Acute Crit Care.
2022 Nov;37(4):601-609. 10.4266/acc.2022.00542.
Association between C-reactive protein-to-albumin ratio and 6-month mortality in out-of-hospital cardiac arrest
- Affiliations
-
- 1Department of Emergency Medicine, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Emergency Medicine, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2540148
- DOI: http://doi.org/10.4266/acc.2022.00542
Abstract
- Background
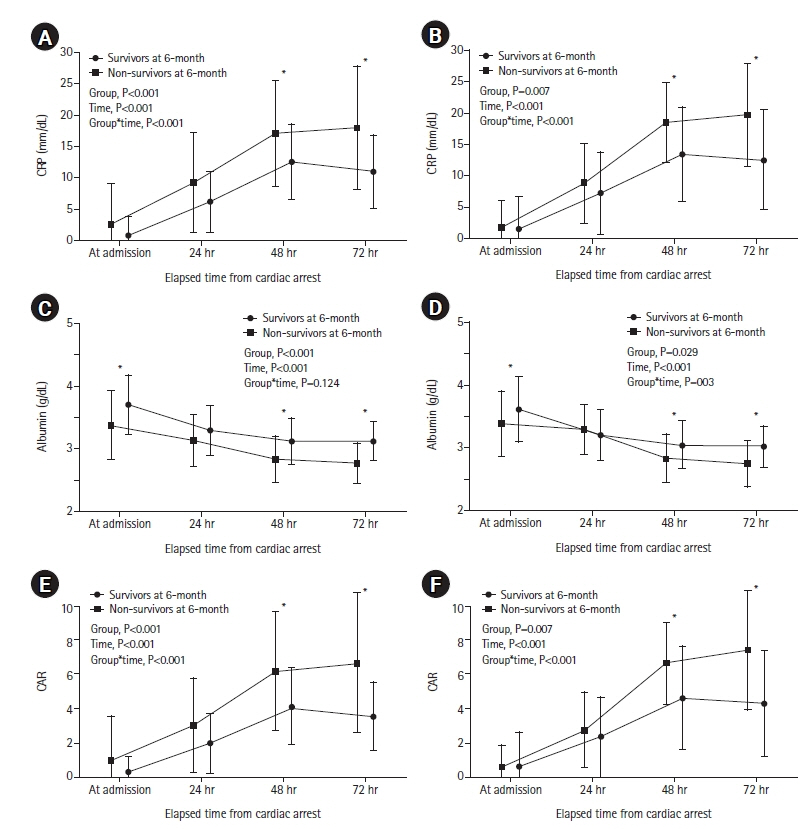
The inflammatory response that occurs following cardiac arrest can determine the long-term prognosis of patients who survive out-of-hospital cardiac arrest. We evaluated the correlation between C-reactive protein-to-albumin ratio (CAR) following cardiac arrest and long-term mortality. Methods: The current retrospective observational study examined patients with post-cardiac arrest syndrome (PCAS) treated with targeted temperature management at a single tertiary care hospital. We measured CAR at four time points (at admission and then 24 hours, 48 hours, and 72 hours after) following cardiac arrest. The primary outcome was the patients’ 6-month mortality. We performed multivariable and area under the receiver operating characteristic curve (AUC) analyses to investigate the relationship between CAR and 6-month mortality. Results: Among the 115 patients, 52 (44.1%) died within 6 months. In the multivariable analysis, CAR at 48 hours (odds ratio [OR], 1.130; 95% confidence interval [CI], 1.027–1.244) and 72 hours (OR, 1.241; 95% CI, 1.059–1.455) after cardiac arrest was independently associated with 6-month mortality. The AUCs of CAR at admission and 24, 48, and 72 hours after cardiac arrest for predicting 6-month mortality were 0.583 (95% CI, 0.489–0.673), 0.622 (95% CI, 0.528–0.710), 0.706 (95% CI, 0.615–0.786), and 0.762 (95% CI, 0.675–0.835), respectively. Conclusions: CAR at 72 hours after cardiac arrest was an independent predictor for long-term mortality in patients with PCAS.
Keyword
Figure
Reference
-
1. Du L, Zheng K, Feng L, Cao Y, Niu Z, Song Z, et al. The first national survey on practices of neurological prognostication after cardiac arrest in China, still a lot to do. Int J Clin Pract. 2021; 75:e13759.
Article2. Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines for post-resuscitation care 2015: section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015; 95:202–22.
Article3. Widgerow AD. Ischemia-reperfusion injury: influencing the microcirculatory and cellular environment. Ann Plast Surg. 2014; 72:253–60.4. Weiser C, Schwameis M, Sterz F, Herkner H, Lang IM, Schwarzinger I, et al. Mortality in patients resuscitated from out-of-hospital cardiac arrest based on automated blood cell count and neutrophil lymphocyte ratio at admission. Resuscitation. 2017; 116:49–55.
Article5. Engel H, Ben Hamouda N, Portmann K, Delodder F, Suys T, Feihl F, et al. Serum procalcitonin as a marker of post-cardiac arrest syndrome and long-term neurological recovery, but not of early-onset infections, in comatose post-anoxic patients treated with therapeutic hypothermia. Resuscitation. 2013; 84:776–81.
Article6. Mongardon N, Lemiale V, Perbet S, Dumas F, Legriel S, Guérin S, et al. Value of procalcitonin for diagnosis of early onset pneumonia in hypothermia-treated cardiac arrest patients. Intensive Care Med. 2010; 36:92–9.
Article7. Mongardon N, Perbet S, Lemiale V, Dumas F, Poupet H, Charpentier J, et al. Infectious complications in out-of-hospital cardiac arrest patients in the therapeutic hypothermia era. Crit Care Med. 2011; 39:1359–64.
Article8. Perbet S, Mongardon N, Dumas F, Bruel C, Lemiale V, Mourvillier B, et al. Early-onset pneumonia after cardiac arrest: characteristics, risk factors and influence on prognosis. Am J Respir Crit Care Med. 2011; 184:1048–54.9. Ning P, Yang B, Yang X, Huang H, Shen Q, Zhao Q, et al. Clinical value of C-reactive protein/albumin ratio in Guillain-Barré syndrome. Neurol Sci. 2021; 42:3275–83.
Article10. Wang R, He M, Ou X, Xie X, Kang Y. CRP albumin ratio is positively associated with poor outcome in patients with traumatic brain injury. Clin Neurol Neurosurg. 2020; 195:106051.
Article11. Karabağ Y, Çağdaş M, Rencuzogullari I, Karakoyun S, Artaç İ, İliş D, et al. Usefulness of the C-reactive protein/albumin ratio for predicting no-reflow in ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Eur J Clin Invest. 2018; 48:e12928.
Article12. Kocatürk M, Kocatürk Ö. Assessment of relationship between C-reactive protein to albumin ratio and 90-day mortality in patients with acute ischaemic stroke. Neurol Neurochir Pol. 2019; 53:205–11.
Article13. Bisschops LL, van der Hoeven JG, Mollnes TE, Hoedemaekers CW. Seventy-two hours of mild hypothermia after cardiac arrest is associated with a lowered inflammatory response during rewarming in a prospective observational study. Crit Care. 2014; 18:546.
Article14. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–45.
Article15. Li YM, Liu XY. Serum levels of procalcitonin and high sensitivity C-reactive protein are associated with long-term mortality in acute ischemic stroke. J Neurol Sci. 2015; 352:68–73.
Article16. Amnuaypattanapon K, Thanachartwet V, Desakorn V, Chamnanchanunt S, Pukrittayakamee S, Sahassananda D, et al. Predictive model of return of spontaneous circulation among patients with out-of-hospital cardiac arrest in Thailand: the WATCH-CPR score. Int J Clin Pract. 2020; 74:e13502.
Article17. Schriefl C, Schoergenhofer C, Poppe M, Clodi C, Mueller M, Ettl F, et al. Admission C-reactive protein concentrations are associated with unfavourable neurological outcome after out-of-hospital cardiac arrest. Sci Rep. 2021; 11:10279.
Article18. Dufner MC, Andre F, Stiepak J, Zelniker T, Chorianopoulos E, Preusch M, et al. Therapeutic hypothermia impacts leukocyte kinetics after cardiac arrest. Cardiovasc Diagn Ther. 2016; 6:199–207.
Article19. Annborn M, Dankiewicz J, Erlinge D, Hertel S, Rundgren M, Smith JG, et al. Procalcitonin after cardiac arrest: an indicator of severity of illness, ischemia-reperfusion injury and outcome. Resuscitation. 2013; 84:782–7.
Article20. Cipolla MJ, Crete R, Vitullo L, Rix RD. Transcellular transport as a mechanism of blood-brain barrier disruption during stroke. Front Biosci. 2004; 9:777–85.
Article21. Li J, Li C, Yuan W, Wu J, Li J, Li Z, et al. Mild hypothermia alleviates brain oedema and blood-brain barrier disruption by attenuating tight junction and adherens junction breakdown in a swine model of cardiopulmonary resuscitation. PLoS One. 2017; 12:e0174596.
Article22. Yoon H, Song KJ, Shin SD, Ro YS, Hong KJ, Park JH. Effect of serum albumin level on hospital outcomes in out-of-hospital cardiac arrest. Hong Kong J Emerg Med. 2020; 27:293–9.
Article23. Bingol Tanriverdi T, Patmano G, Bozkurt FT, Kaya BC, Tercan M. Prognostic value of C-reactive protein to albumin ratio in patients resuscitated from out-of-hospital cardiac arrest. Int J Clin Pract. 2021; 75:e14227.
Article24. Akin M, Sieweke JT, Zauner F, Garcheva V, Tongers J, Napp LC, et al. Mortality in patients with out-of-hospital cardiac arrest undergoing a standardized protocol including therapeutic hypothermia and routine coronary angiography: experience from the HACORE Registry. JACC Cardiovasc Interv. 2018; 11:1811–20.25. Tabi M, Burstein BJ, Ahmed A, Dezfulian C, Kashani KB, Jentzer JC. Shock severity and hospital mortality in out of hospital cardiac arrest patients treated with targeted temperature management. Shock. 2021; 55:48–54.
Article26. Shi J, Dai W, Kloner RA. Therapeutic hypothermia reduces the inflammatory response following ischemia/reperfusion injury in rat hearts. Ther Hypothermia Temp Manag. 2017; 7:162–70.
Article27. Wenisch C, Narzt E, Sessler DI, Parschalk B, Lenhardt R, Kurz A, et al. Mild intraoperative hypothermia reduces production of reactive oxygen intermediates by polymorphonuclear leukocytes. Anesth Analg. 1996; 82:810–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Significance of Initial Serum Albumin on Mortality in Out-of-hospital Cardiac Arrest
- High-sensitivity C-reactive protein/albumin ratio as a predictor of in-hospital mortality in older adults admitted to the emergency department
- C-reactive protein-to-albumin ratio is a predictor of 1-year mortality following liver transplantation
- The Usefulness of Heart-type Fatty Acid binding Protein and Ischemia Modified Albumin to Diagnose the Cardiac cause of Arrest and the Difference of the Two Biomarkers between the Return of Spontaneous Circulation (ROSC) group and the non-ROSC group
- Change in Red Cell Distribution Width as Predictor of Death and Neurologic Outcome in Patients Treated with Therapeutic Hypothermia after Out-of-Hospital Cardiac Arrest