Cancer Res Treat.
2023 Apr;55(2):562-569. 10.4143/crt.2022.871.
Retrospective Cohort Study on the Long-term Oncologic Outcomes of Sentinel Lymph Node Mapping Methods (Dye-Only versus Dye and Radioisotope Mapping) in Early Breast Cancer: A Propensity Score-Matched Analysis
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 3Cancer Research Institute, Seoul National University, Seoul, Korea
- KMID: 2541243
- DOI: http://doi.org/10.4143/crt.2022.871
Abstract
- Purpose
In sentinel lymph node (SLN) biopsy (SLNB) during breast cancer surgery, SLN mapping using dye and isotope (DUAL) may have lower false-negative rates than the dye-only (DYE) method. However, the long-term outcomes of either method are unclear. We aimed to compare long-term oncological outcomes of DYE and DUAL for SLNB in early breast cancer.
Materials and Methods
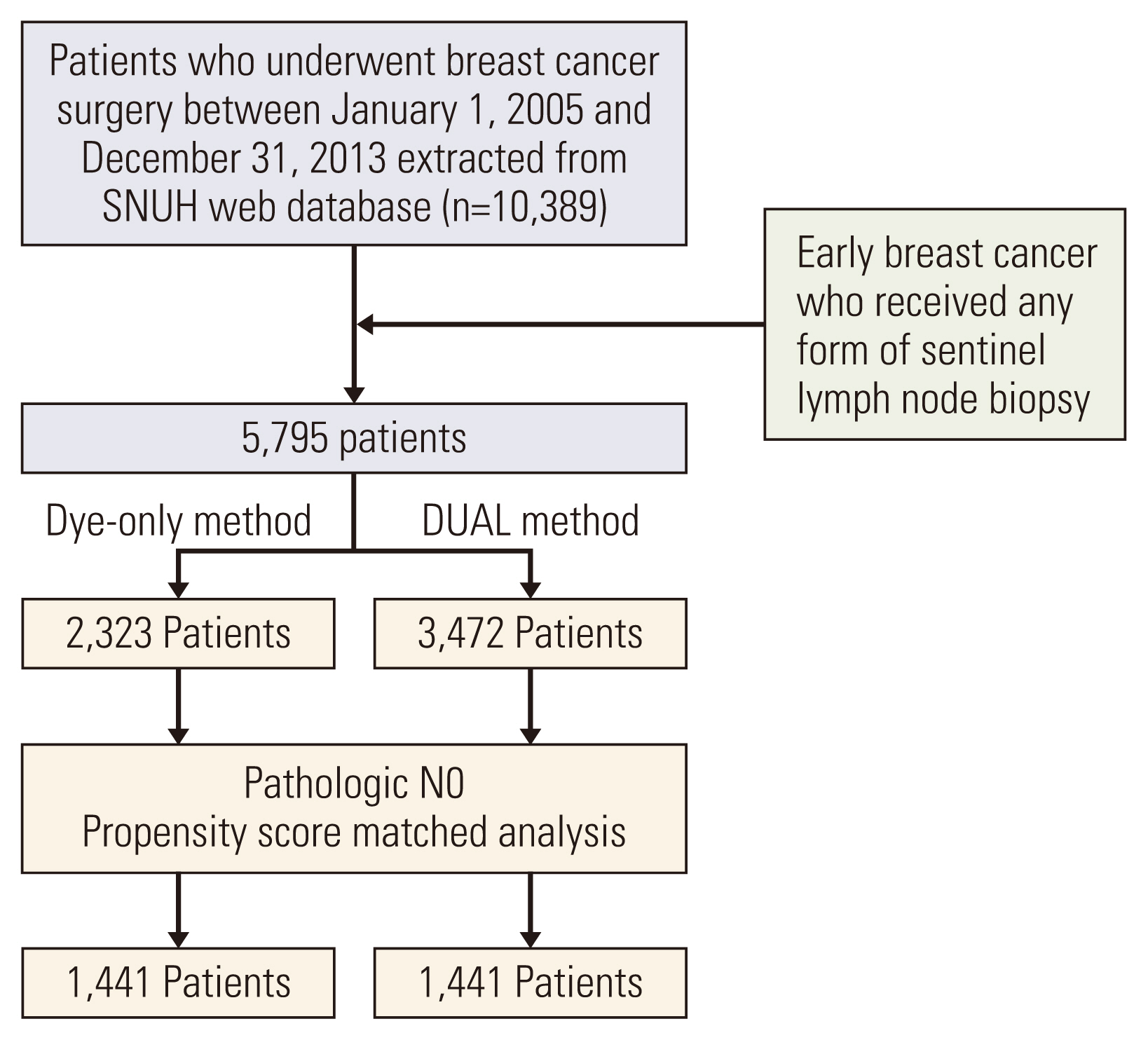
This retrospective single-institution cohort study included 5,795 patients (DYE, 2,323; DUAL, 3,472) with clinically node-negative breast cancer who underwent SLNB and no neoadjuvant therapy. Indigo carmine was used for the dye method and Tc99m-antimony trisulfate for the isotope. To compare long-term outcomes, pathologic N0 patients were selected from both groups, and propensity score matching (PSM), considering age, pT category, breast surgery, and adjuvant treatment, was performed (1,441 patients in each group).
Results
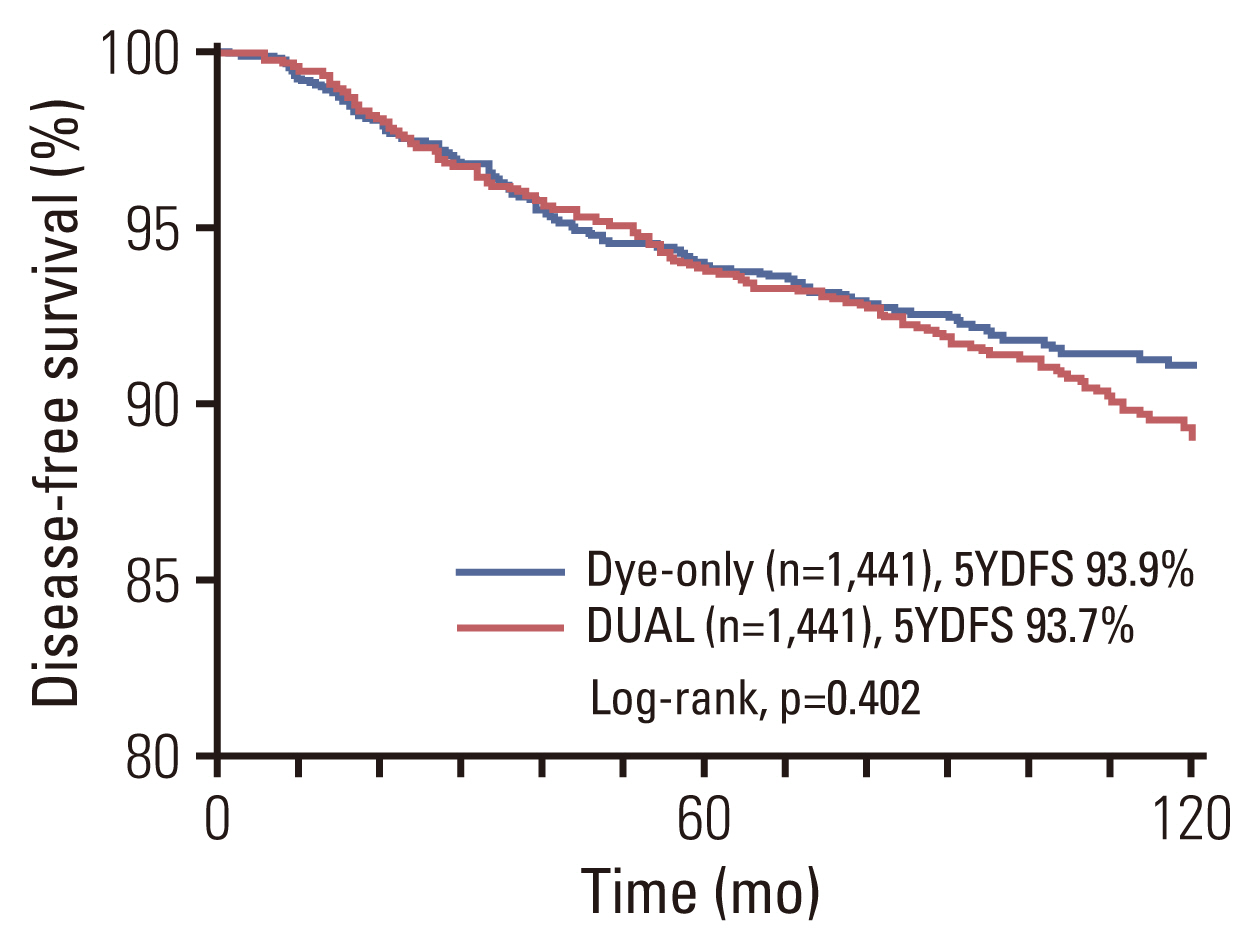
The median follow-up duration was 8.7 years. The median number of harvested sentinel nodes was 3.21 and 3.12 in the DYE and DUAL groups, respectively (p=0.112). The lymph node–positive rate was not significantly different between the two groups in subgroups of similar tumor sizes (p > 0.05). Multivariate logistic regression revealed that the mapping method was not significantly associated with the lymph node–positive rate (p=0.758). After PSM, the 5-year axillary recurrence rate (DYE 0.8% vs. DUAL 0.6%, p=0.096), and 5-year disease-free survival (DYE 93.9% vs. DUAL 93.7%, p=0.402) were similar between the two groups.
Conclusion
Dye alone for SLNB was not inferior to dual mapping regarding long-term oncological outcomes in early breast cancer.
Keyword
Figure
Reference
-
References
1. Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994; 220:391–8.
Article2. Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010; 11:927–33.
Article3. Li J, Chen X, Qi M, Li Y. Sentinel lymph node biopsy mapped with methylene blue dye alone in patients with breast cancer: a systematic review and meta-analysis. PLoS One. 2018; 13:e0204364.
Article4. Syme DB, Collins JP, Mann GB. Comparison of blue dye and isotope with blue dye alone in breast sentinel node biopsy. ANZ J Surg. 2005; 75:817–21.
Article5. Radovanovic Z, Golubovic A, Plzak A, Stojiljkovic B, Radovanovic D. Blue dye versus combined blue dye-radioactive tracer technique in detection of sentinel lymph node in breast cancer. Eur J Surg Oncol. 2004; 30:913–7.
Article6. Motomura K, Inaji H, Komoike Y, Hasegawa Y, Kasugai T, Noguchi S, et al. Combination technique is superior to dye alone in identification of the sentinel node in breast cancer patients. J Surg Oncol. 2001; 76:95–9.
Article7. Pesek S, Ashikaga T, Krag LE, Krag D. The false-negative rate of sentinel node biopsy in patients with breast cancer: a meta-analysis. World J Surg. 2012; 36:2239–51.
Article8. Ahmed M, Purushotham AD, Douek M. Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol. 2014; 15:e351–62.
Article9. Aihara T, Takatsuka Y. Dye-guided sentinel node biopsy revi-sited; validation and observational study from a single institute. Breast Cancer. 2003; 10:254–9.
Article10. He PS, Li F, Li GH, Guo C, Chen TJ. The combination of blue dye and radioisotope versus radioisotope alone during sentinel lymph node biopsy for breast cancer: a systematic review. BMC Cancer. 2016; 16:107.
Article11. Cody HS 3rd, Fey J, Akhurst T, Fazzari M, Mazumdar M, Yeung H, et al. Complementarity of blue dye and isotope in sentinel node localization for breast cancer: univariate and multivariate analysis of 966 procedures. Ann Surg Oncol. 2001; 8:13–9.
Article12. Lyman GH, Giuliano AE, Somerfield MR, Benson AB 3rd, Bodurka DC, Burstein HJ, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005; 23:7703–20.
Article13. Gentilini O, Cremonesi M, Trifiro G, Ferrari M, Baio SM, Cara-cciolo M, et al. Safety of sentinel node biopsy in pregnant patients with breast cancer. Ann Oncol. 2004; 15:1348–51.
Article14. Krynyckyi BR, Miner M, Ragonese JM, Firestone M, Kim CK, Machac J. Technical aspects of performing lymphoscintigraphy: optimization of methods used to obtain images. Clin Nucl Med. 2000; 25:978–85.15. Golshan M, Nakhlis F. Can methylene blue only be used in sentinel lymph node biopsy for breast cancer? Breast J. 2006; 12:428–30.
Article16. Bundred NJ, Barnes NL, Rutgers E, Donker M. Is axillary lymph node clearance required in node-positive breast cancer? Nat Rev Clin Oncol. 2015; 12:55–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Peritumoral and Subareolar Injection of Blue Dye Improves Sentinel Lymph Node Localization Rates
- Surgical technique of two-step pelvic and para-aortic sentinel lymph node mapping in early-stage endometrial cancer: laparoscopic, robotic, and open method
- A Case of Anaphylactic Reactions to Isosulfan Blue Dye in A Cervical Cancer Patient
- Combined Peritumoral and Subareolar Injection of Blue Dye Improves Sentinel Lymph Node Localization Rates
- Decrease in Pulse Oximeter Readings Following Injection of Isosulfan Blue Dye