Korean Circ J.
2023 Apr;53(4):217-238. 10.4070/kcj.2023.0047.
Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Treatment
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul St. Mary’s Hospital, Catholic Research Institute for Intractable Cardiovascular Disease, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Cardiovascular Medicine, Chonnam National University Medical School, Gwangju, Korea
- 4Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 5Department of Cardiology, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 6Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 7Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 8Division of Cardiology, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 9Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 10Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2542293
- DOI: http://doi.org/10.4070/kcj.2023.0047
Abstract
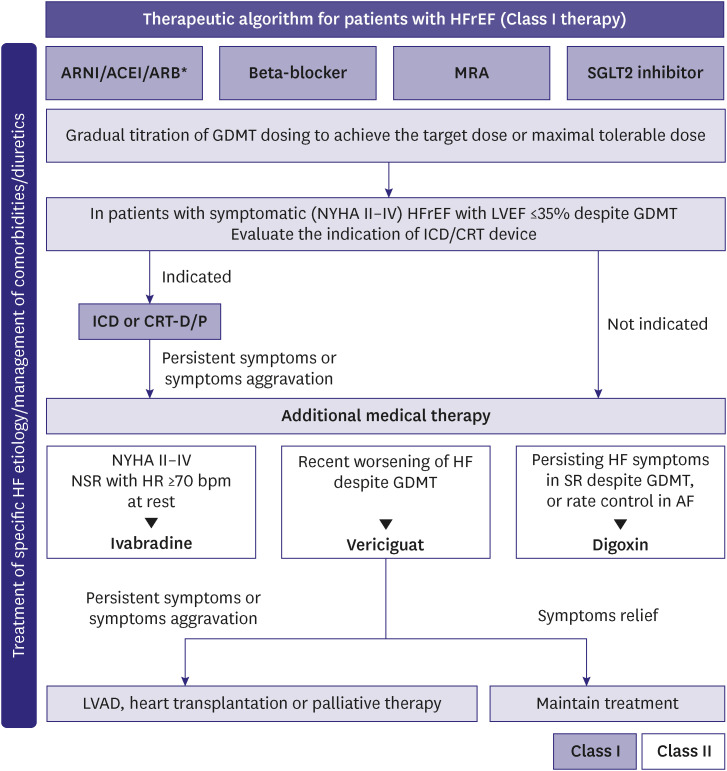
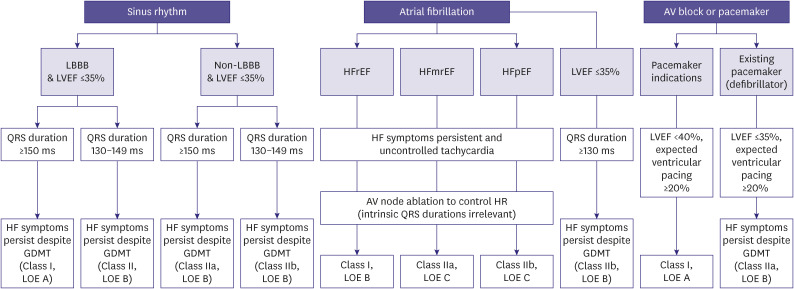
- The Korean Society of Heart Failure (KSHF) guidelines aim to provide physicians with evidencebased recommendations for the management of patients with heart failure (HF). After the first introduction of the KSHF guidelines in 2016, newer therapies for HF with reduced ejection fraction, HF with mildly reduced ejection fraction, and HF with preserved ejection fraction have since emerged. The current version has been updated based on international guidelines and research data on Korean patients with HF. Herein, we present Part II of these guidelines, which comprises treatment strategies to improve the outcomes of patients with HF.
Keyword
Figure
Cited by 2 articles
-
Should We Use Renin-Angiotensin-Aldosterone System Inhibitors Routinely in Patients With Hypertrophic Cardiomyopathy?
Jae-Hyeong Park
Korean Circ J. 2023;53(9):619-620. doi: 10.4070/kcj.2023.0161.Device-Detected Subclinical Atrial Fibrillation as Fire Under the Ashes
Seung-Jung Park
Korean Circ J. 2023;53(7):497-498. doi: 10.4070/kcj.2023.0136.
Reference
-
1. Kim MS, Lee JH, Kim EJ, et al. Korean guidelines for diagnosis and management of chronic heart failure. Korean Circ J. 2017; 47:555–643. PMID: 28955381.
Article2. Lee JH, Kim MS, Kim EJ, et al. KSHF Guidelines for the management of acute heart failure: Part I. Definition, epidemiology and diagnosis of acute heart failure. Korean Circ J. 2019; 49:1–21. PMID: 30637993.
Article3. Lee JH, Kim MS, Yoo BS, et al. KSHF Guidelines for the management of acute heart failure: Part II. Treatment of acute heart failure. Korean Circ J. 2019; 49:22–45. PMID: 30637994.
Article4. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42:3599–3726. PMID: 34447992.
Article5. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022; 79:e263–e421. PMID: 35379503.6. Kim ES, Youn JC, Baek SH. Update on the pharmacotherapy of heart failure with reduced ejection fraction. Cardiovasc Prev Pharmacother. 2020; 2:113–133.
Article7. Choi HM, Park MS, Youn JC. Update on heart failure management and future directions. Korean J Intern Med. 2019; 34:11–43. PMID: 30612416.
Article8. Halliday BP, Wassall R, Lota AS, et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet. 2019; 393:61–73. PMID: 30429050.
Article9. Choi KH, Lee GY, Choi JO, et al. Effects of angiotensin receptor blocker at discharge in patients with heart failure with reduced ejection fraction: Korean Acute Heart Failure (KorAHF) registry. Int J Cardiol. 2018; 257:168–176. PMID: 29506690.
Article10. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993–1004. PMID: 25176015.
Article11. Senni M, McMurray JJ, Wachter R, et al. Impact of systolic blood pressure on the safety and tolerability of initiating and up-titrating sacubitril/valsartan in patients with heart failure and reduced ejection fraction: insights from the TITRATION study. Eur J Heart Fail. 2018; 20:491–500. PMID: 29164797.
Article12. Januzzi JL Jr, Prescott MF, Butler J, et al. Association of change in N-terminal pro-B-type natriuretic peptide following initiation of sacubitril-valsartan treatment with cardiac structure and function in patients with heart failure with reduced ejection fraction. JAMA. 2019; 322:1085–1095. PMID: 31475295.
Article13. Khariton Y, Fonarow GC, Arnold SV, et al. Association between sacubitril/valsartan initiation and health status outcomes in heart failure with reduced ejection fraction. JACC Heart Fail. 2019; 7:933–941. PMID: 31521679.
Article14. Myhre PL, Vaduganathan M, Claggett B, et al. B-type natriuretic peptide during treatment with sacubitril/valsartan: the PARADIGM-HF trial. J Am Coll Cardiol. 2019; 73:1264–1272. PMID: 30846338.15. Velazquez EJ, Morrow DA, DeVore AD, et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med. 2019; 380:539–548. PMID: 30415601.
Article16. DeVore AD, Braunwald E, Morrow DA, et al. Initiation of angiotensin-neprilysin inhibition after acute decompensated heart failure: secondary analysis of the open-label extension of the PIONEER-HF trial. JAMA Cardiol. 2020; 5:202–207. PMID: 31825471.
Article17. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999; 353:9–13. PMID: 10023943.18. Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001; 344:1651–1658. PMID: 11386263.
Article19. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999; 353:2001–2007. PMID: 10376614.20. Hjalmarson A, Goldstein S, Fagerberg B, et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). JAMA. 2000; 283:1295–1302. PMID: 10714728.
Article21. Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005; 26:215–225. PMID: 15642700.
Article22. Lim NK, Lee SE, Lee HY, et al. Risk prediction for 30-day heart failure-specific readmission or death after discharge: data from the Korean Acute Heart Failure (KorAHF) registry. J Cardiol. 2019; 73:108–113. PMID: 30360893.
Article23. Seo WW, Park JJ, Park HA, et al. Guideline-directed medical therapy in elderly patients with heart failure with reduced ejection fraction: a cohort study. BMJ Open. 2020; 10:e030514.
Article24. Choi KH, Choi JO, Jeon ES, et al. Guideline-directed medical therapy for patients with heart failure with midrange ejection fraction: a patient-pooled analysis from the KorHF and KorAHF registries. J Am Heart Assoc. 2018; 7:e009806. PMID: 30608208.
Article25. Ahn MS, Yoo BS, Yoon J, et al. Guideline-directed therapy at discharge in patients with heart failure and atrial fibrillation. Heart. 2020; 106:292–298. PMID: 31492703.
Article26. Kim KA, Kim ES, Youn JC, et al. A dose-response relationship of renin-angiotensin system blockers and beta-blockers in patients with acute heart failure syndrome: a nationwide prospective cohort study. Eur Heart J Cardiovasc Pharmacother. 2022; 8:587–599. PMID: 35088082.
Article27. Cho MS, Kim MS, Lee SE, et al. Outcomes after predischarge initiation of β-blocker in patients hospitalized for severe decompensated heart failure requiring inotropic therapy. Can J Cardiol. 2018; 34:1145–1152. PMID: 30170669.
Article28. Park JJ, Park HA, Cho HJ, et al. β-Blockers and 1-year postdischarge mortality for heart failure and reduced ejection fraction and slow discharge heart rate. J Am Heart Assoc. 2019; 8:e011121. PMID: 30755071.
Article29. Kim HJ, Jo SH, Lee MH, Seo WW, Choi JO, Ryu KH. The effect of beta-blockers in acute heart failure according to heart rate. Korean J Intern Med. 2021; 36:898–905. PMID: 32872744.
Article30. Choi KH, Lee GY, Choi JO, et al. The mortality benefit of carvedilol versus bisoprolol in patients with heart failure with reduced ejection fraction. Korean J Intern Med. 2019; 34:1030–1039. PMID: 30317846.
Article31. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999; 341:709–717. PMID: 10471456.
Article32. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003; 348:1309–1321. PMID: 12668699.
Article33. Na SJ, Youn JC, Lee HS, et al. The prescription characteristics, efficacy and safety of spironolactone in real-world patients with acute heart failure syndrome: a prospective nationwide cohort study. Front Cardiovasc Med. 2022; 9:791446. PMID: 35274010.
Article34. Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020; 383:1413–1424. PMID: 32865377.35. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019; 381:1995–2008. PMID: 31535829.
Article36. Ellison DH. The physiologic basis of diuretic synergism: its role in treating diuretic resistance. Ann Intern Med. 1991; 114:886–894. PMID: 2014951.
Article37. Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010; 376:875–885. PMID: 20801500.
Article38. Swedberg K, Komajda M, Böhm M, et al. Effects on outcomes of heart rate reduction by ivabradine in patients with congestive heart failure: is there an influence of beta-blocker dose?: findings from the SHIFT (Systolic Heart failure treatment with the I(f) inhibitor ivabradine Trial) study. J Am Coll Cardiol. 2012; 59:1938–1945. PMID: 22617188.
Article39. Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020; 382:1883–1893. PMID: 32222134.
Article40. Ziff OJ, Kotecha D. Digoxin: the good and the bad. Trends Cardiovasc Med. 2016; 26:585–595. PMID: 27156593.
Article41. Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997; 336:525–533. PMID: 9036306.42. Sonnenblick M, Abraham AS, Meshulam Z, Eylath U. Correlation between manifestations of digoxin toxicity and serum digoxin, calcium, potassium, and magnesium concentrations and arterial pH. Br Med J (Clin Res Ed). 1983; 286:1089–1091.
Article43. Bavendiek U, Aguirre Davila L, Koch A, Bauersachs J. Assumption versus evidence: the case of digoxin in atrial fibrillation and heart failure. Eur Heart J. 2017; 38:2095–2099. PMID: 28065909.
Article44. Ingelfinger JA, Goldman P. The serum digitalis concentration--does it diagnose digitalis toxicity? N Engl J Med. 1976; 294:867–870. PMID: 1250314.
Article45. Renneboog B, Musch W, Vandemergel X, Manto MU, Decaux G. Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med. 2006; 119:71.e1–71.e8.
Article46. Ghali JK, Koren MJ, Taylor JR, et al. Efficacy and safety of oral conivaptan: a V1A/V2 vasopressin receptor antagonist, assessed in a randomized, placebo-controlled trial in patients with euvolemic or hypervolemic hyponatremia. J Clin Endocrinol Metab. 2006; 91:2145–2152. PMID: 16522696.
Article47. Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006; 355:2099–2112. PMID: 17105757.
Article48. Gheorghiade M, Konstam MA, Burnett JC Jr, et al. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007; 297:1332–1343. PMID: 17384438.
Article49. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–259. PMID: 16855265.
Article50. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006; 355:260–269. PMID: 16855266.
Article51. Youn JC, Ahn Y, Jung HO. Pathophysiology of heart failure with preserved ejection fraction. Heart Fail Clin. 2021; 17:327–335. PMID: 34051965.
Article52. Shim CY. Heart failure with preserved ejection fraction: the major unmet need in cardiology. Korean Circ J. 2020; 50:1051–1061. PMID: 33150751.
Article53. Borlaug BA. Evaluation and management of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2020; 17:559–573. PMID: 32231333.
Article54. Faris R, Flather M, Purcell H, Henein M, Poole-Wilson P, Coats A. Current evidence supporting the role of diuretics in heart failure: a meta analysis of randomised controlled trials. Int J Cardiol. 2002; 82:149–158. PMID: 11853901.
Article55. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID: 30165516.56. Kitzman DW, Brubaker P, Morgan T, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2016; 315:36–46. PMID: 26746456.
Article57. Obokata M, Reddy YN, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017; 136:6–19. PMID: 28381470.
Article58. Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021; 385:1451–1461. PMID: 34449189.59. Butler J, Packer M, Filippatos G, et al. Effect of empagliflozin in patients with heart failure across the spectrum of left ventricular ejection fraction. Eur Heart J. 2022; 43:416–426. PMID: 34878502.
Article60. Jhund PS, Kondo T, Butt JH, et al. Dapagliflozin across the range of ejection fraction in patients with heart failure: a patient-level, pooled meta-analysis of DAPA-HF and DELIVER. Nat Med. 2022; 28:1956–1964. PMID: 36030328.
Article61. Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022; 387:1089–1098. PMID: 36027570.62. Vaduganathan M, Docherty KF, Claggett BL, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet. 2022; 400:757–767. PMID: 36041474.
Article63. Solomon SD, McMurray JJV, Anand IS, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019; 381:1609–1620. PMID: 31475794.
Article64. Solomon SD, Vaduganathan M, L Claggett B, et al. Sacubitril/valsartan across the spectrum of ejection fraction in heart failure. Circulation. 2020; 141:352–361. PMID: 31736342.
Article65. Vaduganathan M, Claggett BL, Desai AS, et al. Prior heart failure hospitalization, clinical outcomes, and response to sacubitril/valsartan compared with valsartan in HFpEF. J Am Coll Cardiol. 2020; 75:245–254. PMID: 31726194.
Article66. O’Connor CM. Meet me in the middle: lessons from the cardiorenal advisory committee for sacubitril/valsartan in HFpEF. JACC Heart Fail. 2021; 9:161–163. PMID: 33509378.67. Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014; 370:1383–1392. PMID: 24716680.
Article68. Pfeffer MA, Claggett B, Assmann SF, et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 2015; 131:34–42. PMID: 25406305.
Article69. de Denus S, O’Meara E, Desai AS, et al. Spironolactone metabolites in TOPCAT - new insights into regional variation. N Engl J Med. 2017; 376:1690–1692. PMID: 28445660.
Article70. Solomon SD, Claggett B, Lewis EF, et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016; 37:455–462. PMID: 26374849.
Article71. Cho JH, Choe WS, Cho HJ, et al. Comparison of characteristics and 3-year outcomes in patients with acute heart failure with preserved, mid-range, and reduced ejection fraction. Circ J. 2019; 83:347–356. PMID: 30404976.
Article72. Connolly SJ, Hallstrom AP, Cappato R, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg. Canadian Implantable Defibrillator Study. Eur Heart J. 2000; 21:2071–2078. PMID: 11102258.
Article73. O’Brien T, Park MS, Youn JC, Chung ES. The past, present and future of cardiac resynchronization therapy. Korean Circ J. 2019; 49:384–399. PMID: 31074211.
Article74. Lee SH, Park SJ, Kim JS, Shin DH, Cho DK, On YK. Mid-term outcomes in patients implanted with cardiac resynchronization therapy. J Korean Med Sci. 2014; 29:1651–1657. PMID: 25469065.
Article75. Uhm JS, Oh J, Cho IJ, et al. Left ventricular end-systolic volume can predict 1-year hierarchical clinical composite end point in patients with cardiac resynchronization therapy. Yonsei Med J. 2019; 60:48–55. PMID: 30554490.
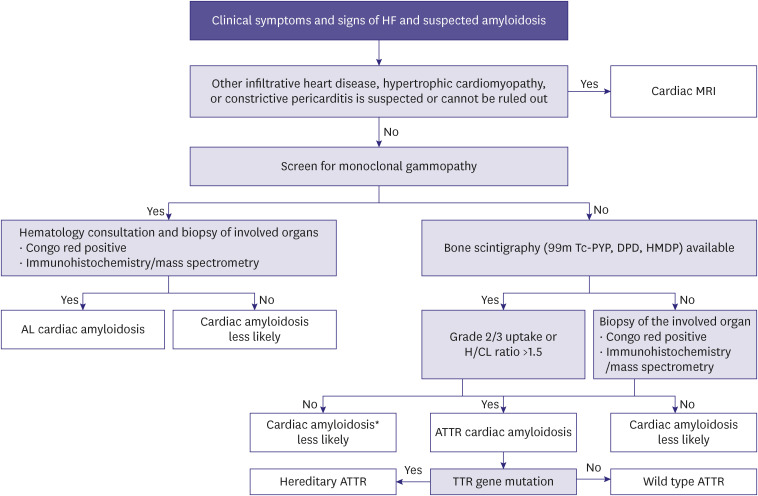
Article76. Jang SY, Kim D, Choi JO, Jeon ES. Incidence, cause of death, and survival of amyloidosis in Korea: a retrospective population-based study. Int J Heart Fail. 2021; 3:172–178. PMID: 36262641.
Article77. Garcia-Pavia P, Rapezzi C, Adler Y, et al. Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2021; 42:1554–1568. PMID: 33825853.
Article78. Kittleson MM, Maurer MS, Ambardekar AV, et al. Cardiac amyloidosis: evolving diagnosis and management: a scientific statement from the American Heart Association. Circulation. 2020; 142:e7–22. PMID: 32476490.
Article79. Kim D, Choi JO, Kim K, Kim SJ, Jeon ES. Untangling amyloidosis: recent advances in cardiac amyloidosis. Int J Heart Fail. 2020; 2:231–239. PMID: 36262171.
Article80. Jung MH, Chang S, Han EJ, Youn JC. Multimodal imaging and biomarkers in cardiac amyloidosis. Diagnostics (Basel). 2022; 12:627. PMID: 35328180.
Article81. Maurer MS, Schwartz JH, Gundapaneni B, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018; 379:1007–1016. PMID: 30145929.
Article82. Damy T, Garcia-Pavia P, Hanna M, et al. Efficacy and safety of tafamidis doses in the Tafamidis in Transthyretin Cardiomyopathy Clinical Trial (ATTR-ACT) and long-term extension study. Eur J Heart Fail. 2021; 23:277–285. PMID: 33070419.
Article83. Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013; 34:2636–2648. 2648a–2648d. PMID: 23824828.
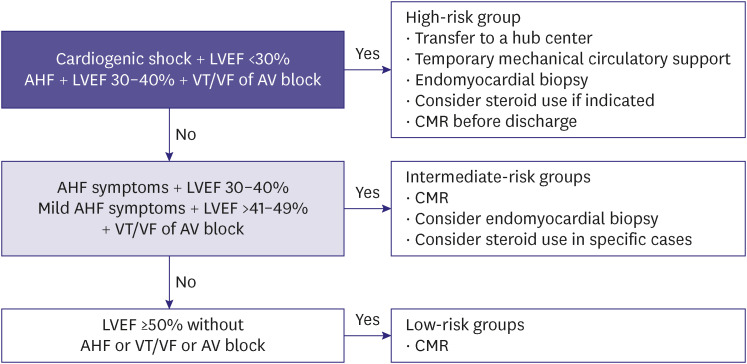
Article84. Cooper LT Jr, Keren A, Sliwa K, Matsumori A, Mensah GA. The global burden of myocarditis: part 1: a systematic literature review for the Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Glob Heart. 2014; 9:121–129. PMID: 25432122.85. Heymans S, Eriksson U, Lehtonen J, Cooper LT Jr. The quest for new approaches in myocarditis and inflammatory cardiomyopathy. J Am Coll Cardiol. 2016; 68:2348–2364. PMID: 27884253.
Article86. Tschöpe C, Ammirati E, Bozkurt B, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. 2021; 18:169–193. PMID: 33046850.
Article87. Ammirati E, Frigerio M, Adler ED, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020; 13:e007405. PMID: 33176455.
Article88. Youn JC, Shim HS, Lee JS, et al. Detailed pathologic evaluation on endomyocardial biopsy provides long-term prognostic information in patients with acute myocarditis. Cardiovasc Pathol. 2014; 23:139–144. PMID: 24529879.
Article89. D’Ambrosio A, Patti G, Manzoli A, et al. The fate of acute myocarditis between spontaneous improvement and evolution to dilated cardiomyopathy: a review. Heart. 2001; 85:499–504. PMID: 11302994.
Article90. Tschöpe C, Cooper LT, Torre-Amione G, Van Linthout S. Management of myocarditis-related cardiomyopathy in adults. Circ Res. 2019; 124:1568–1583. PMID: 31120823.
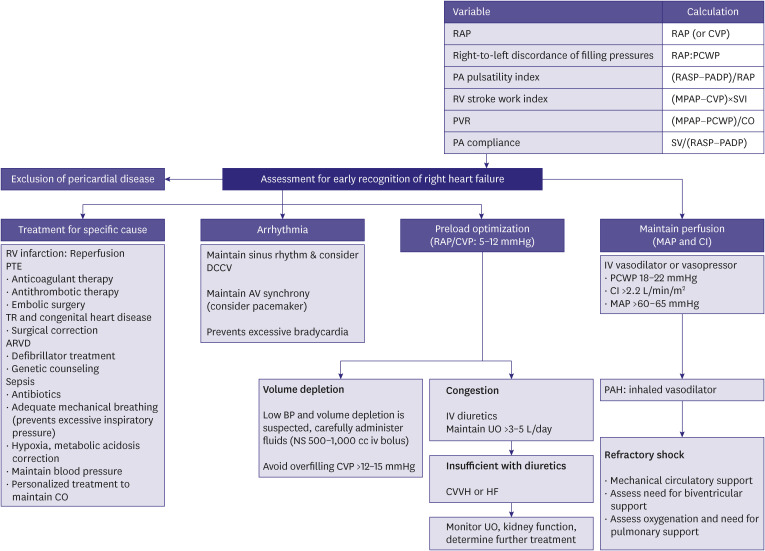
Article91. Harjola VP, Mebazaa A, Čelutkienė J, et al. Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology. Eur J Heart Fail. 2016; 18:226–241. PMID: 26995592.
Article92. Arrigo M, Huber LC, Winnik S, et al. Right ventricular failure: pathophysiology, diagnosis and treatment. Card Fail Rev. 2019; 5:140–146. PMID: 31768270.
Article93. Wever-Pinzon O, Drakos SG, Fang JC. Team-based care for advanced heart failure. Heart Fail Clin. 2015; 11:467–477. PMID: 26142642.
Article94. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995; 333:1190–1195. PMID: 7565975.
Article95. Rich MW, Gray DB, Beckham V, Wittenberg C, Luther P. Effect of a multidisciplinary intervention on medication compliance in elderly patients with congestive heart failure. Am J Med. 1996; 101:270–276. PMID: 8873488.
Article96. McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004; 44:810–819. PMID: 15312864.
Article97. Kasper EK, Gerstenblith G, Hefter G, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002; 39:471–480. PMID: 11823086.
Article98. Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005; 111:179–185. PMID: 15642765.
Article99. Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004; 291:1358–1367. PMID: 15026403.
Article100. Kim C. Overview of cardiac rehabilitation and current situations in Korea. Ann Cardiopulm Rehabil. 2021; 1:6–16.
Article101. Kim WS. Exercise-based cardiac rehabilitation in heart failure. Ann Cardiopulm Rehabil. 2021; 1:57–65.
Article102. Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015; 22:35–74. PMID: 23943649.
Article103. Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019; 140:e69–e89. PMID: 31082266.
Article104. Pedretti RF, Iliou MC, Israel CW, et al. Comprehensive multicomponent cardiac rehabilitation in cardiac implantable electronic devices recipients: a consensus document from the European Association of Preventive Cardiology (EAPC; Secondary prevention and rehabilitation section) and European Heart Rhythm Association (EHRA). Europace. 2021; 23:1336–1337o. PMID: 33636723.
Article105. Dunlay SM, Allison TG, Pereira NL. Changes in cardiopulmonary exercise testing parameters following continuous flow left ventricular assist device implantation and heart transplantation. J Card Fail. 2014; 20:548–554. PMID: 24893345.
Article106. Schmidt T, Bjarnason-Wehrens B, Predel HG, Reiss N. Exercise after heart transplantation: typical alterations, diagnostics and interventions. Int J Sports Med. 2021; 42:103–111. PMID: 32688413.
Article107. Wilhelm M, Abreu A, Adami PE, et al. EAPC core curriculum for preventive cardiology. Eur J Prev Cardiol. 2022; 29:251–274. PMID: 33791783.
Article108. Suzuki S, Yoshihisa A, Sato Y, et al. Clinical significance of get with the guidelines-heart failure risk score in patients with chronic heart failure after hospitalization. J Am Heart Assoc. 2018; 7:e008316. PMID: 30371158.
Article109. Kim IC, Youn JC, Jang SY, et al. Physician adherence and patient-reported outcomes in heart failure with reduced ejection fraction in the era of angiotensin receptor-neprilysin inhibitor therapy. Sci Rep. 2022; 12:7730. PMID: 35545653.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of cardiac imaging in management of heart failure
- Acute Heart Failure and Its Management
- Key Role of the Korean Society of Heart Failure: Moving Towards a Global and Individualized Approach
- The Korean Society of Heart Failure: Breaking Barriers, Bridging Solutions Together!
- Optimal Management of Heart Failure with Preserve Ejection Fraction