J Korean Med Sci.
2023 Mar;38(11):e83. 10.3346/jkms.2023.38.e83.
Neurological and Psychiatric Manifestations of Post-COVID-19 Conditions
- Affiliations
-
- 1Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 2Department of Pulmonary and Critical Care Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 3Department of Family Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 4Department of Infectious Disease, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 5The Office of Chief Executive Officer and Chairman, Department of General Surgery, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- KMID: 2540650
- DOI: http://doi.org/10.3346/jkms.2023.38.e83
Abstract
- Background
We aimed to investigate the factors associated with neurological manifestations of post-coronavirus disease 2019 (COVID-19) conditions.
Methods
We retrospectively collected data from 440 patients who visited our post-COVID-19 clinic more than 4 weeks after severe acute respiratory syndrome coronavirus 2 infection. We analyzed the prevalence of different neurological symptoms (brain fog, memory impairment, headache, and dizziness) and assessed the associated factors.
Results
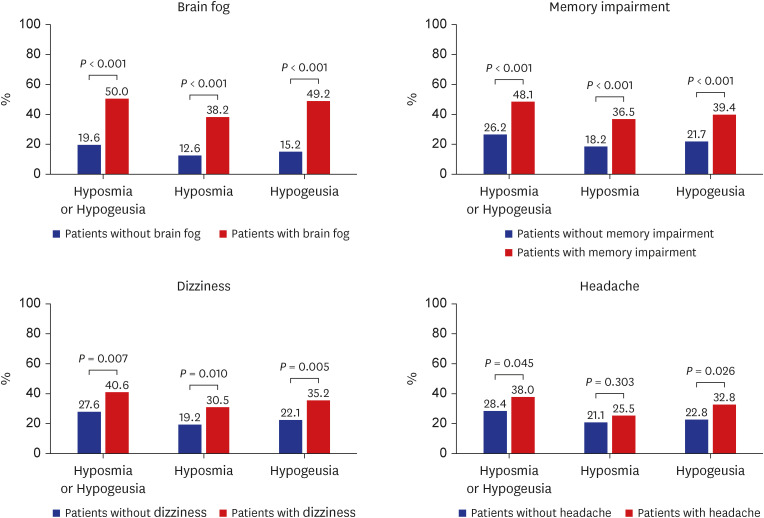
Brain fog was the most common symptom, observed in 170 patients (38.6%), followed by headaches (n = 137, 31.1%), dizziness (n = 128, 29%), and memory impairment (n = 104, 23.6%). Brain fog was associated with hyposmia or hypogeusia (odds ratio [OR], 2.54; P < 0.001), Fatigue Severity Scale (FSS) (OR, 1.06; P < 0.001), and Hospital Anxiety and Depression Scale-Anxiety (OR, 1.09; P = 0.037). Memory impairment was associated with sleep problems (OR, 2.83; P < 0.001), FSS (OR, 1.05; P < 0.001), and age (OR, 1.02; P = 0.015). Headache was associated with sleep problems (OR, 2.28; P= 0.001), sex (OR, 1.68; P = 0.042), and FSS (OR, 1.04; P < 0.001). Dizziness was associated with sleep problems (OR, 2.88; P < 0.001), and FSS (OR, 1.04; P < 0.001). The incidence of brain fog ( P < 0.001), memory impairment ( P < 0.001), dizziness (P = 0.007), and headache (P = 0.045) accompanied by hyposmia and hypogeusia was higher in patients with the aforementioned symptoms than in those without.
Conclusion
This study suggests that there is a relationship between neurological symptoms and other clinical factors, such as fatigue, depression, anxiety, hyposmia, and hypogeusia.
Figure
Reference
-
1. Our World in Data. Daily new confirmed COVID-19 deaths per million people. Updated 2022. Accessed August 25, 2022. https://ourworldindata.org/covid-deaths .2. Jung YH, Ha EH, Choe KW, Lee S, Jo DH, Lee WJ. Persistent symptoms after acute COVID-19 infection in Omicron era. J Korean Med Sci. 2022; 37(27):e213. PMID: 35818704.3. Ziauddeen N, Gurdasani D, O’Hara ME, Hastie C, Roderick P, Yao G, et al. Characteristics and impact of Long Covid: findings from an online survey. PLoS One. 2022; 17(3):e0264331. PMID: 35259179.4. Kim Y, Bitna-Ha , Kim SW, Chang HH, Kwon KT, Bae S, et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis. 2022; 22(1):93. PMID: 35086489.5. Kim Y, Kim SW, Chang HH, Kwon KT, Bae S, Hwang S. Significance and associated factors of long-term sequelae in patients after acute COVID-19 infection in Korea. Infect Chemother. 2021; 53(3):463–476. PMID: 34405592.6. Kim Y, Kim SE, Kim T, Yun KW, Lee SH, Lee E, et al. Preliminary guidelines for the clinical evaluation and management of long COVID. Infect Chemother. 2022; 54(3):566–597. PMID: 36196612.7. Soh HS, Cho B. Long COVID-19 and health-related quality of life of mild cases in Korea: 3-months follow-up of a single community treatment center. J Korean Med Sci. 2022; 37(46):e326. PMID: 36631024.8. Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. 2022; 434:120162. PMID: 35121209.9. Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022; 604(7907):697–707. PMID: 35255491.10. Martelletti P, Bentivegna E, Spuntarelli V, Luciani M. Long-COVID headache. SN Compr Clin Med. 2021; 3(8):1704–1706. PMID: 34036244.11. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370. PMID: 6880820.12. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002; 52(2):69–77. PMID: 11832252.13. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989; 46(10):1121–1123. PMID: 2803071.14. Hjollund NH, Andersen JH, Bech P. Assessment of fatigue in chronic disease: a bibliographic study of fatigue measurement scales. Health Qual Life Outcomes. 2007; 5(1):12. PMID: 17326844.15. Becker JH, Lin JJ, Doernberg M, Stone K, Navis A, Festa JR, et al. Assessment of cognitive function in patients after COVID-19 infection. JAMA Network Open. 2021; 4(10):e2130645. PMID: 34677597.16. Liu YH, Chen Y, Wang QH, Wang LR, Jiang L, Yang Y, et al. One-year trajectory of cognitive changes in older survivors of COVID-19 in Wuhan, China: a longitudinal cohort study. JAMA Neurol. 2022; 79(5):509–517. PMID: 35258587.17. Bolay H, Gül A, Baykan B. COVID-19 is a real headache! Headache. 2020; 60(7):1415–1421. PMID: 32412101.18. Membrilla J, Caronna E, Trigo-López J, González-Martínez A, Layos-Romero A, Pozo-Rosich P, et al. Persistent headache after COVID-19: pathophysioloy, clinic and treatment. Neurology Perspectives. 2021; 1:S31–S36.19. Rozen TD. Daily persistent headache after a viral illness during a worldwide pandemic may not be a new occurrence: lessons from the 1890 Russian/Asiatic flu. Cephalalgia. 2020; 40(13):1406–1409. PMID: 33146034.20. Diaz-Mitoma F, Vanast WJ, Tyrrell DL. Increased frequency of Epstein-Barr virus excretion in patients with new daily persistent headaches. Lancet. 1987; 329(8530):411–415.21. Calabria M, García-Sánchez C, Grunden N, Pons C, Arroyo JA, Gómez-Anson B, et al. Post-COVID-19 fatigue: the contribution of cognitive and neuropsychiatric symptoms. J Neurol. 2022; 269(8):3990–3999. PMID: 35488918.22. Moghimi N, Di Napoli M, Biller J, Siegler JE, Shekhar R, McCullough LD, et al. The neurological manifestations of post-acute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021; 21(9):44. PMID: 34181102.23. Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022; 101:93–135. PMID: 34973396.24. Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep. 2021; 9(3):e14726. PMID: 33523608.25. Lee CH, Giuliani F. The role of inflammation in depression and fatigue. Front Immunol. 2019; 10:1696. PMID: 31379879.26. Song WJ, Hui CKM, Hull JH, Birring SS, McGarvey L, Mazzone SB, et al. Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses. Lancet Respir Med. 2021; 9(5):533–544. PMID: 33857435.27. Sun B, Tang N, Peluso MJ, Iyer NS, Torres L, Donatelli JL, et al. Characterization and biomarker analyses of post-COVID-19 complications and neurological manifestations. Cells. 2021; 10(2):386. PMID: 33668514.28. Milaneschi Y, Kappelmann N, Ye Z, Lamers F, Moser S, Jones PB, et al. Association of inflammation with depression and anxiety: evidence for symptom-specificity and potential causality from UK Biobank and NESDA cohorts. Mol Psychiatry. 2021; 26(12):7393–7402. PMID: 34135474.29. Di Stadio A, Brenner MJ, De Luca P, Albanese M, D’Ascanio L, Ralli M, et al. Olfactory dysfunction, headache, and mental clouding in adults with long-COVID-19: what is the link between cognition and olfaction? A cross-sectional study. Brain Sci. 2022; 12(2):154. PMID: 35203918.30. Butowt R, von Bartheld CS. Anosmia in COVID-19: underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist. 2021; 27(6):582–603. PMID: 32914699.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurological Manifestations in Patients with COVID-19: Experiences from the Central Infectious Diseases Hospital in South Korea
- Descriptive analysis of the incidence rate of post-acute COVID-19 syndrome in the Republic of Korea Army
- Cardiovascular Manifestations of COVID-19
- Post-COVID-19 Syndrome
- State and Improvement Policy of Psychiatric Emergency during COVID-19 Pandemic