Acute Crit Care.
2023 Feb;38(1):104-112. 10.4266/acc.2022.01389.
Lower limb muscle matters in patients with hypoxic brain injury following out-of-hospital cardiac arrest
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Emergency Medicine, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 4Department of Emergency Medical Services, Kyungdong University, Wonju, Korea
- KMID: 2540320
- DOI: http://doi.org/10.4266/acc.2022.01389
Abstract
- Background
There are conflicting results regarding the association between body mass index and the prognosis of cardiac arrest patients. We investigated the association of the composition and distribution of muscle and fat with neurologic outcomes at hospital discharge in successfully resuscitated out-of-hospital cardiac arrest (OHCA) patients.
Methods
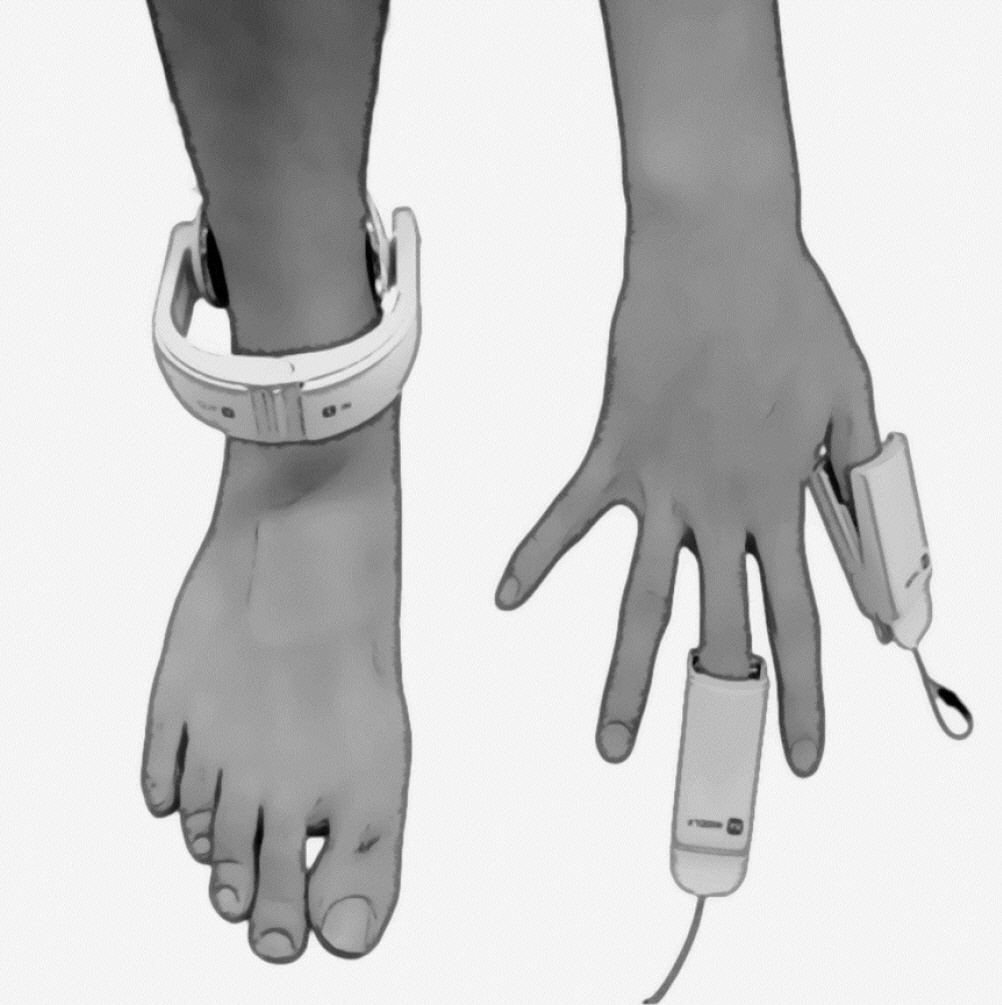
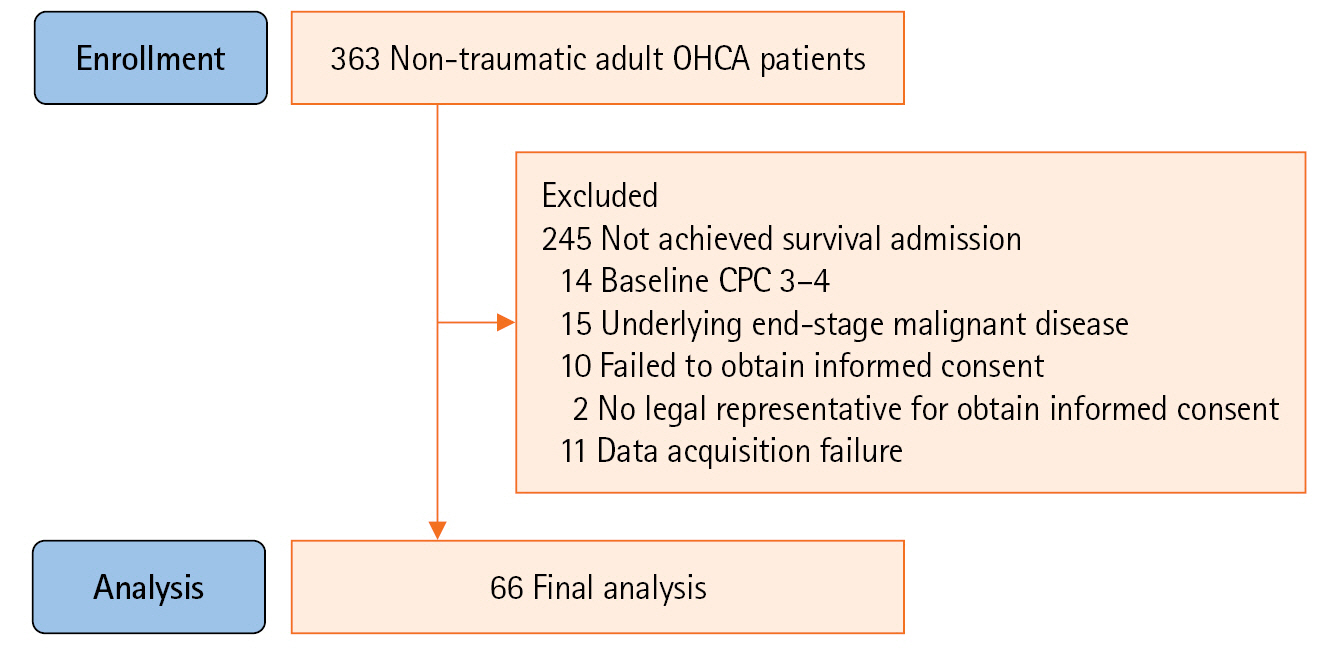
This prospective, single-centre, observational study involved adult OHCA patients, conducted between April 2019 and June 2021. The ratio of total skeletal muscle, upper limb muscle, lower limb muscle, and total fat to body weight was measured using InBody S10, a bioimpedance analyser, after achieving the return of spontaneous circulation. Restricted cubic spline curves with four knots were used to examine the relationship between total skeletal muscle, upper limb muscle, and lower limb muscle relative to total body weight and neurologic outcome at discharge. Multivariable logistic regression analysis was performed to assess an independent association.
Results
A total of 66 patients were enrolled in the study. The proportion of total muscle and lower limb muscle positively correlated with the possibility of having a good neurologic outcome. The proportion of lower limb muscle showed an independent association in the multivariable analysis (adjusted odds ratio, 2.29; 95% confidence interval, 1.06–13.98), and its optimal cut-off value calculated through receiver operating characteristic curve analysis was 23.1%, which can predict a good neurological outcome.
Conclusions
A higher proportion of lower limb muscle to body weight was independently associated with the probability of having a good neurologic outcome in OHCA patients.
Figure
Reference
-
1. Kiguchi T, Okubo M, Nishiyama C, Maconochie I, Ong ME, Kern KB, et al. Out-of-hospital cardiac arrest across the World: first report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020; 152:39–49.2. Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation. 2008; 79:350–79.3. Sekhon MS, Ainslie PN, Griesdale DE. Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a “two-hit” model. Crit Care. 2017; 21:90.4. Majewski D, Ball S, Finn J. Systematic review of the relationship between comorbidity and out-of-hospital cardiac arrest outcomes. BMJ Open. 2019; 9:e031655.5. Geri G, Savary G, Legriel S, Dumas F, Merceron S, Varenne O, et al. Influence of body mass index on the prognosis of patients successfully resuscitated from out-of-hospital cardiac arrest treated by therapeutic hypothermia. Resuscitation. 2016; 109:49–55.6. Gupta T, Kolte D, Mohananey D, Khera S, Goel K, Mondal P, et al. Relation of obesity to survival after in-hospital cardiac arrest. Am J Cardiol. 2016; 118:662–7.7. Ma Y, Huang L, Zhang L, Yu H, Liu B. Association between body mass index and clinical outcomes of patients after cardiac arrest and resuscitation: a meta-analysis. Am J Emerg Med. 2018; 36:1270–9.8. Lee H, Oh J, Kang H, Lim TH, Ko BS, Choi HJ, et al. Association between the body mass index and outcomes of patients resuscitated from out-of-hospital cardiac arrest: a prospective multicentre registry study. Scand J Trauma Resusc Emerg Med. 2021; 29:24.9. Bang HJ, Park KN, Youn CS, Kim HJ, Oh SH, Lim JY, et al. The relationship between body mass index and neurologic outcomes in survivors of out-of-hospital cardiac arrest treated with targeted temperature management. PLoS One. 2022; 17:e0265656.10. Kim DW, Choi JK, Won SH, Yun YJ, Jo YH, Park SM, et al. A new variant position of head-up CPR may be associated with improvement in the measurements of cranial near-infrared spectroscopy suggestive of an increase in cerebral blood flow in non-traumatic out-of-hospital cardiac arrest patients: a prospective interventional pilot study. Resuscitation. 2022; 175:159–66.11. Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S444–64.12. Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020; 142(16_suppl_2):S366–468.13. Lee SY, Ahn S, Kim YJ, Ji MJ, Kim KM, Choi SH, et al. Comparison between dual-energy X-ray absorptiometry and bioelectrical impedance analyses for accuracy in measuring whole body muscle mass and appendicular skeletal muscle mass. Nutrients. 2018; 10:738.14. Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, et al. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr. 2011; 30:610–5.15. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015; 132:1286–300.16. Lee SE, Kim HH, Chae MK, Park EJ, Choi S. Predictive value of estimated lean body mass for neurological outcomes after out-of-hospital cardiac arrest. J Clin Med. 2020; 10:71.17. Pickkers P, de Keizer N, Dusseljee J, Weerheijm D, van der Hoeven JG, Peek N. Body mass index is associated with hospital mortality in critically ill patients: an observational cohort study. Crit Care Med. 2013; 41:1878–83.18. Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity (Silver Spring). 2008; 16:515–21.19. Bone AE, Hepgul N, Kon S, Maddocks M. Sarcopenia and frailty in chronic respiratory disease. Chron Respir Dis. 2017; 14:85–99.20. Nichols S, O’Doherty AF, Taylor C, Clark AL, Carroll S, Ingle L. Low skeletal muscle mass is associated with low aerobic capacity and increased mortality risk in patients with coronary heart disease: a CARE CR study. Clin Physiol Funct Imaging. 2019; 39:93–102.21. Hong SI, Kim KW, Ko Y, Kim YJ, Huh JW, Hong SB, et al. Long-term outcomes after in-hospital cardiac arrest: does pre-arrest skeletal muscle depletion matter? Front Physiol. 2021; 12:692757.22. Tian S, Xu Y. Association of sarcopenic obesity with the risk of all-cause mortality: a meta-analysis of prospective cohort studies. Geriatr Gerontol Int. 2016; 16:155–66.23. Zhang X, Xie X, Dou Q, Liu C, Zhang W, Yang Y, et al. Association of sarcopenic obesity with the risk of all-cause mortality among adults over a broad range of different settings: a updated meta-analysis. BMC Geriatr. 2019; 19:183.24. Walsh K. Adipokines, myokines and cardiovascular disease. Circ J. 2009; 73:13–8.25. Chung HS, Choi KM. Adipokines and myokines: a pivotal role in metabolic and cardiovascular disorders. Curr Med Chem. 2018; 25:2401–15.26. Pedersen BK, Febbraio MA. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev. 2008; 88:1379–406.27. Lee MJ, Kim EH, Bae SJ, Choe J, Jung CH, Lee WJ, et al. Protective role of skeletal muscle mass against progression from metabolically healthy to unhealthy phenotype. Clin Endocrinol (Oxf). 2019; 90:102–13.28. Staiano AE, Gupta AK, Katzmarzyk PT. Cardiometabolic risk factors and fat distribution in children and adolescents. J Pediatr. 2014; 164:560–5.29. Yang M, Lin J, Ma X, Zhu C, Wei C, Wang L, et al. Truncal and leg fat associations with metabolic risk factors among Chinese adults. Asia Pac J Clin Nutr. 2016; 25:798–809.30. Jung S, Park J, Seo YG. Relationship between arm-to-leg and limbs-to-trunk body composition ratio and cardiovascular disease risk factors. Sci Rep. 2021; 11:17414.31. Abreo AP, Bailey SR, Abreo K. Associations between calf, thigh, and arm circumference and cardiovascular and all-cause mortality in NHANES 1999-2004. Nutr Metab Cardiovasc Dis. 2021; 31:1410–5.32. Kremer WM, Labenz C, Kuchen R, Sagoschen I, Bodenstein M, Schreiner O, et al. Sonographic assessment of low muscle quantity identifies mortality risk during COVID-19: a prospective single-centre study. J Cachexia Sarcopenia Muscle. 2022; 13:169–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prolonged Delirium Secondary to Hypoxic-ischemic Encephalopathy Following Cardiac Arrest
- Comparison of Prognosis between the Hypoxic-Hypotensive Brain Injured and Traumatic Brain Injured Patients
- Targeted temperature management with hypothermia for comatose patients after cardiac arrest
- Management of Brain Injury after Post-cardiac Arrest Syndrome
- Number Processing Error as a Clinical Manifestation of Hemispatial Neglect Following Hypoxic Brain Injury:a Case Report