Korean J Transplant.
2023 Mar;37(1):63-68. 10.4285/kjt.22.0043.
Delayed exacerbation of COVID-19 pneumonia in vaccinated kidney transplant recipients receiving immunosuppressants: a case series
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Bong Seng Memorial Hospital, Busan, Korea
- KMID: 2541314
- DOI: http://doi.org/10.4285/kjt.22.0043
Abstract
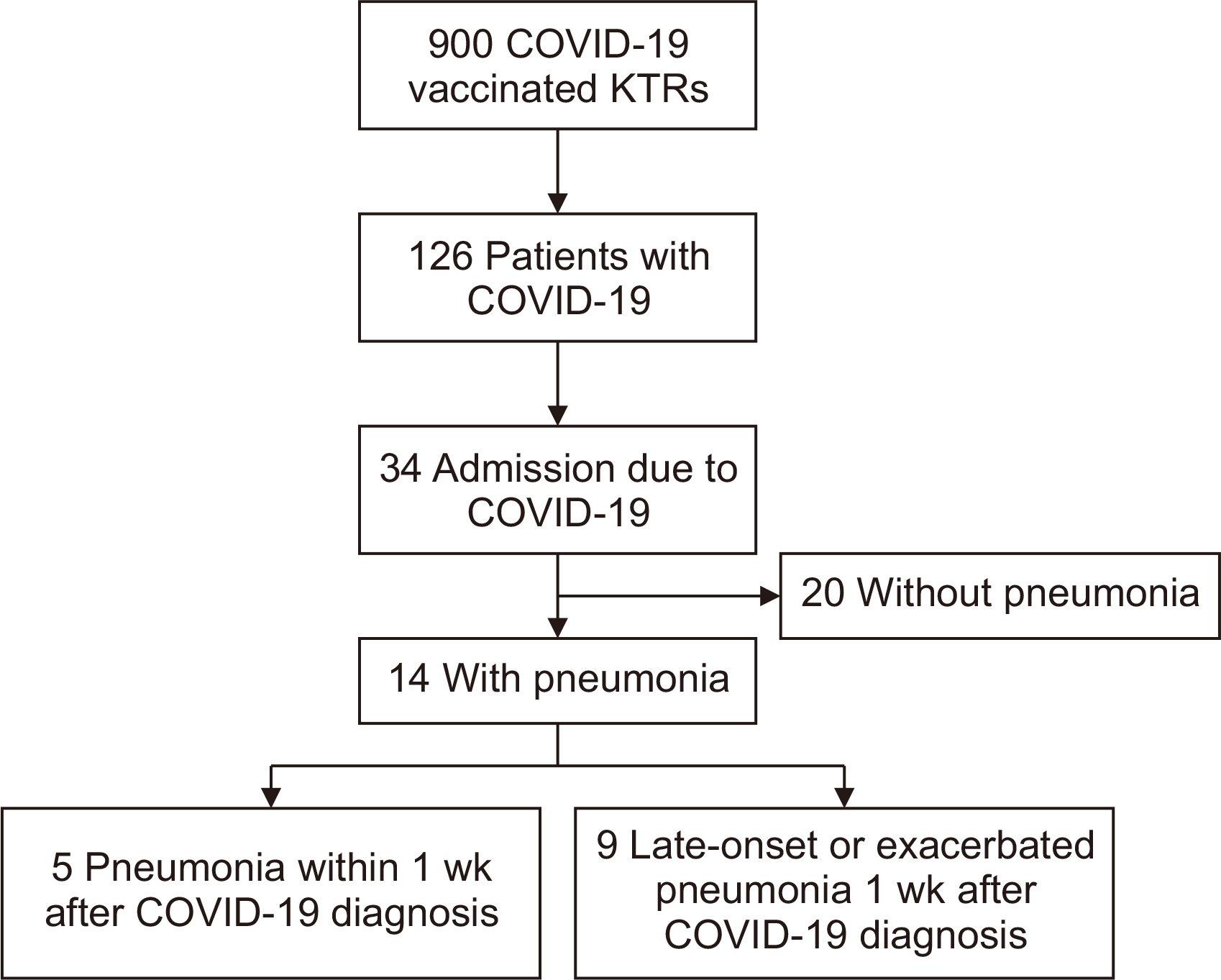
- Coronavirus disease 2019 (COVID-19) increases the risk of mortality and hospitalization in immunocompromised patients, including kidney transplant recipients (KTRs) receiving immunosuppressants. Several vaccines for COVID-19 have been developed and proven effective in decreasing the incidence of COVID-19 and the rate of progression to severe COVID-19. However, breakthrough infections have also been reported in vaccinated patients. We report cases from our center of delayed exacerbated pneumonia from COVID-19 in vaccinated KTRs receiving immunosuppressants. Of the 900 KTRs who had been vaccinated for COVID-19 and were followed up at our center from January 1, 2022, to April 30, 2022 (during the Omicron variant outbreak), 126 contracted COVID-19 (incidence rate, 14%). Thirty-four (27%) in this group were hospitalized due to COVID-19. Twenty patients did not have pneumonia but had symptoms of upper respiratory tract infection or diarrhea, which improved with conservative treatment. Nine of the 14 patients with pneumonia had delayed onset or exacerbated pneumonia 1 week after their COVID-19 diagnosis. They were treated with remdesivir, and most recovered. One patient died due to progressive pneumonia and pneumothorax. It is important that KTRs who are taking immunosuppressants be observed closely and for a prolonged period after a COVID-19 diagnosis, irrespective of their COVID-19 vaccination status.
Keyword
Figure
Cited by 1 articles
-
Tixagevimab/cilgavimab prophylaxis against COVID-19 in solid organ transplant recipients: a systematic review and meta-analysis
Saeed Khorramnia, Zia Navidi, Amirhossein Orandi, Mojgan Mohajeri Iravani, Amirali Orandi, Ebadallah Shiri Malekabad, Seyed Hamid Pakzad Moghadam
Clin Transplant Res. 2024;38(2):136-144. doi: 10.4285/ctr.24.0015.
Reference
-
1. Dai CL, Kornilov SA, Roper RT, Cohen-Cline H, Jade K, Smith B, et al. 2021; Characteristics and factors associated with coronavirus disease 2019 infection, hospitalization, and mortality across race and ethnicity. Clin Infect Dis. 73:2193–204. DOI: 10.1093/cid/ciab154. PMID: 33608710. PMCID: PMC7929051.2. Li J, Huang DQ, Zou B, Yang H, Hui WZ, Rui F, et al. 2021; Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 93:1449–58. DOI: 10.1002/jmv.26424. PMID: 32790106. PMCID: PMC7436673.
Article3. Zhang YJ, Sun XF, Xie B, Feng WJ, Han SL. 2021; Exploration of severe Covid-19 associated risk factor in China: meta-analysis of current evidence. Int J Clin Pract. 75:e14900. DOI: 10.1111/ijcp.14900. PMCID: PMC8646532.
Article4. Kates OS, Haydel BM, Florman SS, Rana MM, Chaudhry ZS, Ramesh MS, et al. 2021; Coronavirus disease 2019 in solid organ transplant: a multicenter cohort study. Clin Infect Dis. 73:e4090–9.5. Kang JM, Kim YJ, Huh K, Kim JM, Park WB, Ahn HJ, et al. 2022; COVID-19 among solid organ transplant recipients in Korea: surveillance data of the Korean Transplantation Society, January 2020 to March 2022. Korean J Transplant. 36:159–63. DOI: 10.4285/kjt.22.0025. PMID: 35919200. PMCID: PMC9296979.6. Akalin E, Azzi Y, Bartash R, Seethamraju H, Parides M, Hemmige V, et al. 2020; Covid-19 and kidney transplantation. N Engl J Med. 382:2475–7. DOI: 10.1056/NEJMc2011117. PMID: 32329975. PMCID: PMC7200055.7. Kee T, Jeong JC, Ur-Rashid H, Begum NA, Arakama MH, Danguilan R, et al. 2021; Clinical characteristics, outcomes, and management of COVID-19 in kidney transplant recipients across Asia: an ASTREGO report. Korean J Transplant. 35:218–29. DOI: 10.4285/kjt.21.0024. PMID: 35769859. PMCID: PMC9235460.
Article8. Monfared A, Akhondzadeh L, Mousazadeh M, Jafari A, Khosravi M, Lebadi M, et al. 2021; COVID-19 in renal transplant recipients and general population: a comparative study of clinical, laboratory, and radiological features, severity, and outcome. Virol J. 18:243. DOI: 10.1186/s12985-021-01713-x. PMID: 34876176. PMCID: PMC8649678.9. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. 2021; A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 27:225–8. DOI: 10.1038/s41591-020-1124-9. PMID: 33082575. PMCID: PMC7573523.10. Asghar MS, Khan MT, Hamid RB, Lal N, Ahmed I, Hameed B, et al. 2021; Clinical characteristics, biochemical markers, and outcomes of postrenal transplant patients with coronavirus diseases 2019: a single-center experience. Saudi J Kidney Dis Transpl. 32:1689–99. DOI: 10.4103/1319-2442.352430. PMID: 35946282.11. Saberian P, Pazooki B, Hasani-Sharamin P, Garjani K, Ahmadi Hatam Z, Dadashi F, et al. 2022; Persistent/late-onset complications of COVID-19 in general population: a cross-sectional study in Tehran, Iran. Int J Community Based Nurs Midwifery. 10:234–45.12. Herman B, Wong MC, Viwattanakulvanid P. 2022; Vaccination status, favipiravir, and micronutrient supplementation roles in post-COVID symptoms: a longitudinal study. PLoS One. 17:e0271385. DOI: 10.1371/journal.pone.0271385. PMID: 35862378. PMCID: PMC9302723.
Article13. Ayhancı T, Toptan H, Özer YE, Uzar S, Enül H, Adıay C, et al. 2022; Shedding of SARS-CoV-2 virus in COVID-19 patients and neutralizing antibody level. Mikrobiyol Bul. 56:416–31. DOI: 10.5578/mb.20229704. PMID: 35960235.14. Jozwik A, Habibi MS, Paras A, Zhu J, Guvenel A, Dhariwal J, et al. 2015; RSV-specific airway resident memory CD8+ T cells and differential disease severity after experimental human infection. Nat Commun. 6:10224. DOI: 10.1038/ncomms10224. PMID: 26687547. PMCID: PMC4703893.15. Quéméneur L, Beloeil L, Michallet MC, Angelov G, Tomkowiak M, Revillard JP, et al. 2004; Restriction of de novo nucleotide biosynthesis interferes with clonal expansion and differentiation into effector and memory CD8 T cells. J Immunol. 173:4945–52. DOI: 10.4049/jimmunol.173.8.4945. PMID: 15470036.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical manifestations of delayed COVID-19 pneumonia in kidney transplant recipients
- Managing COVID-19 infection in living donation kidney transplant recipient: a single center experience
- Association of COVID-19 vaccination and COVID-19 infection risk in heart transplantation recipients
- Outcomes of COVID-19 in Thai kidney transplant recipients in the vaccination era
- Single center experience of COVID-19 management among kidney transplant recipient in Omicron pandemic