Arch Hand Microsurg.
2020 Dec;25(4):249-258. 10.12790/ahm.20.0056.
Boutonniere Deformity: A Review of Considerations before Treatment and Current Treatment Options
- Affiliations
-
- 1Department of Orthopaedic Surgery, Inje University Seoul Paik Hospital, Seoul, Korea
- 2Department of Orthopaedic Surgery, CHA Bundang Medical Center, Seongnam, Korea
- KMID: 2508937
- DOI: http://doi.org/10.12790/ahm.20.0056
Abstract
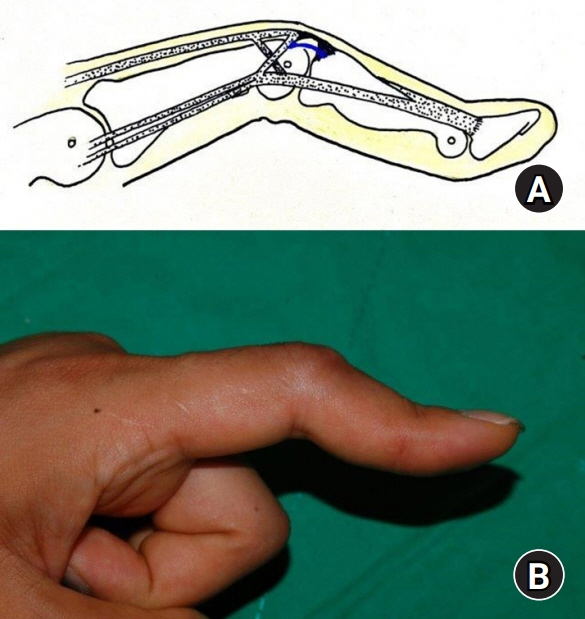
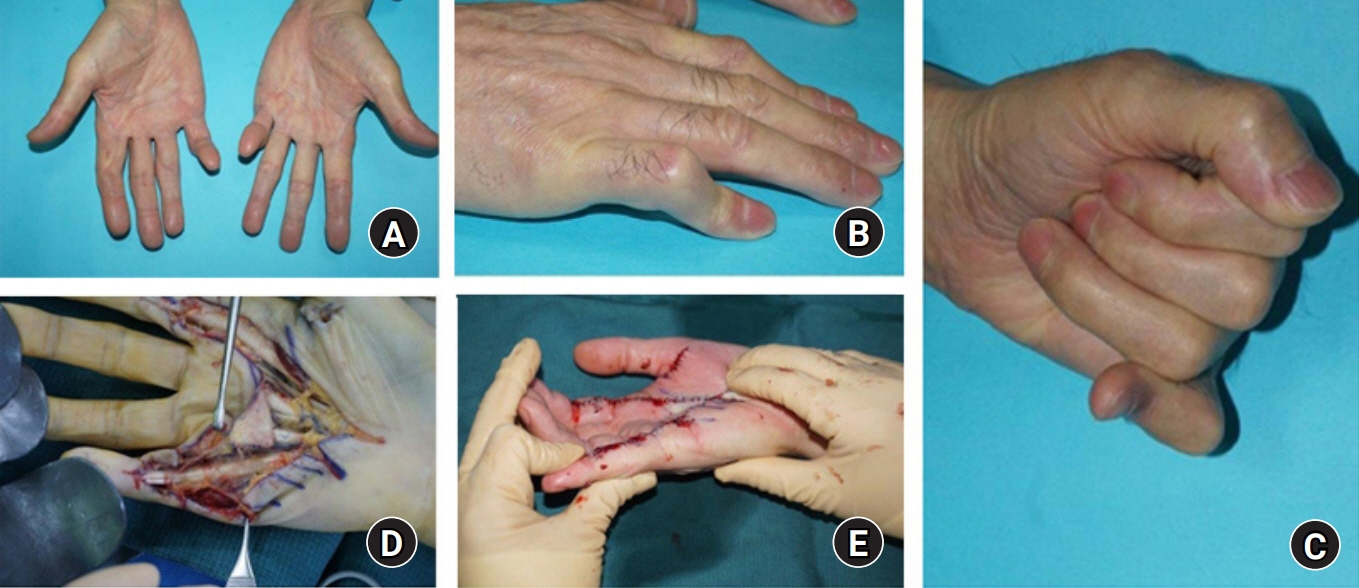
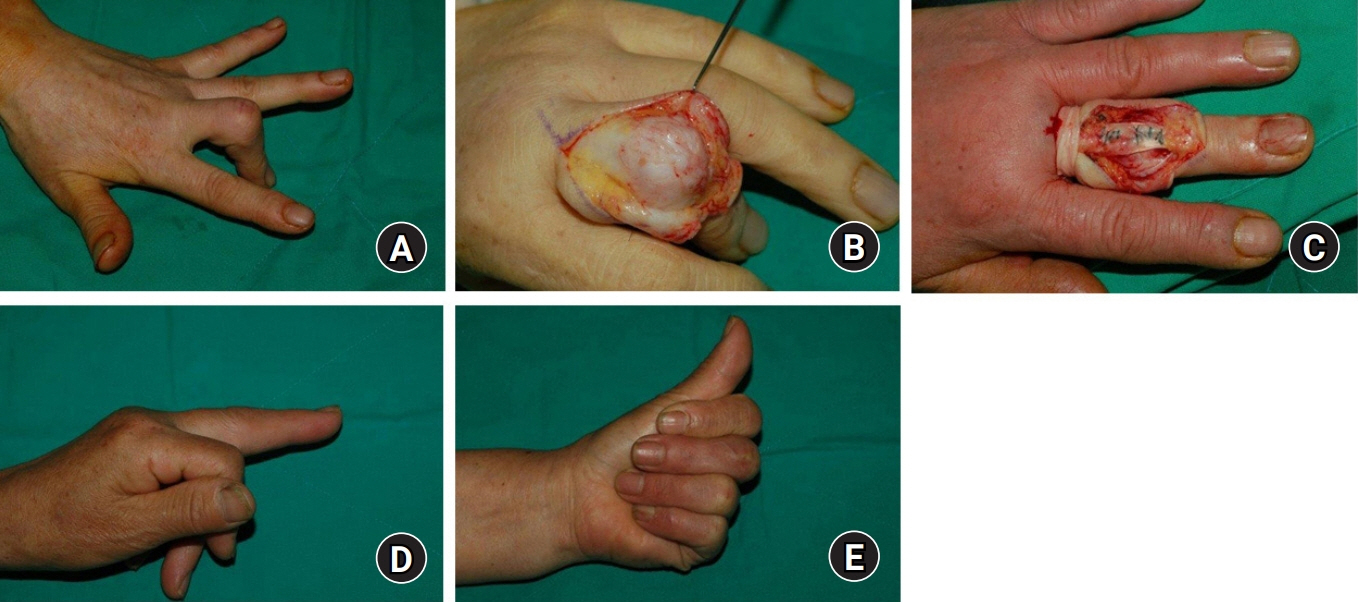
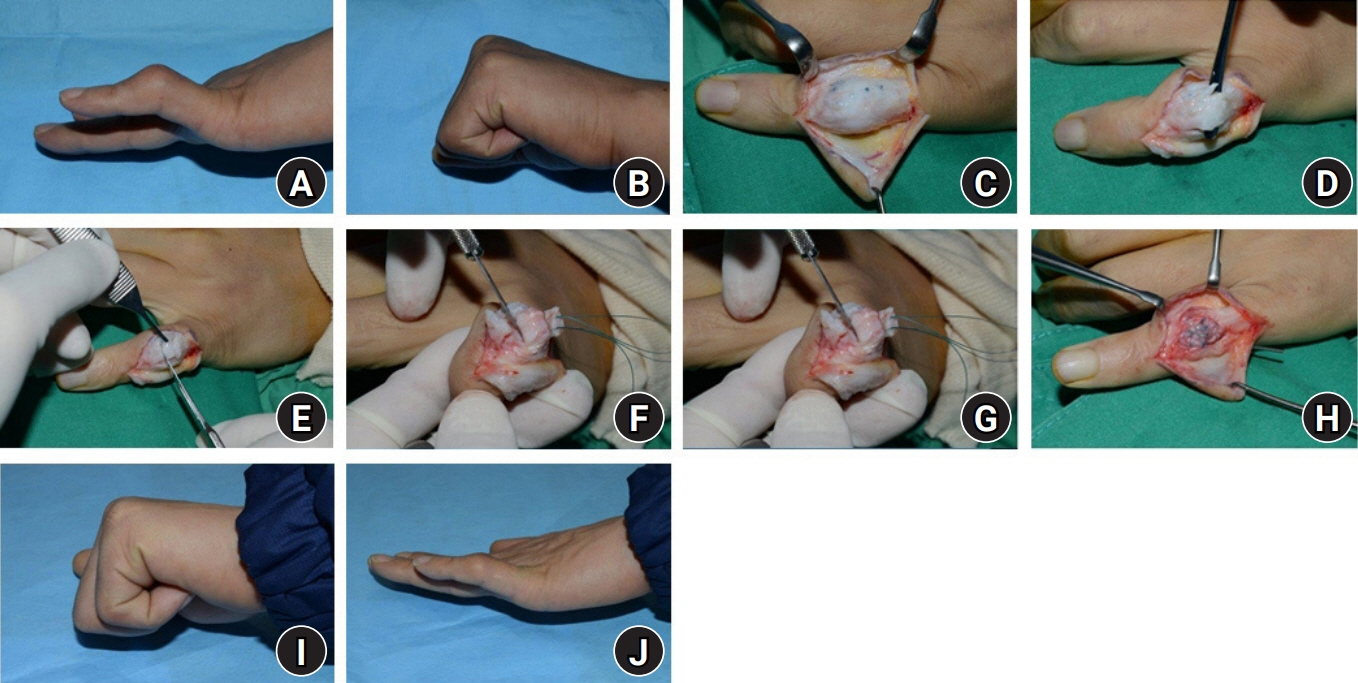
- Central slip injury is a common occurrence in hand trauma. When the base of the middle phalanx, which is the contact part of the central tendon, is weakened or damaged, extension lag or restriction would be found in the proximal interphalangeal (PIP) joint and the distal interphalangeal joint becomes hyperextended, presenting buttonhole or boutonniere deformation. Buttonhole deformation has limited cases that a hand surgeon can experience, and there is still no clear guideline for treatment, so treatment tends to depend on the knowledge and experience of the treating doctor. In this review, the factors to be considered in determining the treatment of boutonniere deformity are discussed, and nonsurgical or surgical treatment is considered. Treatment of the PIP joint in boutonniere deformity is a difficult task. Understanding the cause of the deformity, the time point and the stage of deformity, the relationship to the biomechanical changes in adjacent joints, the patient’s functional limitations, and the condition of the joint will improve treatment decisions and outcomes. Based on these considerations, an appropriate treatment should be chosen among nonsurgical or surgical treatments. Various surgical options were introduced but none of method guarantee the optimal outcome. Sufficient understanding of deformity and sufficient consultation and cooperation with the patient regarding the treatment process, outcome, and rehabilitation are necessary.
Figure
Reference
-
1. Wray RC, Young VL, Holtman B. Proximal interphalangeal joint sprains. Plast Reconstr Surg. 1984; 74:101–7.
Article2. Rothwell AG. Repair of the established post traumatic boutonnière deformity. Hand. 1978; 10:241–5.
Article3. Stack HG. Button hole deformity. Hand. 1971; 3:152–4.4. Souter WA. The problem of boutonniere deformity. Clin Orthop Relat Res. 1974; (104):116–33.
Article5. Grundberg AB, Reagan DS. Central slip tenotomy for chronic mallet finger deformity. J Hand Surg Am. 1987; 12:545–7.
Article6. Grau L, Baydoun H, Chen K, Sankary ST, Amirouche F, Gonzalez MH. Biomechanics of the acute boutonniere deformity. J Hand Surg Am. 2018; 43:80.
Article7. Clavero JA, Golanó P, Fariñas O, Alomar X, Monill JM, Esplugas M. Extensor mechanism of the fingers: MR imaging-anatomic correlation. Radiographics. 2003; 23:593–611.
Article8. Posner MA, Green SM. Diagnosis and treatment of finger deformities following injuries to the extensor tendon mechanism. Hand Clin. 2013; 29:269–81.
Article9. Fox PM, Chang J. Treating the proximal interphalangeal joint in swan neck and boutonniere deformities. Hand Clin. 2018; 34:167–76.
Article10. Burton RI. Extensor tendons: late reconstruction. In : Green DP, Hotchkiss RN, Pederson WC, editors. Operative hand surgery. New York: Churchill Livingstone;1988. p. 2073–116.11. Bellemère P. Treatment of chronic extensor tendons lesions of the fingers. Chir Main. 2015; 34:155–81.
Article12. McKeon KE, Lee DH. Posttraumatic boutonnière and swan neck deformities. J Am Acad Orthop Surg. 2015; 23:623–32.
Article13. Meadows SE, Schneider LH, Sherwyn JH. Treatment of the chronic boutonniere deformity by extensor tenotomy. Hand Clin. 1995; 11:441–7.
Article14. Stern PJ. Extensor tenotomy: a technique for correction of posttraumatic distal interphalangeal joint hyperextension deformity. J Hand Surg Am. 1989; 14:546–9.
Article15. Rubin J, Bozentka DJ, Bora FW. Diagnosis of closed central slip injuries. A cadaveric analysis of non-invasive tests. J Hand Surg Br. 1996; 21:614–6.16. Johnsson PM, Eberhardt K. Hand deformities are important signs of disease severity in patients with early rheumatoid arthritis. Rheumatology (Oxford). 2009; 48:1398–401.
Article17. Porter BJ, Brittain A. Splinting and hand exercise for three common hand deformities in rheumatoid arthritis: a clinical perspective. Curr Opin Rheumatol. 2012; 24:215–21.18. Williams K, Terrono AL. Treatment of boutonniere finger deformity in rheumatoid arthritis. J Hand Surg Am. 2011; 36:1388–93.
Article19. Boyer MI, Gelberman RH. Operative correction of swan-neck and boutonniere deformities in the rheumatoid hand. J Am Acad Orthop Surg. 1999; 7:92–100.
Article20. Kiefhaber TR, Strickland JW. Soft tissue reconstruction for rheumatoid swan-neck and boutonniere deformities: long-term results. J Hand Surg Am. 1993; 18:984–9.
Article21. Schreck MJ, Holbrook HS, Koman LA. Technique of dynamic flexor digitorum superficialis transfer to lateral bands for proximal interphalangeal joint deformity correction in severe Dupuytren disease. J Hand Surg Am. 2018; 43:192.
Article22. Kuhlmann JN, Boabighi A, Guero S, Mimoun M, Baux S. Boutonniere deformity in Dupuytren’s disease. J Hand Surg Br. 1988; 13:379–82.
Article23. Smith P, Breed C. Central slip attenuation in Dupuytren’s contracture: a cause of persistent flexion of the proximal interphalangeal joint. J Hand Surg Am. 1994; 19:840–3.
Article24. Littler JW, Eaton RG. Redistribution of forces in the correction of boutonniere deformity. J Bone Joint Surg Am. 1967; 49:1267–74.25. Caroli A, Zanasi S, Squarzina PB, Guerra M, Pancaldi G. Operative treatment of the post-traumatic boutonnière deformity. A modification of the direct anatomical repair technique. J Hand Surg Br. 1990; 15:410–5.26. To P, Watson JT. Boutonniere deformity. J Hand Surg Am. 2011; 36:139–42.
Article27. Dolphin JA. Extensor tenotomy for chronic boutonni’ere deformity of the finger: report of two cases. J Bone Joint Surg Am. 1965; 47:161–4.28. Matev I. Transposition of the lateral slips of the aponeurosis in treatment of long-standing “boutonni’ere deformity” of the fingers. Br J Plast Surg. 1964; 17:281–6.29. Pardini AG, Costa RD, Morais MS. Surgical repair of the boutonnière deformity of the fingers. Hand. 1979; 11:87–92.
Article30. Grundberg AB. Anatomic repair of boutonnière deformity. Clin Orthop Relat Res. 1980; (153):226–9.31. Souter W. A review of 101 patients with division of the central slip of the extensor expansion of the fingers. J Bone Joint Surg. 1967; 49:710–21.32. Hou Z, Zhao L, Yu S, Xiao B, Zhou J. Successful surgical repair of central slip rupture in finger extensor tendon. In Vivo. 2014; 28:599–603.33. Ahmad F, Pickford M. Reconstruction of the extensor central slip using a distally based flexor digitorum superficialis slip. J Hand Surg Am. 2009; 34:930–2.
Article34. Duzgun S, Duran A, Keskin E, Yigit AK, Buyukdogan H. Chronic boutonniere deformity: cross-lateral band technique using palmaris longus autograft. J Hand Surg Am. 2017; 42:661.
Article35. Chung MS, Yun JO, Lee KH, Baek GH, Kim SJ. Correction of the buttonhole deformity. J Korean Orhop Assoc. 1993; 28:1041–50.
Article36. Curtis RM, Reid RL, Provost JM. A staged technique for the repair of the traumatic boutonniere deformity. J Hand Surg Am. 1983; 8:167–71.
Article37. Kaplan EB. 3 anatomy, injuries and treatment of the extensor apparatus of the hand and the digits. Clin Orthop. 1959; 13:24–41.38. Steichen J, Strickland J, Call W, Powell S. Results of surgical treatment of chronic boutonniere deformity: an analysis of prognostic factors. In : Strickland J, Steichen J, editors. Difficult problems in hand surgery. St. Louis, MO: CV Mosby;1982. p. 62e69.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Boutonniere Deformity of the Thumb
- Swan neck deformity: a review of its causes and treatment options
- Boutonniere Deformity, 3 cases
- Anatomic Repair of the Central Slip with Anchor Suture Augmentation for Treatment of Established Boutonniere Deformity
- Boutonniere Deformity of the knee Following Patellectomy: A Case Report