otolaryngol Head Neck Surg. 2003; Oct. 129(10):1041–6.
Article14. Homans NC, Metselaar RM, Dingemanse JG, van der Schroeff MP, Brocaar MP, Wieringa MH, et al. Prevalence of age-related hearing loss, including sex differences, in older adults in a large cohort study. Laryngoscope. 2017; Mar. 127(3):725–30.
Article15. Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: the Epidemiology of Hearing Loss Study. Am J Epidemiol. 1998; Nov. 148(9):879–86.
Article16. Wilson BS, Tucci DL, Merson MH, O’Donoghue GM. Global hearing health care: new findings and perspectives. Lancet. 2017; Dec. 390(10111):2503–15.
Article17. World Health Organization. Deafness and hearing loss. World Health Organization;2021 [cited 2023 April 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss.18. Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M, et al. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013; Feb. 23(1):146–52.
Article19. Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011; May. 66(5):582–90.
Article20. GBD 2019 Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet. 2021; Mar. 397(10278):996–1009.21. Kim Y, Han BG; KoGES group. Cohort profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; Apr. 46(2):e20.
Article22. Olusanya BO, Davis AC, Hoffman HJ. Hearing loss grades and the international classification of functioning, disability and health. Bull World Health Organ. 2019; Oct. 97(10):725–8.23. Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000; Sep. 32(9 Suppl):S498–504.
Article24. Mitchell P, Gopinath B, Wang JJ, McMahon CM, Schneider J, Rochtchina E, et al. Five-year incidence and progression of hearing impairment in an older population. Ear Hear. 2011; Mar-Apr. 32(2):251–7.
Article25. Karlsmose B, Lauritzen T, Engberg M, Parving A. A five-year longitudinal study of hearing in a Danish rural population aged 31-50 years. Br J Audiol. 2000; Feb. 34(1):47–55.
Article26. Pirila T, Jounio-Ervasti K, Sorri M. Left-right asymmetries in hearing threshold levels in three age groups of a random population. Audiology. 1992; 31(3):150–61.
Article27. Moscicki EK, Elkins EF, Baum HM, McNamara PM. Hearing loss in the elderly: an epidemiologic study of the Framingham Heart Study Cohort. Ear Hear. 1985; Jul-Aug. 6(4):184–90.28. Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med. 2011; Nov. 171(20):1851–2.
Article29. Wild DC, Brewster MJ, Banerjee AR. Noise-induced hearing loss is exacerbated by long-term smoking. Clin Otolaryngol. 2005; Dec. 30(6):517–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Cochlear Implantation on Cognitive Function in Elderly Patients
- The Effects of Hearing Handicaps and Instrumental Activities of Daily Living on Hearing-Handicap-Related Quality of Life in Community-Dwelling Older Adults
- The Effect of Visual and Hearing Impairment on Depression and Cognitive Function in Community-dwelling Elderly: The Korean Longitudinal Study of Aging 2008
- Effects of Subjective Hearing Handicap and Perceived Stress on Quality of Communication Life of Older Adults
- Trajectories of Cognitive Function and Their Associated Factors in Community-Dwelling Older Adults by Living Arrangement Using the Korean Longitudinal Study of Aging