J Cerebrovasc Endovasc Neurosurg.
2020 Dec;22(4):267-272. 10.7461/jcen.2020.E2019.09.006.
Foreign body granuloma reaction after endovascular therapy of an unruptured right frontal arteriovenous malformation
- Affiliations
-
- 1Department of Surgery-Neurosurgery, Arzobispo Loayza National Hospital, Lima, Peru
- 2Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
- 3Department of Neurosurgery, Ospedali Riuniti Marche Nord, Pesaro, Italy
- 4Department of Pathology, Alberto Hurtado School of Medicine, Universidad Peruana Cayetano Heredia, Lima, Peru
- 5Department of Neurosurgery, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
- KMID: 2511040
- DOI: http://doi.org/10.7461/jcen.2020.E2019.09.006
Abstract
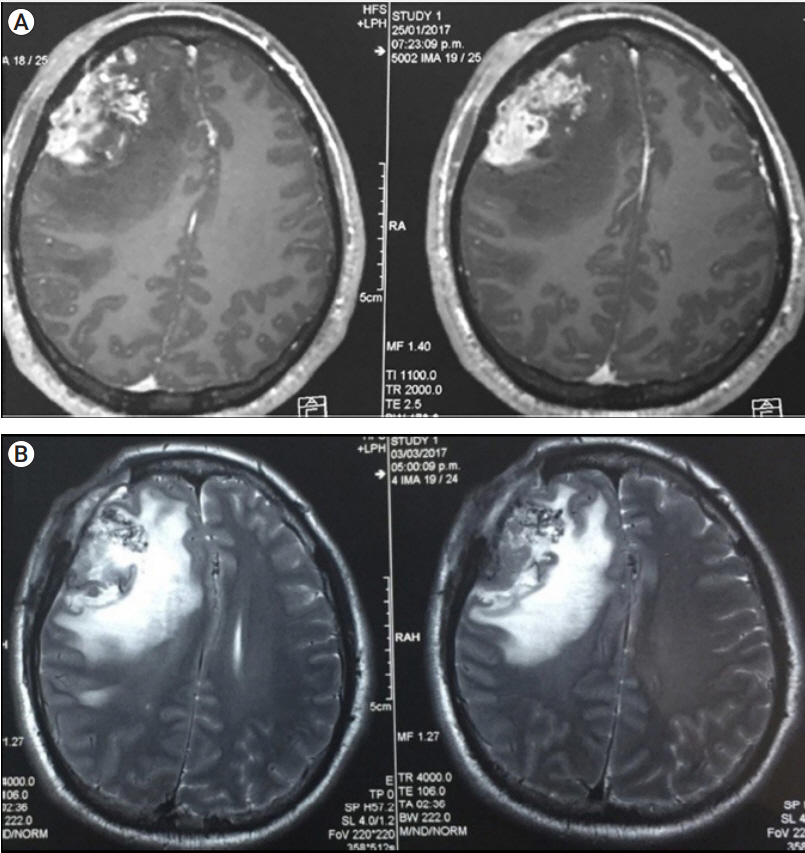
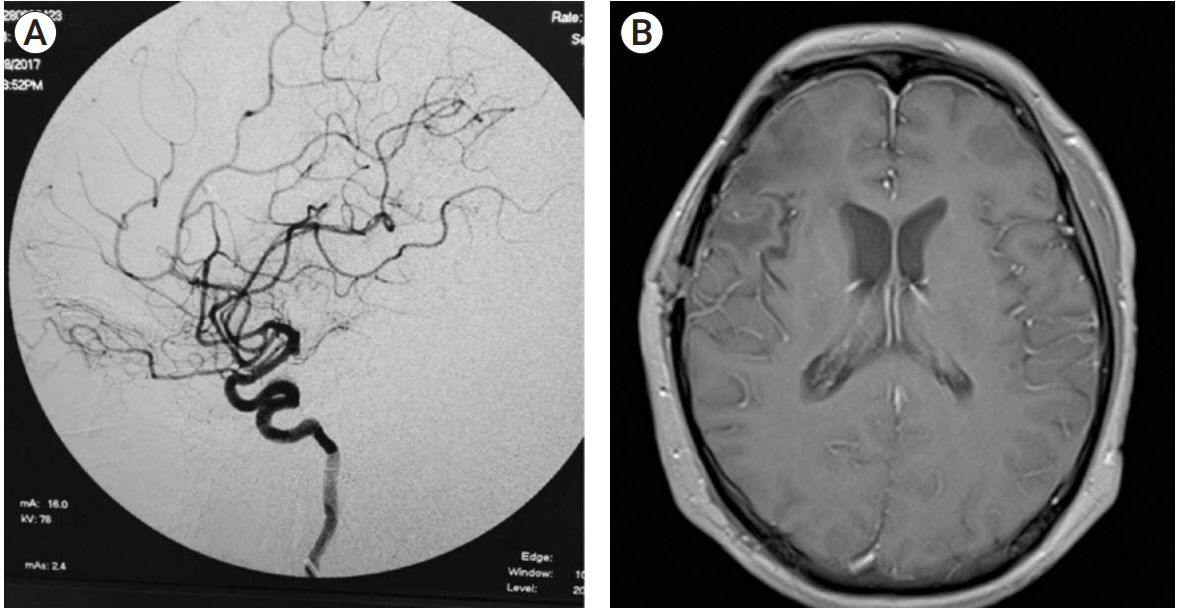
- Foreign body reactions after endovascular procedures for brain arteriovenous malformations are extremely rare. We report the case of a cerebral foreign body granuloma reaction after embolization of a frontal arteriovenous malformation with Onyx. A previously treated 36-year-old man underwent re-embolization of a residual and recurrent unruptured right frontal vascular malformation with Onyx. The post-procedural imaging revealed a right frontotemporal heterogeneously enhancing expansive lesion associated with a residual malformation. Following microsurgical resection, the histopathological examination of the expansive lesion revealed basophilic foreign body like deposits adjacent to multi-nucleated giant cells, highly compatible with cerebral foreign body granulomas reaction to Onyx. The clinical and radiological follow-up of the patient was favorable after complete resection of the lesions.
Keyword
Figure
Reference
-
1. Brown RD Jr, Wiebers DO, Forbes G, O’Fallon WM, Piepgras DG, Marsh WR, et al. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg. 1988; Mar. 68(3):352–7.
Article2. Brown RD Jr, Wiebers DO, Torner JC, O’Fallon WM. Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis: a population-based study of intracranial vascular malformations in Olmsted Country, Minnesota. J Neurosurg. 1996; Jul. 85(1):29–32.3. Choque-Velasquez J, Kozyrev DA, Colasanti R, Thiarawat P, Intarakhao P, Jahromi BR, et al. The open access video collection project “Hernesniemi’s 1001 and more microsurgical videos of Neurosurgery”: A legacy for educational purposes. Surg Neurol Int. 2017; Aug. 8:188.
Article4. Dinesh SK, Lee SY, Thomas J. A case of mistaken identity: intracranial foreign body reaction after AVM embolisation mimicking a glioma. J Clin Neurosci. 2008; Apr. 15(4):463–5.
Article5. Duffner F, Ritz R, Bornemann A, Freudenstein D, Wiendl H, Siekmann R. Combined therapy of cerebral arteriovenous malformations: histological differences between a non-adhesive liquid embolic agent and n-butyl 2-cyanoacrylate (NBCA). Clin Neuropathol. 2002; Jan-Feb. 21(1):13–7.6. Gunawat P, Shaikh ST, Karmarkar V, Deopujari C. Symptomatic granuloma secondary to embolic agent: A case report. J Clin Diagn Res. 2016; Nov. 10(11):PD15–6.7. Jahan R, Murayama Y, Gobin YP, Duckwiler GR, Vinters HV, Viñuela F. Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patients. Neurosurgery. 2001; May. 48(5):984–95; discussion 995.
Article8. Liu CY, Yonkers MA, Liu TS, Minckler DS, Tao JP. Vascular steal syndrome, optic neuropathy, and foreign body granuloma reaction to Onyx-18 embolization for congenital orbito-facial vascular malformation. Ocul Oncol Pathol. 2016; Apr. 2(3):185–9.
Article9. Murayama Y, Viñuela F, Ulhoa A, Akiba Y, Duckwiler GR, Gobin YP, et al. Nonadhesive liquid embolic agent for cerebral arteriovenous malformations: preliminary histopathological studies in swine rete mirabile. Neurosurgery. 1998; Nov. 43(5):1164–75.
Article10. Natarajan SK, Born D, Ghodke B, Britz GW, Sekhar LN. Histopathological changes in brain arteriovenous malformations after embolization using Onyx or N-butyl cyanoacrylate. Laboratory investigation. J Neurosurg. 2009; Jul. 111(1):105–13.11. Panagiotopoulos V, Gizewski E, Asgari S, Regel J, Forsting M, Wanke I. Embolization of intracranial arteriovenous malformations with ethylene-vinyl alcohol copolymer (Onyx). AJNR Am J Neuroradiol. 2009; Jan. 30(1):99–106.
Article12. van Rooij WJ, Sluzewski M, Beute GN. Brain AVM embolization with Onyx. AJNR Am J Neuroradiol. 2007; Jan. 28(1):172–7; discussion 178.13. Singla A, Fargen KM, Hoh B. Onyx extrusion through the scalp after embolization of dural arteriovenous fistula. J Neurointerv Surg. 2016; Sep. 8(9):e38.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Foreign Body Granuloma after Squalene Injection by Non-dermatologists
- The Management of Arteriovenous Malformation Diagnosed after Extremity Trauma
- Foreign-body Granuloma After Honeybee Acupuncture
- A Case of Foreign Body Granulomatous Reaction to a Red Lip Cosmetic Tattoo Successfully Treated with Carbon Dioxide Laser
- Foreign Body Granuloma after Filler Injection Treated with Liposuction