Korean J Gastroenterol.
2023 Mar;81(3):129-132. 10.4166/kjg.2022.128.
Primary Duodenal Mucosa-associated Lymphoid Tissue Lymphoma Treated with Radiation Therapy Alone
- Affiliations
-
- 1Departments of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- 2Departments of Pathology, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2540956
- DOI: http://doi.org/10.4166/kjg.2022.128
Abstract
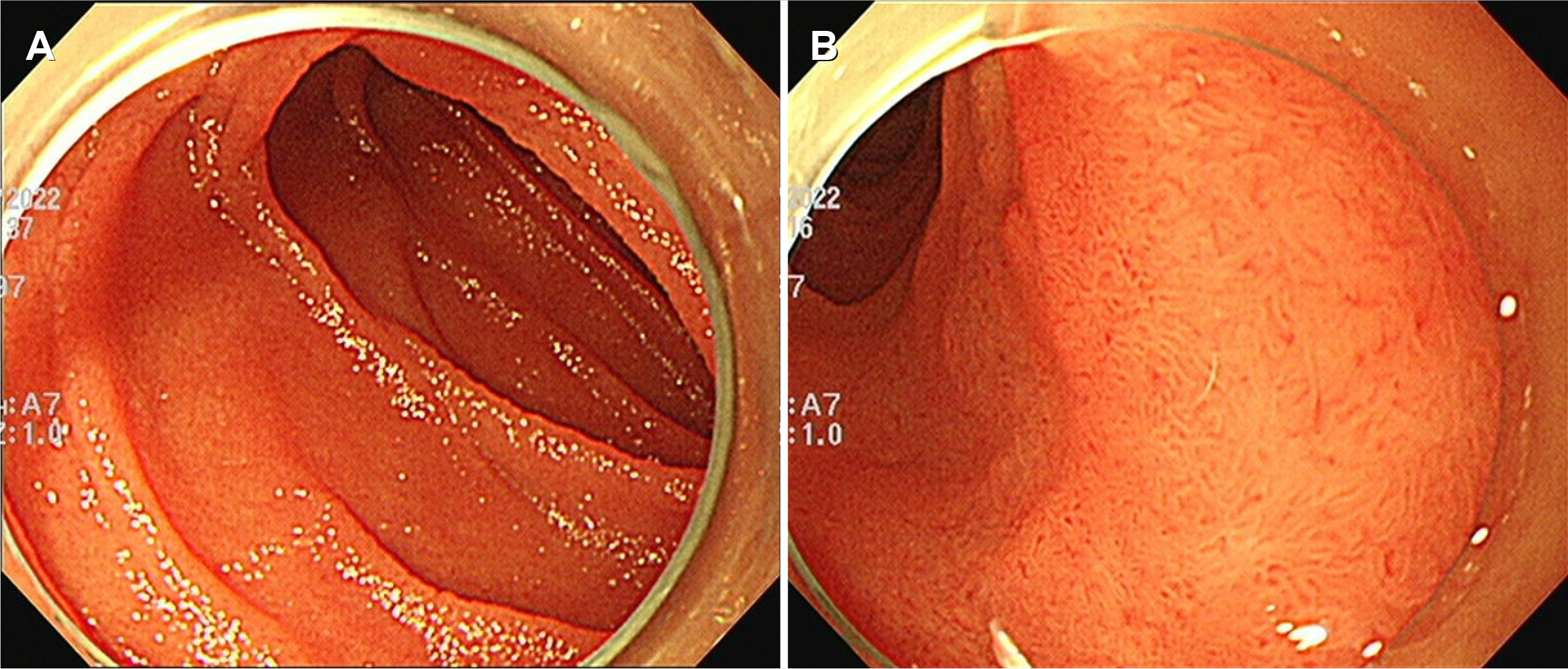
- Primary mucosa-associated with a lymphoid tissue (MALT) lymphoma is a rare distinct subtype of non-Hodgkin’s lymphoma that occurs in approximately 8% of all non-Hodgkin lymphomas. Primary gastrointestinal MALT lymphoma usually occurs in the stomach, but duodenal involvement is extremely rare. Therefore, the clinical manifestations, treatment, and prognosis of primary duodenal MALT lymphoma have not yet been validated because of its rarity. This paper reports a case of a 40-year-old male with primary duodenal MALT lymphoma who was treated successfully with radiation therapy alone. A 40-year-old male visited for a medical check-up. Esophagogastroduodenoscopy revealed whitish multi-nodular mucosal lesions in the second and third portions of the duodenum. Biopsy specimens from mucosal lesions in the duodenum were reported to be suspicious for MALT lymphoma of the duodenum. He received a total dose of 3,000 cGy in 15 fractions with external beam radiation therapy for three weeks. Three months after radiation therapy, an endoscopic examination revealed complete resolution of the duodenal lesions. The follow-up 12 months after radiation therapy showed no evidence of tumor recurrence.
Figure
Reference
-
1. Foukas PG, Bisig B, de Leval L. 2021; Recent advances upper gastrointestinal lymphomas: molecular updates and diagnostic implications. Histopathology. 78:187–214. DOI: 10.1111/his.14289. PMID: 33382495.2. Shirwaikar Thomas A, Schwartz M, Quigley E. 2019; Gastrointestinal lymphoma: the new mimic. BMJ Open Gastroenterol. 6:e000320. DOI: 10.1136/bmjgast-2019-000320. PMID: 31645987. PMCID: PMC6782046.3. Olszewska-Szopa M, Wróbel T. 2019; Gastrointestinal non-Hodgkin lymphomas. Adv Clin Exp Med. 28:1119–1124. DOI: 10.17219/acem/94068. PMID: 31414733.4. Di Rocco A, Petrucci L, Assanto GM, Martelli M, Pulsoni A. 2022; Extranodal marginal zone lymphoma: pathogenesis, diagnosis and treatment. Cancers (Basel). 14:1742. DOI: 10.3390/cancers14071742. PMID: 35406516. PMCID: PMC8997163.5. Rodríguez-Sevilla JJ, Salar A. 2021; Recent advances in the genetic of MALT lymphomas. Cancers (Basel). 14:176. DOI: 10.3390/cancers14010176. PMID: 35008340. PMCID: PMC8750177.6. Violeta Filip P, Cuciureanu D, Sorina Diaconu L, Maria Vladareanu A, Silvia Pop C. 2018; MALT lymphoma: epidemiology, clinical diagnosis and treatment. J Med Life. 11:187–193. DOI: 10.25122/jml-2018-0035. PMID: 30364585. PMCID: PMC6197515.7. Thieblemont C, Zucca E. 2017; Clinical aspects and therapy of gastrointestinal MALT lymphoma. Best Pract Res Clin Haematol. 30:109–117. DOI: 10.1016/j.beha.2017.01.002. PMID: 28288705.8. Ishikawa E, Nakamura M, Satou A, Shimada K, Nakamura S. 2022; Mucosa-associated lymphoid tissue (MALT) lymphoma in the gastrointestinal tract in the modern era. Cancers (Basel). 14:446. DOI: 10.3390/cancers14020446. PMID: 35053607. PMCID: PMC8773811.9. Carman R, Snyder J, Davidson M. 2011; Primary mucosa-associated lymphoid tumor lymphoma of the duodenum: a rare presentation of non-Hodgkin's lymphoma. J Clin Oncol. 29:e226–229. DOI: 10.1200/JCO.2010.31.9525. PMID: 21205760.10. Na HK, Won SH, Ahn JY, et al. 2021; Clinical course of duodenal mucosa-associated lymphoid tissue lymphoma: Comparison with gastric mucosa-associated lymphoid tissue lymphoma. J Gastroenterol Hepatol. 36:406–412. DOI: 10.1111/jgh.15157. PMID: 32573049.11. Ochi M, Tominaga K, Okazaki H, et al. 2006; Regression of primary low-grade mucosa-associated lymphoid tissue lymphoma of duodenum after long-term treatment with clarithromycin. Scand J Gastroenterol. 41:365–369. DOI: 10.1080/00365520500331224. PMID: 16497629.12. Nagashima R, Takeda H, Maeda K, Ohno S, Takahashi T. 1996; Regression of duodenal mucosa-associated lymphoid tissue lymphoma after eradication of Helicobacter pylori. Gastroenterology. 111:1674–1678. DOI: 10.1016/S0016-5085(96)70032-X. PMID: 8942749.13. Kamura M, Matsui K, Kokubo Y, et al. 2000; [A case of the mucosa-associated lymphoid tissue lymphoma in the duodenal bulb improved rapidly by eradication of Helicobacter pylori for 4-years]. Gastroenterol Endosc. 42:164–168. Japanese.14. Nakamura S, Matsumoto T, Nakamura S, et al. 2001; Duodenal mucosa-associated lymphoid tissue lymphoma treated by eradication of Helicobacter pylori: report of 2 cases including EUS findings. Gastrointest Endosc. 54:772–775. DOI: 10.1067/mge.2001.119602. PMID: 11726860.15. Woo KH, Kim JH, Yoon SB, et al. 2007; Duodenal mucosa-associated lymphoid tissue lymphoma: a case report. Korean J Intern Med. 22:296–299. DOI: 10.3904/kjim.2007.22.4.296. PMID: 18309692. PMCID: PMC2687664.16. Xiang Z, Onoda N, Ohira M, et al. 2004; Mucosa-associated lymphoid tissue lymphoma of the duodenum: report of a case resistant to Helicobacter pylori eradication. Hepatogastroenterology. 51:732–735.17. Wu Y, Liu X, Imber BS, et al. 2022; Influence of age on long-term net survival benefit for early-stage MALT lymphomas treated with radiotherapy: A SEER database analysis (2000-2015). Radiother Oncol. 173:179–187. DOI: 10.1016/j.radonc.2022.05.034. PMID: 35667572.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mucosa-associated Lymphoid Tissue Lymphoma Presenting with Bowel Obstruction of the Duodenum and Small Bowels: A Case Report
- Colonic Mucosa-associated Lymphoid Tissue Lymphoma Treated by Radiation Therapy: Report of a Case and Literature Review
- Duodenal Mucosa-associated Lymphoid Tissue Lymphoma Treated with Chemotherapy
- Longlasting Remission of Primary Hepatic Mucosa-associated Lymphoid Tissue (MALT) Lymphoma Achieved by Radiotherapy Alone
- A Case of Simultaneous Primary Gastric and Duodenal Mucosa-Associated Lymphoid Tissue Lymphoma after Therapeutic Endoscopy