Arch Hand Microsurg.
2023 Mar;28(1):1-15. 10.12790/ahm.22.0038.
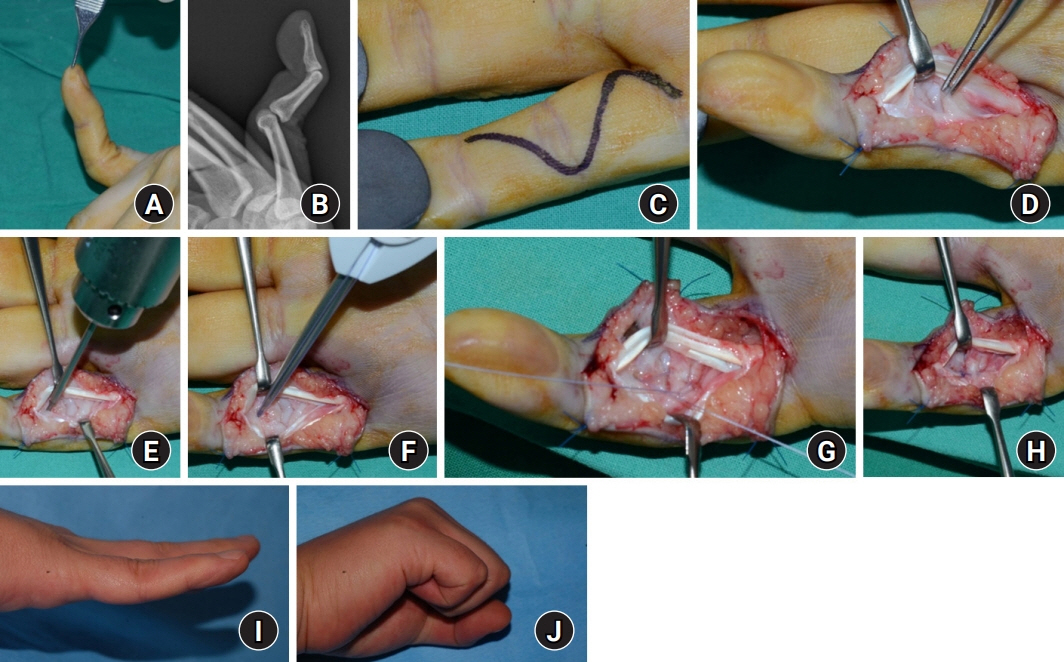
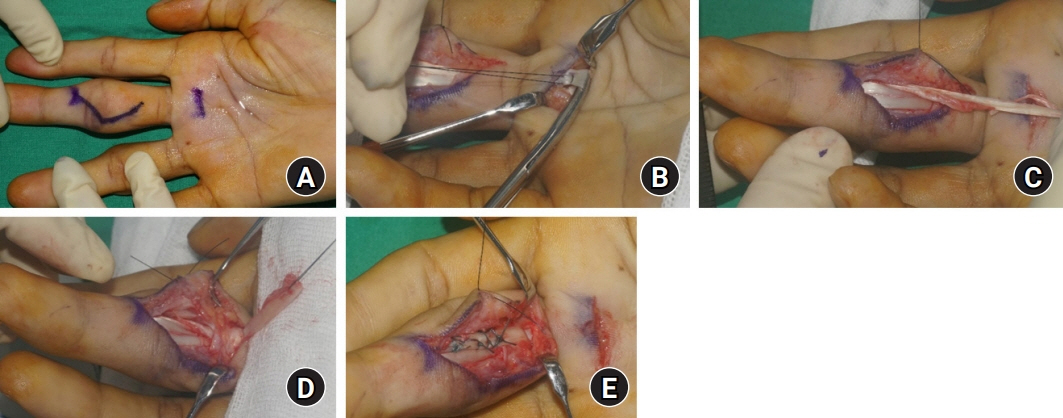
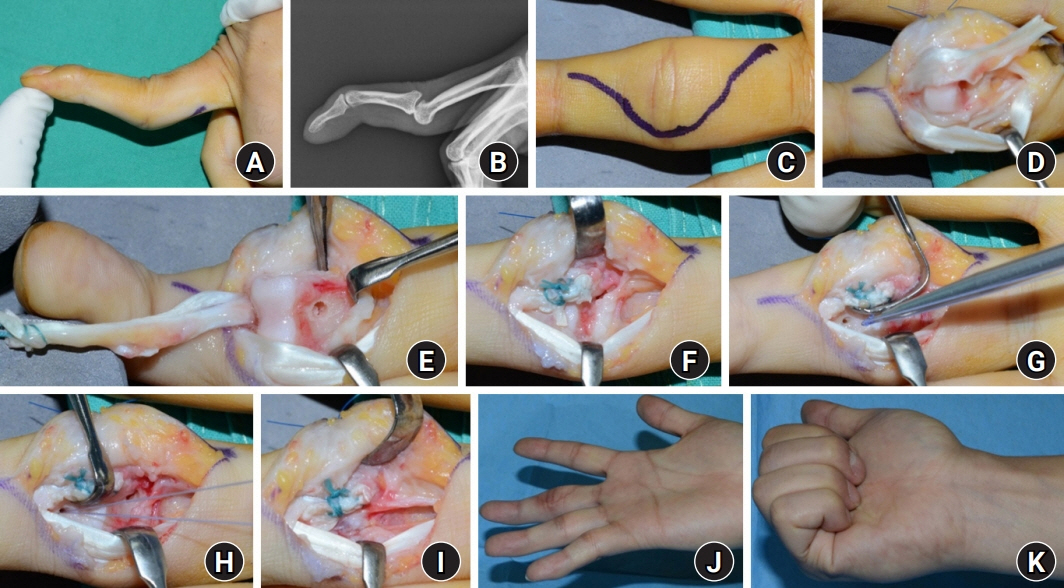
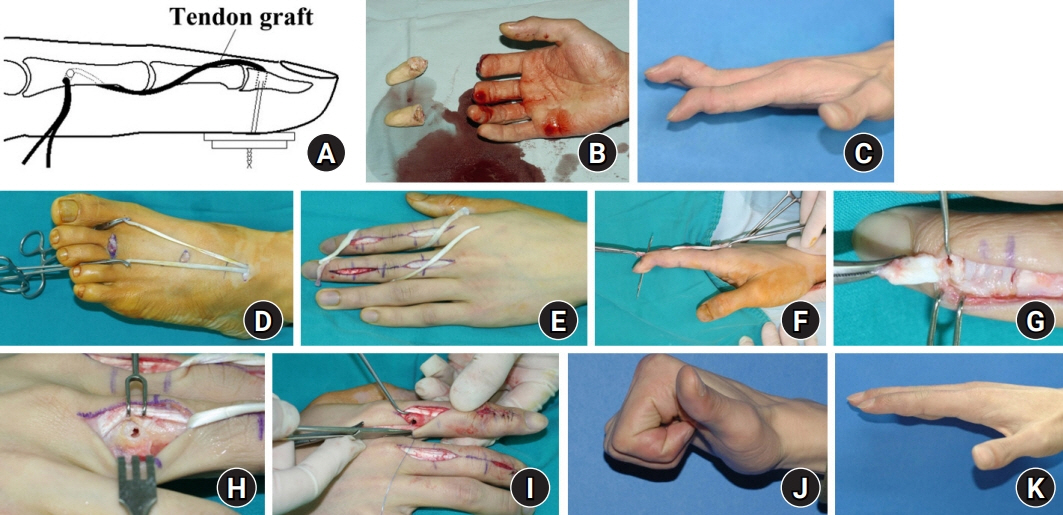
Swan neck deformity: a review of its causes and treatment options
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 2Department of Orthopaedic Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Orthopaedic Surgery, Korea University Anam Hospital, Seoul, Korea
- KMID: 2540025
- DOI: http://doi.org/10.12790/ahm.22.0038
Abstract
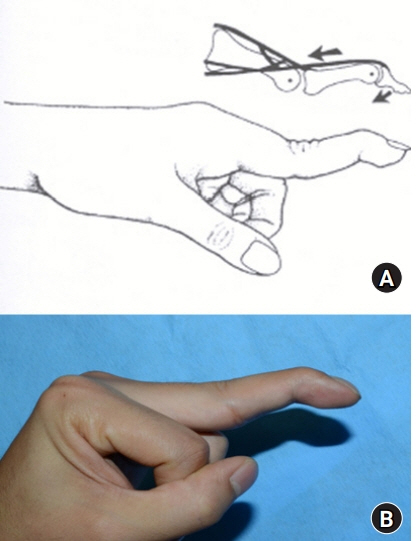
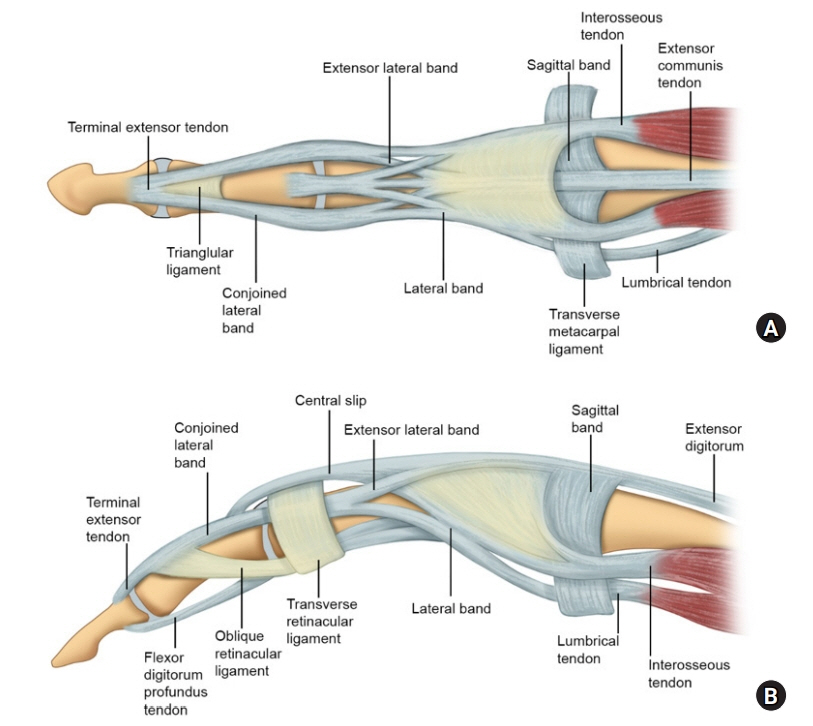
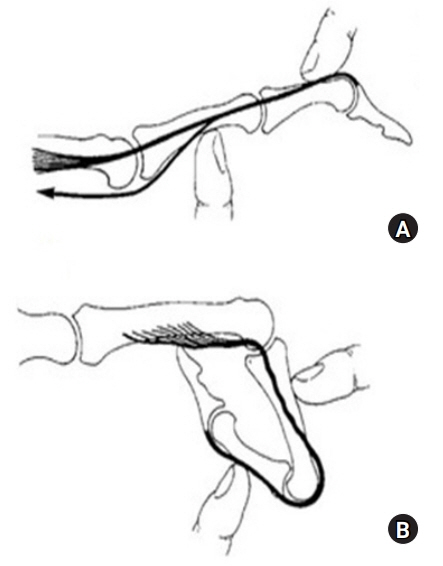
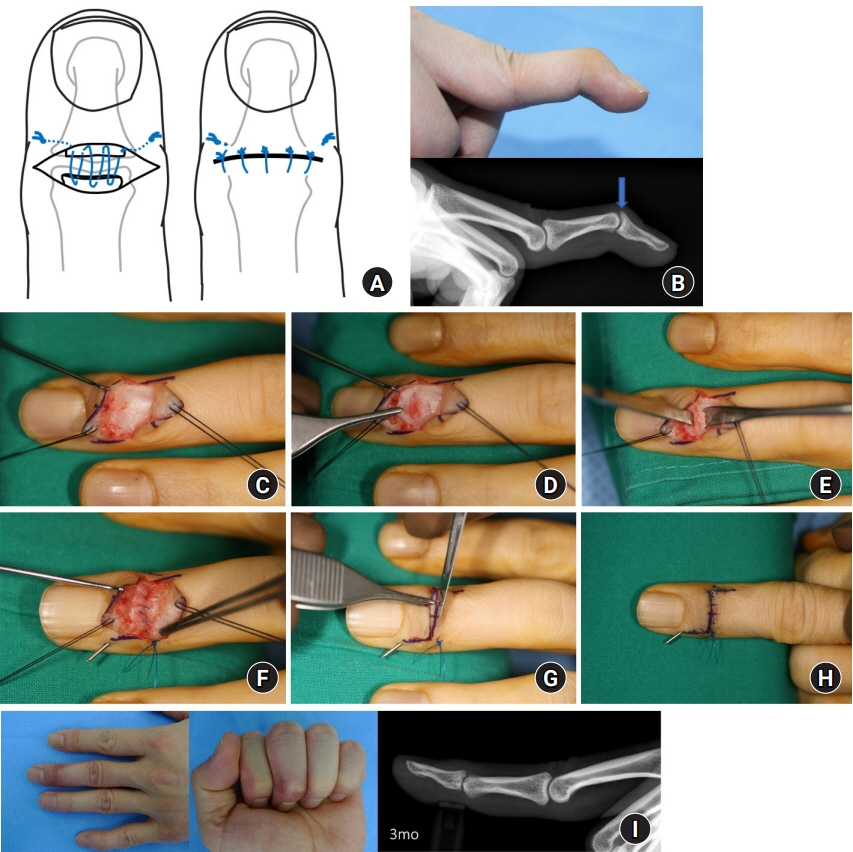
- Swan neck deformity is characterized by hyperextension of the proximal interphalangeal joint and limited extension of the distal interphalangeal joint, showing the shape of a swan’s neck. The deformity can occur either acutely or chronically. A common acute cause of this deformity is trauma, and a common chronic cause is a secondary deformity due to rheumatoid arthritis. The treatment of swan neck deformity tends to depend on the knowledge and experience of the physician because the number of cases that hand surgeons can experience is limited, and there are no clear guidelines on treatment options. This review introduces the known causes of swan neck deformity and its treatment options. For swan neck deformity, the cause of the deformity, the elapsed time, the stage of the deformity, the biomechanical relationship between adjacent joints, and the functional limitations and needs of the patients must be considered when determining the treatment method. Based on these considerations, an appropriate choice should be made between nonsurgical and surgical treatment. The patients should receive a full explanation before treatment that an optimal outcome is not always guaranteed. The treatment process requires full understanding and cooperation from the patient.
Keyword
Figure
Reference
-
References
1. Kuczynski K. The proximal interphalangeal joint: anatomy and causes of stiffness in the fingers. J Bone Joint Surg Br. 1968; 50:656–63.2. Elzinga K, Chung KC. Managing swan neck and boutonniere deformities. Clin Plast Surg. 2019; 46:329–37.3. Fox PM, Chang J. Treating the proximal interphalangeal joint in swan neck and boutonniere deformities. Hand Clin. 2018; 34:167–76.4. Howell JW, Peck F. Rehabilitation of flexor and extensor tendon injuries in the hand: current updates. Injury. 2013; 44:397–402.5. McKeon KE, Lee DH. Posttraumatic boutonnière and swan neck deformities. J Am Acad Orthop Surg. 2015; 23:623–32.6. Adkinson JM, Johnson SP, Chung KC. The clinical implications of the oblique retinacular ligament. J Hand Surg Am. 2014; 39:535–41.7. Shrewsbury MM, Johnson RK. A systematic study of the oblique retinacular ligament of the human finger: its structure and function. J Hand Surg Am. 1977; 2:194–9.8. Wehbé MA. Anatomy of the extensor mechanism of the hand and wrist. Hand Clin. 1995; 11:361–6.9. Zancolli E. Structural and dynamic bases of hand surgery. 2nd ed. Philadelphia: Lippincott;1979. p. 64–79.10. Bunnell S. Ischaemic contracture, local, in the hand. J Bone Joint Surg Am. 1953; 35-A:88–101.11. Nalebuff EA. The rheumatoid swan-neck deformity. Hand Clin. 1989; 5:203–14.12. van der Giesen FJ, Nelissen RG, van Lankveld WJ, et al. Swan neck deformities in rheumatoid arthritis: a qualitative study on the patients’ perspectives on hand function problems and finger splints. Musculoskeletal Care. 2010; 8:179–88.13. Porter BJ, Brittain A. Splinting and hand exercise for three common hand deformities in rheumatoid arthritis: a clinical perspective. Curr Opin Rheumatol. 2012; 24:215–21.14. Iselin F, Levame J, Godoy J. A simplified technique for treating mallet fingers: tenodermodesis. J Hand Surg Am. 1977; 2:118–21.15. Kon M, Bloem JJ. Treatment of mallet fingers by tenodermodesis. Hand. 1982; 14:174–5.16. Georgescu AV, Capota IM, Matei IR. A new surgical treatment for mallet finger deformity: deepithelialised pedicled skin flap technique. Injury. 2013; 44:351–5.17. Murray PM. Treatment of the osteoarthritic hand and thumb. In : Wolfe S, Pederson W, Kozin SH, Cohen M, editors. Green’s operative hand surgery. 8th ed. Philadelphia: Elsevier;2021. p. 345–372.18. Han SH, Cha YS, Song WT. Arthrodesis of distal interphalangeal joints in the hand with interosseous wiring and intramedullary K-wire fixation. Clin Orthop Surg. 2014; 6:401–4.19. Lee JK, Lee S, Choi S, et al. Distal interphalangeal joint arthrodesis using only kirschner wires in small distal phalanges. Handchir Mikrochir Plast Chir. 2021; 53:462–6.20. Kiziridis G, Giddins GE. Volar tenodesis for the treatment of swan-neck deformity; a systematic review. J Hand Surg Asian Pac Vol. 2017; 22:267–74.21. Hiwatari R, Kuniyoshi K, Aoki M, Hashimoto K, Suzuki T, Takahashi K. Fractional Fowler tenotomy for chronic mallet finger: a cadaveric biomechanical study. J Hand Surg Am. 2012; 37:2263–8.22. Bowers WH, Hurst LC. Chronic mallet finger: the use of Fowler’s central slip release. J Hand Surg Am. 1978; 3:373–6.23. Lucas GL. Fowler central slip tenotomy for old mallet deformity. Plast Reconstr Surg. 1987; 80:92–4.24. Rozmaryn LM. Central slip tenotomy with distal repair in the treatment of severe chronic mallet fingers. J Hand Surg Am. 2014; 39:773–8.25. Grundberg AB, Reagan DS. Central slip tenotomy for chronic mallet finger deformity. J Hand Surg Am. 1987; 12:545–7.26. Houpt P, Dijkstra R, Storm van Leeuwen JB. Fowler’s tenotomy for mallet deformity. J Hand Surg Br. 1993; 18:499–500.27. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980; 5:260–8.28. Wollstein R, Watson HK, Carlson L. A technique for the repair of chronic volar plate avulsion of the proximal interphalangeal joint: a review of 54 cases. Plast Reconstr Surg. 2006; 117:1239–47.29. Nalebuff EA, Millender LH. Surgical treatment of the swan-neck deformity in rheumatoid arthritis. Orthop Clin North Am. 1975; 6:733–52.30. Curtis R. Sublimis tenodesis. In : Edmonson A, Crenshaw A, editors. Campbell’s operative orthopaedics. 6th ed. St. Louis: C.V. Mosby;1980. p. 319.31. Karthaus RP, van der Werf GJ. Operative correction of posttraumatic and congenital swanneck deformity-a new technique. J Hand Surg Br. 1986; 11:239–42.32. Wei DH, Terrono AL. Superficialis sling (flexor digitorum superficialis tenodesis) for swan neck reconstruction. J Hand Surg Am. 2015; 40:2068–74.33. Caviglia D, Ciolli G, Fulchignoni C, Rocchi L. Chronic post-traumatic volar plate avulsions of the finger proximal interphalangeal joint: a literature review of different surgical techniques. Orthop Rev (Pavia). 2021; 13:9058.34. Catalano LW 3rd, Skarparis AC, Glickel SZ, et al. Treatment of chronic, traumatic hyperextension deformities of the proximal interphalangeal joint with flexor digitorum superficialis tenodesis. J Hand Surg Am. 2003; 28:448–52.35. Brulard C, Sauvage A, Mares O, Wavreille G, Fontaine C. Treatment of rheumatoid swan neck deformity by tenodesis of proximal interphalangeal joint with a half flexor digitorum superficialis tendon: about 23 fingers at 61 months follow-up. Chir Main. 2012; 31:118–27.36. Littler JW. Restoration of the oblique retinacular ligament for correcting hyperextension deformity of the proximal interphalangeal joint. In : Tubiana R, editor. La main rhumatismale. Paris: Expansion Scientifique Francaise;1966. p. 159–67.37. Tonkin MA, Hughes J, Smith KL. Lateral band translocation for swan-neck deformity. J Hand Surg Am. 1992; 17:260–7.38. Charruau B, Laulan J, Saint-Cast Y. Lateral band translocation for swan-neck deformity: outcomes of 41 digits after a mean follow-up of eight years. Orthop Traumatol Surg Res. 2016; 102(4 Suppl):S221–4.39. Gainor BJ, Hummel GL. Correction of rheumatoid swan-neck deformity by lateral band mobilization. J Hand Surg Am. 1985; 10:370–6.40. Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament (SORL). J Hand Surg Am. 1978; 3:482–7.41. Oh JY, Kim JS, Lee DC, et al. Comparative study of spiral oblique retinacular ligament reconstruction techniques using either a lateral band or a tendon graft. Arch Plast Surg. 2013; 40:773–8.42. Kanaya K, Wada T, Yamashita T. The Thompson procedure for chronic mallet finger deformity. J Hand Surg Am. 2013; 38:1295–300.43. Kleinman WB, Petersen DP. Oblique retinacular ligament reconstruction for chronic mallet finger deformity. J Hand Surg Am. 1984; 9:399–404.44. Carlson EJ, Carlson MG. Treatment of swan neck deformity in cerebral palsy. J Hand Surg Am. 2014; 39:768–72.45. Toyama S, Tokunaga D, Tsuchida S, et al. Comprehensive assessment of alterations in hand deformities over 11 years in patients with rheumatoid arthritis using cluster analysis and analysis of covariance. Arthritis Res Ther. 2021; 23:66.46. Borisch N, Haubmann P. Littler tenodesis for correction of swan neck deformity in rheumatoid arthritis. Oper Orthop Traumatol. 2011; 23:232–40.47. Matsuo T, Matsuo A, Hajime T, Fukumoto S, Chen W, Iwamoto Y. Release of flexors and intrinsic muscles for finger spasticity in cerebral palsy. Clin Orthop Relat Res. 2001; (384):162–8.48. Carlson MG, Gallagher K, Spirtos M. Surgical treatment of swan-neck deformity in hemiplegic cerebral palsy. J Hand Surg Am. 2007; 32:1418–22.49. de Bruin M, van Vliet DC, Smeulders MJ, Kreulen M. Long-term results of lateral band translocation for the correction of swan neck deformity in cerebral palsy. J Pediatr Orthop. 2010; 30:67–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-Laminectomy Swan Neck Deformity in Adults
- Correction of Distal Interphalangeal Joint Extension Lag Using Spiral Oblique Retinacular Ligament Reconstruction
- Swan-Neck Deformity of the Cervical Spine Following Multiple Laminectomies in a Child with Neurofibromatosis: A case report
- Striatal Hand in Traumatic Brain Injury: A case report
- Boutonniere Deformity: A Review of Considerations before Treatment and Current Treatment Options