J Cerebrovasc Endovasc Neurosurg.
2023 Mar;25(1):36-49. 10.7461/jcen.2023.E2022.06.003.
Clinical and anatomic description of patients with arteriovenous malformation treated with endovascular therapy in a Mexican population
- Affiliations
-
- 1Neurological Endovascular Therapy Department, National Neurology and Neurosurgery Institute “Dr. Manuel Velasco Suárez”, Tlalpan, Mexico City, Mexico
- 2Department of Geriatrics, North Central Hospital (PEMEX), Azcapotzalco, Mexico City, Mexico
- 3Department of Surgical Pathology, The American British Cowdray Medical Center, Cuajimalpa, Mexico City, Mexico
- 4Department of Neurosurgery, South Central High Specialty Hospital (PEMEX), Tlalpan, Mexico City, Mexico
- 5Research Department, Autonomous Tamaulipas University, Medicine Faculty of Tampico “Dr. Alberto Romo Caballero”, Tampico, Tamaulipas, Mexico
- KMID: 2540806
- DOI: http://doi.org/10.7461/jcen.2023.E2022.06.003
Abstract
Objective
Arteriovenous malformations (AVMs) are benign congenital lesions. The estimated prevalence is 10-18 per 100,000 individuals, with an incidence rate of 1.1-1.4 per 100,000 person-year; only 12% of AVMs present symptoms during life. It is important to study different characteristics associated with AVMs because these patients require multidisciplinary treatment.
Methods
A descriptive, observational, longitudinal, and retrospective study was carried out from January 15, 2016 to October 19, 2021. Convenience sampling was used on patients diagnosed with arteriovenous malformation. Sociodemographic data was obtained, such as: sex, age, site, predominant symptoms, clinical debut, type of malformation, data associated with post therapy evolution, type of embolizing agent used, associated complications, Rankin scale, and death.
Results
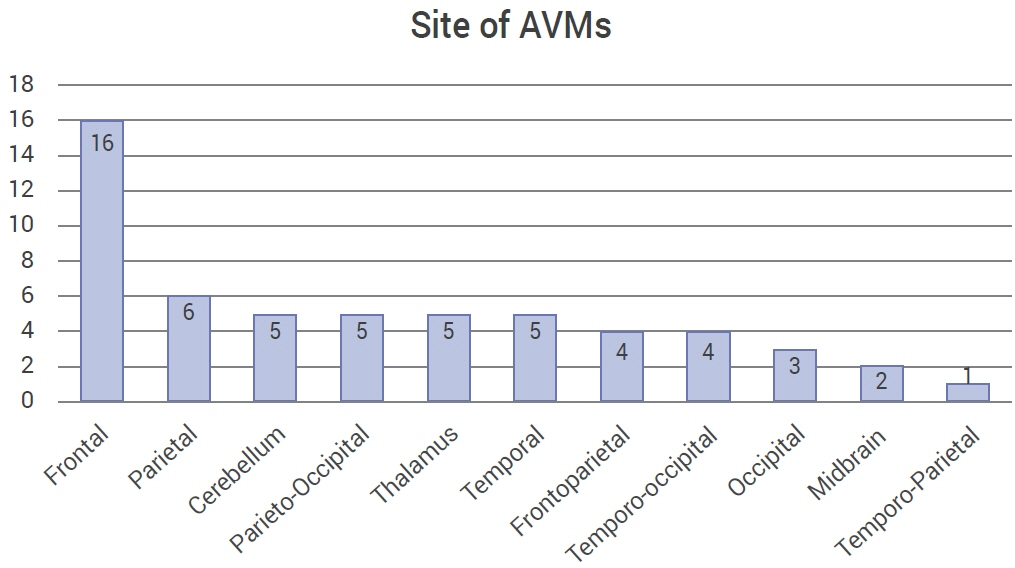
Data from 535 procedures was collected, we calculated an incidence of 4.4 cases per million inhabitants. Ninety procedures in 56 patients that used endovascular therapy were obtained with a female-male ratio of 0.75 and an age distribution of 35±14 (SD). A 36.3±11.5 (SD) mm diameter was registered. There was a 33% success rate for endovascular surgery.
Conclusions
The multidisciplinary treatment of AVMs is made up of three pillar techniques: microsurgical resection, embolization, and radio-neurosurgery. It is extremely important to make an appropriate decision, with an emphasis on achieving better functional outcomes for the patient. Although neurological endovascular therapy was initially used as an adjuvant treatment for neurosurgery and radio-neurosurgery, it has been used more and more frequently as the first line of treatment.
Figure
Reference
-
1. Baharvahdat H, Blanc R, Termechi R, Pistocchi S, Bartolini B, Redjemet H, et al. Hemorrhagic complications after endovascular treatment of cerebral arteriovenous malformations. AJNR Am J Neuroradiol. 2014; May. 35(5):978–83.2. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988; Dec. 19(12):1497–500.3. Chen CJ, Ding D, Derdeyn CP, Lanzino G, Friedlander RM, Southerland AM, et al. Brain arteriovenous malformations: a review of natural history, pathobiology, and interventions. Neurology. 2020; Nov. 95(20):917–27.4. Chen CJ, Norat P, Ding D, Mendes GAC, Tvrdik P, Park MS, et al. Transvenous embolization of brain arteriovenous malformations: a review of techniques, indications, and outcomes. Neurosurg Focus. 2018; Jul. 45(1):e13.5. Chen CJ, Shabo LM, Ding D, Ironside N, Kano H, Mathieu D, et al. Seizure presentation in patients with brain arteriovenous malformations treated with stereotactic radiosurgery: a multicenter study. World Neurosurg. 2019; Jun. 126:e634–40.6. Chen W, Choi EJ, McDougall CM, Su H. Brain arteriovenous malformation modeling, pathogenesis, and novel therapeutic targets. Transl Stroke Res. 2014; Jun. 5(3):316–29.7. Comisión Cordinadora de Institutos Nacionales de Salud y Hospitales de Aalta Especialidad. Manual de organización específico del Instituto Nacional de Neurología y Neurocirugía Manuel Velasco Suárez Gobierno de México, Diciembre 2016. http://www.innn.salud.gob.mx/descargas/instituto/normateca/man_org_12.pdf.8. Dumont TM, Kan P, Snyder KV, Hopkins LN, Siddiqui AH, Levy EI. A proposed grading system for endovascular treatment of cerebral arteriovenous malformations: Buffalo score. Surg Neurol Int. 2015; Jan. 6:3.9. García-Muñoz L, Vargas-Herrera A, Luján-Castilla P, Villaseñor-Navarro L. Malformaciones arteriovenosas tratadas con radiocirugía: experiencia en el Hospital General de México. Rev Mex Neuroci. 2010; 11(1):26–9.10. González-Block MA, Reyes-Morales H, Cahuana-Hurtado L, Balandrán A, Méndez E. Mexico: health system review. World Health Organization. Regional Office for Europe. Health Systems in Transition. 2020; 22(2):222. https://apps.who.int/iris/handle/10665/334334.11. Halim AX, Singh V, Johnston SC, Higashida RT, Dowd CF, Halbach VV, et al. Characteristics of brain arteriovenous malformations with coexisting aneurysms a comparison of two referral centers. Stroke. 2002; Mar. 33(3):675–9.12. Hernesniemi JA, Dashti R, Juvela S, Väärt K, Niemelä M, Laakso A. Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery. 2008; Nov. 63(5):823–9. discussion 829-31.13. Hofmeister C, Stapf C, Hartmann A, Sciacca RR, Mansmann U, terBrugge K, et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke. 2000; Jun. 31(6):1307–10.14. Instituto Nacional de Estadística; Geografía e Informática. Demografía y sociedad. derechos reservados. Last visit:28 Mar, 2022. https://www.inegi.org.mx/temas/estructura/.15. Kim H, Abla AA, Nelson J, McCulloch CE, Bervini D, Morgan MK, et al. Validation of the supplemented Spetzler-Martin grading system for brain arteriovenous malformations in a multicenter cohort of 1009 surgical patients. Neurosurgery. 2015; Jan. 76(1):25–31.16. Komiyama M. Pathogenesis of brain arteriovenous malformations. Neurol Med Chir (Tokyo). 2016; Jun. 56(6):317–25.17. Koo HW, Jo KI, Yeon JY, Kim KH, Jeon P, Kim JS, et al. Clinical features of superficially located brain arteriovenous malformations with transdural arterial communication. Cerebrovasc Dis. 2016; 41(3-4):204–10.18. Larios C, Mimenza-Alvarado A, Zenteno M, Murillo-Bonilla L, Sánchez-Hernández J, García-Ramos G, et al. Comportamiento de las malformaciones arteriovensosas cerebrales: estudio de una cohorte de 302 pacientes. Rev Mex Neuroci. 2010; 11(5):330–7.19. Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010; Apr. 66(4):702–13. discussion 713.20. Lopes DK, Moftakhar R, Straus D, Munich SA, Chaus F, Kaszuba MC. Arteriovenous malformation embocure score: AVMES. J Neurointerv Surg. 2016; Jul. 8(7):685–91.21. Lv X, Wu Z, Li Y, Yang X, Jiang C. Hemorrhage risk after partial endovascular NBCA and ONYX embolization for brain arteriovenous malformation. Neurol Res. 2012; Jul. 34(6):552–6.22. Mast H, Young WL, Koennecke H, Sciacca RR, Osipov A, Pile-Spellman J, et al. Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet. 1997; Oct. 350(9084):1065–8.23. Melo-Guzmán G, Padilla-Vázquez F, Escobar-de la Garma VH, Mendizábal-Guerra R. Experiencia en el manejo de malformaciones arteriovenosas cerebrales en el Hospital Juárez de México. Rev Mex Neuroci. 2017; 18(2):65–75.24. Mendes GAC, Kalani MYS, Iosif C, Lucena AF, Carvalho R, Saleme S, et al. Transvenous curative embolization of cerebral arteriovenous malformations: a prospective cohort study. Neurosurgery. 2018; Nov. 83(5):957–64.25. Morales-Valero SF, Bortolotti C, Sturiale C, Lanzino G. Are parenchymal AVMs congenital lesions? Neurosurg Focus. 2014; Sep. 37(3):e2.26. Pollock BE, Link MJ, Stafford SL, Garces YI, Foote RL. Stereotactic radiosurgery for arteriovenous malformations: the effect of treatment period on patient outcomes. Neurosurgery. 2016; Apr. 78(4):499–508.27. Pulli B, Stapleton CJ, Walcott BP, Koch MJ, Raymond SB, Leslie- Mazwi TM, et al. Comparison of predictive grading systems for procedural risk in endovascular treatment of brain arteriovenous malformations: analysis of 104 consecutive patients. J Neurosurg. 2019; Jun. 133(2):342–50.28. Rankin J. Cerebral vascular accidents in patients over the age of 60. Scott Med J. 1957; May. 2(5):200–15.29. Rodríguez-Parra V, Aburto-Murrieta Y, Zenteno-Castellanos MA. Descripción de factores clínicos y angiográficos asociados a hemorragia en malformaciones arteriovenosas cerebrales tratadas con embolización. Arch Neurocien (Mex),. 2010; 15(4):211–6.30. Saatci I, Geyik S, Yavuz K, Cekirge HS. Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: long-term results in 350 consecutive patients with completed endovascular treatment course. J Neurosurg. 2011; Jul. 115(1):78–88.31. Soderman M, Rodesch G, Lasjaunias P. Transdural blood supply to cerebral arteriovenous malformations adjacent to the dura mater. AJNR Am J Neuroradiol. 2002; Sep. 23(8):1295–300.32. Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986; Oct. 65(4):476–83.33. Starke RM, Kano H, Ding D, Lee JYK, Mathieu D, Whitesell J, et al. Stereotactic radiosurgery for cerebral arteriovenous malformations: evaluation of long-term outcomes in a multicenter cohort. J Neurosurg. 2017; Jan. 126(1):36–44.34. STROBE. Strengthening the reporting of observational studies in epidemiology. STROBE. Last visit:31 Mar, 2022. https://www.strobe-statement.org/.35. Sugiyama T, Grasso G, Torregrossa F, Fujimura M. Current concepts and perspectives on brain arteriovenous malformations: a review of pathogenesis and multidisciplinary treatment. World Neurosurg. 2022; Mar. 159:314–26.36. Thomas JM, Surendran S, Abraham M, Rajavelu A, Kartha CC. Genetic and epigenetic mechanisms in the development of arteriovenous malformations in the brain. Vol. 8, Clinical Epigenetics. Clin Epigenetics. 2016; Jul. 8:78.37. Unnithan A. Overview of the current concepts in the management of arteriovenous malformations of the brain. Postgrad Med J. 2020; Apr. 96(1134):212–20.38. Van Rooij WJ, Jacobs S, Sluzewski M, Van Der Pol B, Beute GN, Sprengers ME. Curative embolization of brain arteriovenous malformations with onyx: patient selection, embolization technique, and results. AJNR Am J Neuroradiol. 2012; Aug. 33(7):1299–304.39. Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; May. 19(5):604–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Management of Arteriovenous Malformation Diagnosed after Extremity Trauma
- Endovascular Treatment of Dural Sinus Malformation in Infant: A Case Report
- Stereotactic radiosurgery as an alternative treatment for dural arteriovenous fistula
- Scrotal Arteriovenous Malformation
- Foreign body granuloma reaction after endovascular therapy of an unruptured right frontal arteriovenous malformation