J Korean Med Sci.
2023 Mar;38(9):e65. 10.3346/jkms.2023.38.e65.
Clinical Characteristics and Outcomes of Children With SARS-CoV-2 Infection During the Delta and Omicron VariantDominant Periods in Korea
- Affiliations
-
- 1Department of Pediatrics, Pusan National University School of Medicine, Busan, Korea
- 2Department of Pediatrics, Jeju National University School of Medicine, Jeju, Korea
- 3Department of Pediatrics, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- 4Department of Pediatrics, Nowon Eulji University Hospital, Seoul, Korea
- 5Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea
- 6Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2540123
- DOI: http://doi.org/10.3346/jkms.2023.38.e65
Abstract
- Background
Data on the clinical characteristics of pediatric patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variant infection are limited. We aimed to evaluate the clinical features and outcomes of children with SARS-CoV-2 infection before and after omicron variant dominance in Korea.
Methods
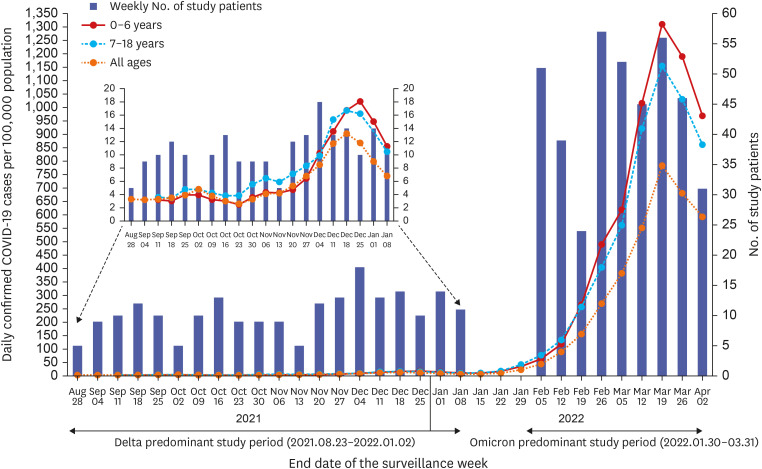
A multicenter retrospective cohort study was conducted in hospitalized patients aged ≤ 18 years with laboratory-confirmed SARS-CoV-2 infection at five university hospitals in South Korea. The study periods were divided into the delta (from August 23, 2021 to January 2, 2022) and omicron (from January 30 to March 31, 2022).
Results
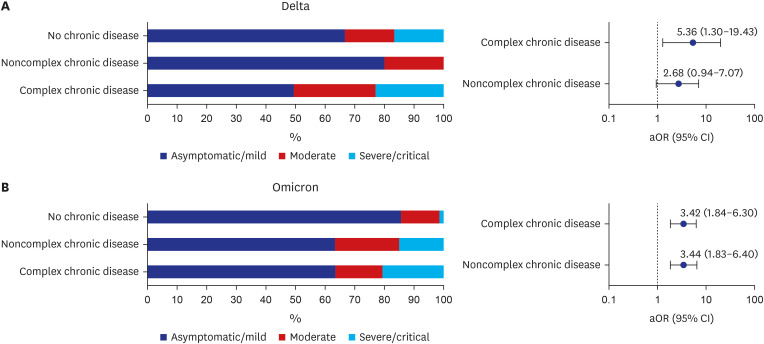
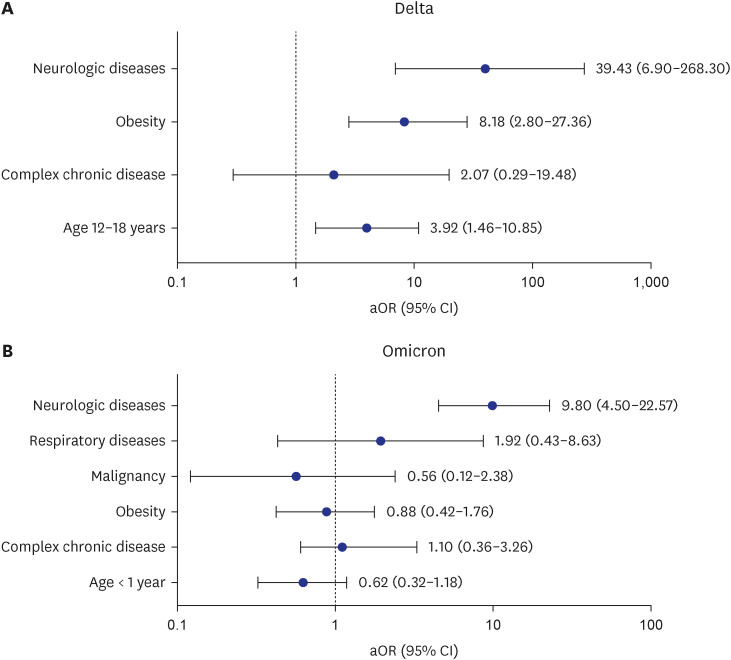
In total, 612 hospitalized patients were identified (211, delta; 401, omicron). During the omicron and delta periods, the proportions of individuals with serious illness (moderate, severe, and critical severity) were 21.2% and 11.8%, respectively (P = 0.034). Compared with the delta period, the proportions of patients with moderate illness increased significantly in the age groups of 0–4 years (14.2% vs. 3.4%) and 5–11 years (18.6% vs. 4.2%) during the omicron period. During the two periods, the proportions of patients with complex chronic diseases (delta, 16.0% vs. 4.3%, P = 0.040; omicron, 27.1% vs. 12.7%; P= 0.002), respiratory diseases except for asthma (delta, 8.0% vs. 0.0%, P = 0.013; omicron, 9.4% vs. 1.6%; P = 0.001), and neurologic diseases (delta, 28.0% vs. 3.2%, P < 0.001; omicron, 40.0% vs. 5.1%, P < 0.001) were significantly higher in patients with serious illness than in those with nonserious illness. During the delta period, the risk for serious illness was higher among patients with obesity (adjusted odds ratio [aOR], 8.18; 95% confidence interval [CI], 2.80–27.36) and neurologic diseases (aOR, 39.43; 95% CI, 6.90–268.3) and aged 12–18 years (aOR, 3.92; 95% CI, 1.46–10.85). However, the presence of neurologic disease (aOR, 9.80; 95% CI, 4.50–22.57) was the only risk factor for serious illness during the omicron period. During the omicron period, the proportions of patients with croup (11.0% vs. 0.5%) and seizures (13.2% vs. 2.8%) increased significantly compared with the delta period.
Conclusion
Compared with the delta period, the proportions of young children and patients with complex comorbidities were higher during the omicron period in Korea. Patients
Keyword
Figure
Reference
-
1. World Health Organization. Classification of omicron (B.1.1.529): SARS-CoV-2 variant of concern. Updated 2021. Accessed April 30, 2022. https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern .2. Kim EY, Choe YJ, Park H, Jeong H, Chung JH, Yu J, et al. Community transmission of SARS-CoV-2 omicron variant, South Korea, 2021. Emerg Infect Dis. 2022; 28(4):898–900. PMID: 35171760.3. Korea Disease Control and Prevention Agency. Coronavirus disease 2019 (COVID-19), Republic of Korea. Updated 2022. Accessed September 13, 2022. https://ncov.kdca.go.kr/en/ .4. Marks KJ, Whitaker M, Anglin O, Milucky J, Patel K, Pham H, et al. Hospitalizations of children and adolescents with laboratory-confirmed COVID-19 - COVID-NET, 14 states, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(7):271–278. PMID: 35176003.5. Butt AA, Dargham SR, Loka S, Shaik RM, Chemaitelly H, Tang P, et al. Coronavirus disease 2019 disease severity in children infected with the omicron variant. Clin Infect Dis. 2022; 75(1):e361–e367.6. Cloete J, Kruger A, Masha M, du Plessis NM, Mawela D, Tshukudu M, et al. Paediatric hospitalisations due to COVID-19 during the first SARS-CoV-2 omicron (B.1.1.529) variant wave in South Africa: a multicentre observational study. Lancet Child Adolesc Health. 2022; 6(5):294–302. PMID: 35189083.7. Forrest CB, Burrows EK, Mejias A, Razzaghi H, Christakis D, Jhaveri R, et al. Severity of acute COVID-19 in children <18 years old March 2020 to December 2021. Pediatrics. 2022; 149(4):e2021055765. PMID: 35322270.8. Marks KJ, Whitaker M, Agathis NT, Anglin O, Milucky J, Patel K, et al. Hospitalization of infants and children aged 0-4 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(11):429–436. PMID: 35298458.9. Tagarro A, Coya ON, Pérez-Villena A, Iglesias B, Navas A, Aguilera-Alonso D, et al. Features of COVID-19 in children during the omicron wave compared with previous waves in Madrid, Spain. Pediatr Infect Dis J. 2022; 41(5):e249–e251.10. Wang L, Berger NA, Kaelber DC, Davis PB, Volkow ND, Xu R. Incidence rates and clinical outcomes of SARS-CoV-2 infection with the omicron and delta variants in children younger than 5 years in the US. JAMA Pediatr. 2022; 176(8):811–813. PMID: 35363246.11. Choi YY, Choi SH, Choi JH, Kim DH, Lee JK, Eun BW, et al. SARS-CoV-2-naïve Korean children and adolescents hospitalized with COVID-19 in 2021. J Korean Med Sci. 2022; 37(42):e303. PMID: 36325607.12. Simon TD, Haaland W, Hawley K, Lambka K, Mangione-Smith R. Development and validation of the pediatric medical complexity algorithm (PMCA) version 3.0. Acad Pediatr. 2018; 18(5):577–580. PMID: 29496546.13. Simon TD, Cawthon ML, Stanford S, Popalisky J, Lyons D, Woodcox P, et al. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014; 133(6):e1647–e1654. PMID: 24819580.14. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61(5):135–149. PMID: 29853938.15. Iuliano AD, Brunkard JM, Boehmer TK, Peterson E, Adjei S, Binder AM, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods - United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(4):146–152. PMID: 35085225.16. Shi DS, Whitaker M, Marks KJ, Anglin O, Milucky J, Patel K, et al. Hospitalizations of children aged 5-11 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(16):574–581. PMID: 35446827.17. Solís-García G, Chacón-Pascual A, González Martínez F, Miranda Herrero MC, Hernández-Sampelayo T, Catalán Alonso P, et al. Neurologic complications in children hospitalized with influenza infections: prevalence, risk factors and impact on disease severity. Pediatr Infect Dis J. 2020; 39(9):789–793. PMID: 32282657.18. Rose EB, Dahl RM, Havers FP, Peacock G, Langley GE. Respiratory syncytial virus-associated hospitalizations in children with neurological disorders, 2006-2015. J Pediatric Infect Dis Soc. 2021; 10(10):951–957. PMID: 34245307.19. Havers F, Fry AM, Chen J, Christensen D, Moore C, Peacock G, et al. Hospitalizations attributable to respiratory infections among children with neurologic disorders. J Pediatr. 2016; 170:135–141.e1-5. PMID: 26687576.20. Britton PN, Blyth CC, Macartney K, Dale RC, Li-Kim-Moy J, Khandaker G, et al. The spectrum and burden of influenza-associated neurological disease in children: combined encephalitis and influenza sentinel site surveillance from Australia, 2013-2015. Clin Infect Dis. 2017; 65(4):653–660. PMID: 29017268.21. Woodruff RC, Campbell AP, Taylor CA, Chai SJ, Kawasaki B, Meek J, et al. Risk factors for severe COVID-19 in children. Pediatrics. 2022; 149(1):e2021053418. PMID: 34935038.22. Martin B, DeWitt PE, Russell S, Anand A, Bradwell KR, Bremer C, et al. Characteristics, outcomes, and severity risk factors associated with SARS-CoV-2 infection among children in the US National COVID Cohort Collaborative. JAMA Netw Open. 2022; 5(2):e2143151. PMID: 35133437.23. Yang S, Jang J, Park SY, Ahn SH, Kim SS, Park SB, et al. COVID-19 outbreak report from January 20, 2020 to January 19, 2022 in the Republic of Korea. Public Health Wkly Rep. 2022; 15(7):414–426.24. Price AM, Olson SM, Newhams MM, Halasa NB, Boom JA, Sahni LC, et al. BNT162b2 protection against the omicron variant in children and adolescents. N Engl J Med. 2022; 386(20):1899–1909. PMID: 35353976.25. Brewster RC, Parsons C, Laird-Gion J, Hilker S, Irwin M, Sommerschield A, et al. COVID-19-associated croup in children. Pediatrics. 2022; 149(6):e2022056492. PMID: 35257175.26. Martin B, DeWitt PE, Russell S, Sanchez-Pinto LN, Haendel MA, Moffitt R, et al. Acute upper airway disease in children with the omicron (B.1.1.529) variant of SARS-CoV-2-a report from the US National COVID Cohort Collaborative. JAMA Pediatr. 2022; 176(8):819–821. PMID: 35426941.27. Murata Y, Tomari K, Matsuoka T. Children with croup and SARS-CoV-2 infection during the large outbreak of omicron. Pediatr Infect Dis J. 2022; 41(5):e249.28. Hui KP, Ho JC, Cheung MC, Ng KC, Ching RH, Lai KL, et al. SARS-CoV-2 omicron variant replication in human bronchus and lung ex vivo. Nature. 2022; 603(7902):715–720. PMID: 35104836.29. Ludvigsson JF. Convulsions in children with COVID-19 during the omicron wave. Acta Paediatr. 2022; 111(5):1023–1026. PMID: 35098577.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Household secondary attack rates and risk factors during periods of SARS-CoV-2 Delta and Omicron variant predominance in the Republic of Korea
- Vaccine Effectiveness Against Severe Disease and Death for Patients With COVID-19 During the Delta-Dominant and Omicron-Emerging Periods: A K-COVE Study
- Recombinant proteins of spike protein of SARS-CoV-2 with the Omicron receptor-binding domain induce production of highly Omicron-specific neutralizing antibodies
- Clinical Characteristics of Patients Who Contracted the SARS-CoV-2 Omicron Variant from an Outbreak in a Single Hospital
- Comparison of the Clinical and Laboratory Features of COVID-19 in Children During All Waves of the Epidemic: A Single Center Retrospective Study