Intest Res.
2023 Apr;21(2):226-234. 10.5217/ir.2022.00010.
Interferon-gamma release assay has poor diagnostic accuracy in differentiating intestinal tuberculosis from Crohn’s disease in tuberculosis endemic areas
- Affiliations
-
- 1Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2541895
- DOI: http://doi.org/10.5217/ir.2022.00010
Abstract
- Background/Aims
Intestinal tuberculosis (ITB) and Crohn’s disease (CD) frequently present with a diagnostic dilemma because of similar presentation. Interferon-gamma release assay (IGRA) has been used in differentiating ITB from CD, but with sparse reports on its diagnostic accuracy in tuberculosis endemic regions and this study evaluated the same.
Methods
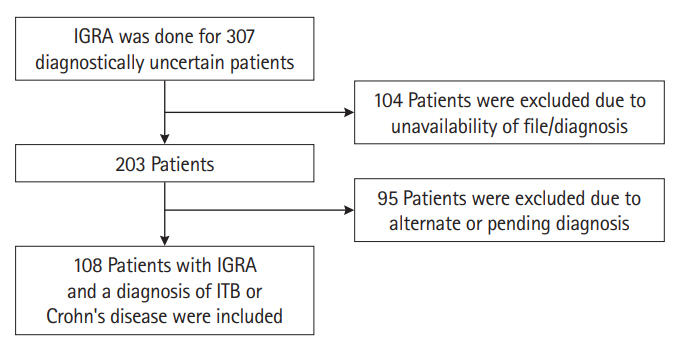
Patients with definitive diagnosis of ITB (n=59) or CD (n=49) who underwent IGRA testing (n=307) were retrospectively included at All India Institute of Medical Sciences, New Delhi (July 2014 to September 2021). CD or ITB was diagnosed as per standard criteria. IGRA was considered positive at >0.35 IU/mL. Relevant data was collected and IGRA results were compared between ITB and CD to determine its accuracy.
Results
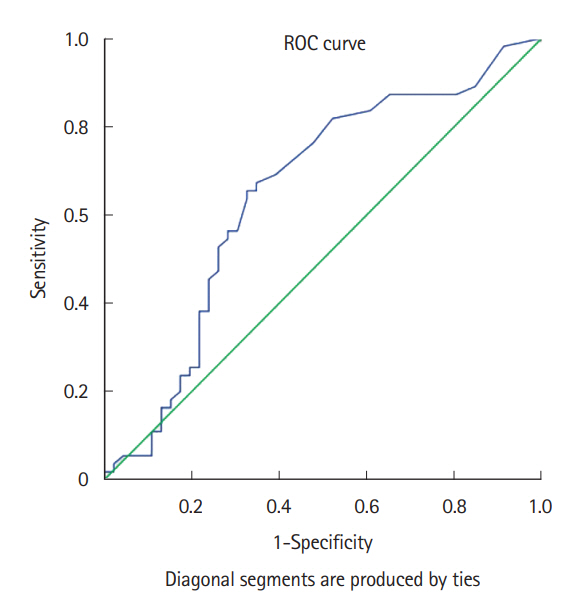
Among 59 ITB patients (mean age, 32.6±13.1 years; median disease duration, 1 year; male, 59.3%), 24 were positive and 35 tested negative for IGRA. Among 49 CD patients (mean age, 37.8±14.0; median disease duration, 4 years; male, 61.2%), 12 were positive and 37 tested negative for IGRA. Hence, for diagnosing ITB, IGRA showed a sensitivity, specificity, positive and negative predictive values of 40.68%, 75.51%, 66.67%, and 51.39%, respectively. The area under the curve of IGRA for ITB diagnosis was 0.66 (95% confidence interval, 0.55–0.75). In a subset (n=64), tuberculin skin test (TST) showed sensitivity, specificity, positive and negative predictive values of 64.7%, 73.3%, 73.3%, and 64.71%, respectively. IGRA and TST were concordant in 38 (59.4%) patients with κ=0.17.
Conclusions
In a tuberculosis endemic region, IGRA had poor diagnostic accuracy for differentiating ITB from CD, suggesting a limited value of IGRA in this setting.
Keyword
Figure
Reference
-
1. World Health Organisation. Global tuberculosis report 2020 [Internet]. c2020 [cited 2021 Nov 15]. https://www.who.int/publications/i/item/9789240013131.2. Rathi P, Gambhire P. Abdominal tuberculosis. J Assoc Physicians India. 2016; 64:38–47.3. Sharma MP, Ahuja V. Abdominal (gastrointestinal tract) tuberculosis in adult. In: Schaaf HS, Zumla AI, Grange JM, eds. Tuberculosis: a comprehensive clinical reference. Edinburgh: Saunders Elsevier,. 2009; 424–431.4. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017; 390:2769–2778.
Article5. Singh P, Ananthakrishnan A, Ahuja V. Pivot to Asia: inflammatory bowel disease burden. Intest Res. 2017; 15:138–141.
Article6. Dhoble P, Desai D, Abraham P. Is the rise in Crohn’s disease in India accompanied by a fall in intestinal tuberculosis? A single-center experience. Indian J Tuberc. 2021; 68:210–214.
Article7. Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010; 11:134–147.
Article8. Limsrivilai J, Pausawasdi N. Intestinal tuberculosis or Crohn’s disease: a review of the diagnostic models designed to differentiate between these two gastrointestinal diseases. Intest Res. 2021; 19:21–32.
Article9. Kedia S, Das P, Madhusudhan KS, et al. Differentiating Crohn’s disease from intestinal tuberculosis. World J Gastroenterol. 2019; 25:418–432.
Article10. Limsrivilai J, Shreiner AB, Pongpaibul A, et al. Meta-analytic Bayesian model for differentiating intestinal tuberculosis from Crohn’s disease. Am J Gastroenterol. 2017; 112:415–427.
Article11. Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific Consensus Statements on Crohn’s disease. Part 1: definition, diagnosis, and epidemiology: (Asia Pacific Crohn’s Disease Consensus: part 1). J Gastroenterol Hepatol. 2016; 31:45–55.
Article12. Gupta A, Pratap Mouli V, Mohta S, et al. Antitubercular therapy given to differentiate Crohn’s disease from intestinal tuberculosis predisposes to stricture formation. J Crohns Colitis. 2020; 14:1611–1618.
Article13. Pai M, Denkinger CM, Kik SV, et al. Gamma interferon release assays for detection of Mycobacterium tuberculosis infection. Clin Microbiol Rev. 2014; 27:3–20.
Article14. Sharma SK, Ryan H, Khaparde S, et al. Index-TB guidelines: guidelines on extrapulmonary tuberculosis for India. Indian J Med Res. 2017; 145:448–463.15. Ng SC, Hirai HW, Tsoi KK, et al. Systematic review with meta-analysis: accuracy of interferon-gamma releasing assay and anti-Saccharomyces cerevisiae antibody in differentiating intestinal tuberculosis from Crohn’s disease in Asians. J Gastroenterol Hepatol. 2014; 29:1664–1670.
Article16. Stange EF, Travis SP, Vermeire S, et al. European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut. 2006; 55(Suppl 1):i1–i15.
Article17. Pratap Mouli V, Munot K, Ananthakrishnan A, et al. Endoscopic and clinical responses to anti-tubercular therapy can differentiate intestinal tuberculosis from Crohn’s disease. Aliment Pharmacol Ther. 2017; 45:27–36.
Article18. Ramakrishna BS, Makharia GK, Ahuja V, et al. Indian Society of Gastroenterology consensus statements on Crohn’s disease in India. Indian J Gastroenterol. 2015; 34:3–22.
Article19. Nayak S, Acharjya B. Mantoux test and its interpretation. Indian Dermatol Online J. 2012; 3:2–6.
Article20. Fan L, Chen Z, Hao XH, Hu ZY, Xiao HP. Interferon-gamma release assays for the diagnosis of extrapulmonary tuberculosis: a systematic review and meta-analysis. FEMS Immunol Med Microbiol. 2012; 65:456–466.
Article21. Kim YJ, Kang JY, Kim SI, Chang MS, Kim YR, Park YJ. Predictors for false-negative QuantiFERON-TB Gold assay results in patients with extrapulmonary tuberculosis. BMC Infect Dis. 2018; 18:457.
Article22. Yamasue M, Komiya K, Usagawa Y, et al. Factors associated with false negative interferon-γ release assay results in patients with tuberculosis: a systematic review with meta-analysis. Sci Rep. 2020; 10:1607.
Article23. Zhao Y, Xu M, Chen L, Liu Z, Sun X. Levels of TB-IGRA may help to differentiate between intestinal tuberculosis and Crohn’s disease in patients with positive results. Therap Adv Gastroenterol. 2020; 13:1756284820922003.
Article24. Kim SH, Cho OH, Park SJ, et al. Diagnosis of abdominal tuberculosis by T-cell-based assays on peripheral blood and peritoneal fluid mononuclear cells. J Infect. 2009; 59:409–415.
Article25. Xu H, Li Y, Qian JM. A Meta-analysis of the accuracy of interferon-γ release assays in differentiating intestinal tuberculosis from Crohn’s disease in Asia. Zhonghua Nei Ke Za Zhi. 2016; 55:535–540.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of an Interferon-gamma Release Assay to Detect Active Tuberculosis in Children: A Pilot Study
- Diagnosis and treatment of latent tuberculosis infection
- The Usefulness of Whole-blood Interferon-gamma Release Assay for the Diagnosis of Extra-pulmonary Tuberculosis
- Intestinal tuberculosis or Crohn’s disease: a review of the diagnostic models designed to differentiate between these two gastrointestinal diseases
- Differentiating between Intestinal Tuberculosis and Crohn’s Disease May Be Complicated by Multidrug-resistant Mycobacterium tuberculosis