J Rheum Dis.
2023 Apr;30(2):133-137. 10.4078/jrd.22.0054.
The SLC29A3 variant, neutrophilic dermatosis, and hyperferritinemia imitate systemic juvenile idiopathic arthritis in a Saudi child: a case report
- Affiliations
-
- 1Department of Pediatric Rheumatology, Saudi Arabia
- 2Department of Pathology and Laboratory Medicine, King Faisal Specialist Hospital and Research Center, Saudi Arabia
- 3Department of Pediatrics, College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
- KMID: 2541057
- DOI: http://doi.org/10.4078/jrd.22.0054
Abstract
- Genetic defects of SLC29A3 result in a wide range of syndromic histiocytosis that encompasses H syndrome. Patients with SLC29A3 variants typically have hyperpigmentation, hypertrichosis, hepatosplenomegaly, sensorineural hearing loss, diabetes mellitus, and hypogonadism. Herein, we identify a novel phenotype in a girl presenting with clinical and laboratory findings similar to systemic juvenile arthritis and hyperferritinemia. Exome sequencing identified a homozygous variant in SLC29A3 (NM_018344.5: c.707C>T [p.T236M]). Our patient did not show the cardinal features of the broad spectrum of SLC29A3-related disorders. She demonstrated remarkable improvement in her clinical and laboratory manifestations after starting interleukin-1 blockade (Anakinra). Recent research suggests that SLC29A3-related disorders are accompanied with autoinflammation and autoimmunity due to an overactive inflammasome pathway, which is most likely induced by mitochondrial and lysosomal dysfunction. Hence, our findings may expand the phenotypic features of the SLC29A3 variant. Patients with the SLC29A3 variant and systemic inflammation may benefit from interleukin-1 blockade as a therapeutic option.
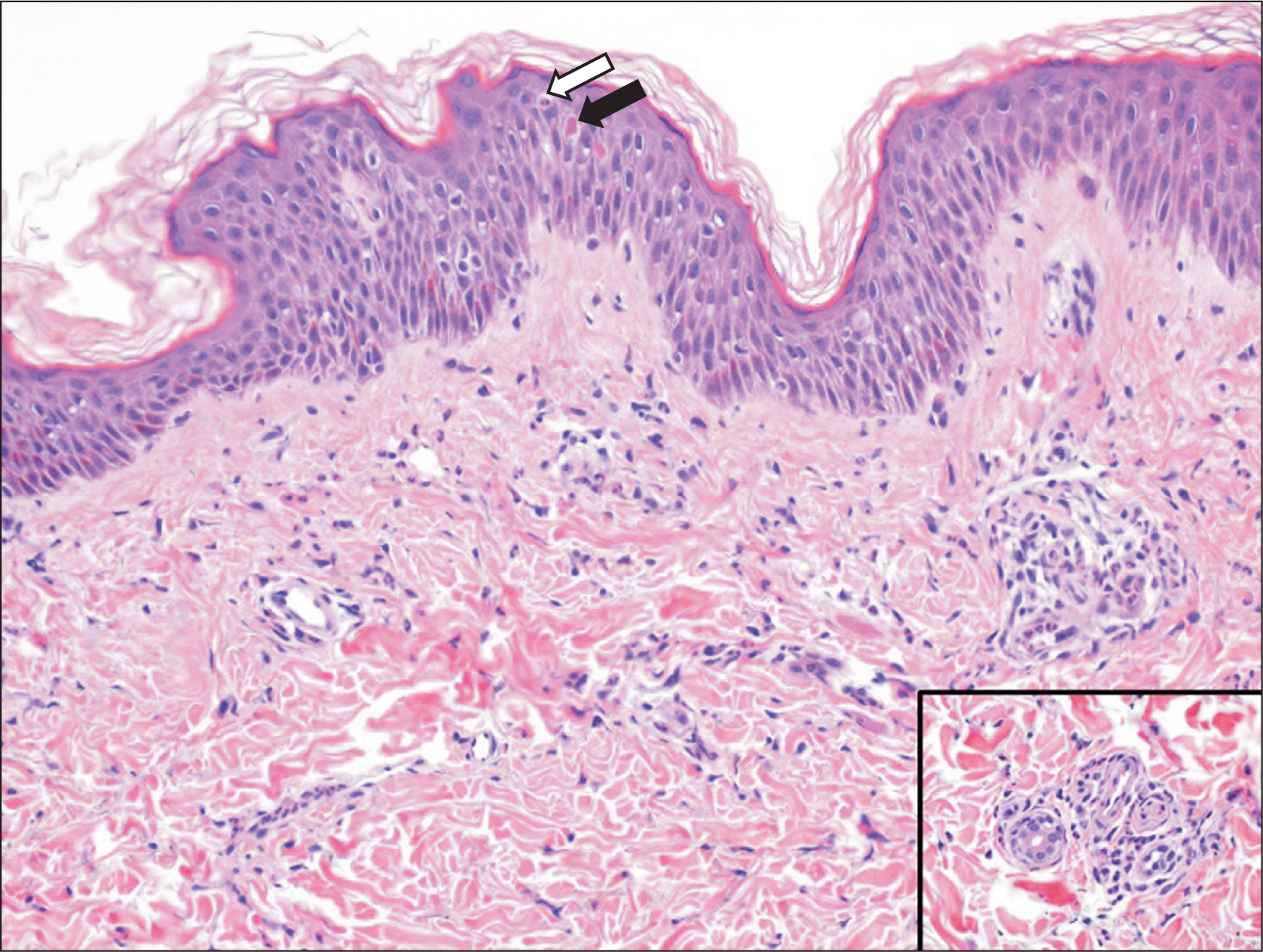
Figure
Reference
-
1. Chouk H, Ben Rejeb M, Boussofara L, Elmabrouk H, Ghariani N, Sriha B, et al. 2021; Phenotypic intrafamilial variability including H syndrome and Rosai-Dorfman disease associated with the same c.1088G > A mutation in the SLC29A3 gene. Hum Genomics. 15:63. DOI: 10.1186/s40246-021-00362-z. PMID: 34657628. PMCID: PMC8522101.2. Molho-Pessach V, Ramot Y, Camille F, Doviner V, Babay S, Luis SJ, et al. 2014; H syndrome: the first 79 patients. J Am Acad Dermatol. 70:80–8. DOI: 10.1016/j.jaad.2013.09.019. PMID: 24172204.
Article3. Morgan NV, Morris MR, Cangul H, Gleeson D, Straatman-Iwanowska A, Davies N, et al. 2010; Mutations in SLC29A3, encoding an equilibrative nucleoside transporter ENT3, cause a familial histiocytosis syndrome (Faisalabad histiocytosis) and familial Rosai-Dorfman disease. PLoS Genet. 6:e1000833. DOI: 10.1371/journal.pgen.1000833. PMID: 20140240. PMCID: PMC2816679.
Article4. Jaouadi H, Zaouak A, Sellami K, Messaoud O, Chargui M, Hammami H, et al. 2018; H syndrome: clinical, histological and genetic investigation in Tunisian patients. J Dermatol. 45:978–85. DOI: 10.1111/1346-8138.14359. PMID: 29808591.
Article5. Bloom JL, Lin C, Imundo L, Guthery S, Stepenaskie S, Galambos C, et al. 2017; H syndrome: 5 new cases from the United States with novel features and responses to therapy. Pediatr Rheumatol Online J. 15:76. DOI: 10.1186/s12969-017-0204-y. PMID: 29041934. PMCID: PMC5645937.
Article6. Nofal H, AlAkad R, Nofal A, Rabie E, Chaikul T, Chiu FP, et al. 2021; H syndrome: a review of treatment options and a hypothesis of phenotypic variability. Dermatol Ther. 34:e15082. DOI: 10.1111/dth.15082. PMID: 34351669.7. David O, Geylis M, Kristal E, Ling G, Schreiber R. 2021; Glomerular involvement in children with H syndrome. Pediatr Nephrol. 36:721–4. DOI: 10.1007/s00467-020-04860-5. PMID: 33387019.
Article8. Melki I, Lambot K, Jonard L, Couloigner V, Quartier P, Neven B, et al. 2013; Mutation in the SLC29A3 gene: a new cause of a monogenic, autoinflammatory condition. Pediatrics. 131:e1308–13. DOI: 10.1542/peds.2012-2255. PMID: 23530176.9. Çağdaş D, Sürücü N, Tan Ç, Kayaoğlu B, Özgül RK, Akkaya-Ulum YZ, et al. 2020; Autoinflammation in addition to combined immunodeficiency: SLC29A3 gene defect. Mol Immunol. 121:28–37. DOI: 10.1016/j.molimm.2020.02.014. PMID: 32151906.
Article10. Spiegel R, Cliffe ST, Buckley MF, Crow YJ, Urquhart J, Horovitz Y, et al. 2010; Expanding the clinical spectrum of SLC29A3 gene defects. Eur J Med Genet. 53:309–13. DOI: 10.1016/j.ejmg.2010.06.012. PMID: 20619369.
Article11. de Jesus J, Imane Z, Senée V, Romero S, Guillausseau PJ, Balafrej A, et al. 2013; SLC29A3 mutation in a patient with syndromic diabetes with features of pigmented hypertrichotic dermatosis with insulin-dependent diabetes, H syndrome and Faisalabad histiocytosis. Diabetes Metab. 39:281–5. DOI: 10.1016/j.diabet.2013.03.007. PMID: 23623699.
Article12. Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. 2004; International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 31:390–2.13. Bolze A, Abhyankar A, Grant AV, Patel B, Yadav R, Byun M, et al. 2012; A mild form of SLC29A3 disorder: a frameshift deletion leads to the paradoxical translation of an otherwise noncoding mRNA splice variant. PLoS One. 7:e29708. DOI: 10.1371/journal.pone.0029708. PMID: 22238637. PMCID: PMC3251605.
Article14. Rafiq NK, Hussain K, Brogan PA. 2017; Tocilizumab for the treatment of SLC29A3 mutation positive PHID syndrome. Pediatrics. 140:e20163148. DOI: 10.1542/peds.2016-3148. PMID: 29079714.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adult-Onset Still’s Disease with Atypical Persistent Rash and Histologic Findings of Neutrophilic Urticarial Dermatosis
- A Case of Neutrophilic Dermatosis of the Dorsal Hands with Concomitant Involvement of the Lips
- A Case of Neutrophilic Dermatosis of the Hands on Both Palms
- Neutrophilic Dermatosis of Dorsal Hands with Concomitant Involvement of the Ankle
- Renal involvement in pediatric rheumatologic diseases