Neurointervention.
2023 Mar;18(1):67-71. 10.5469/neuroint.2022.00465.
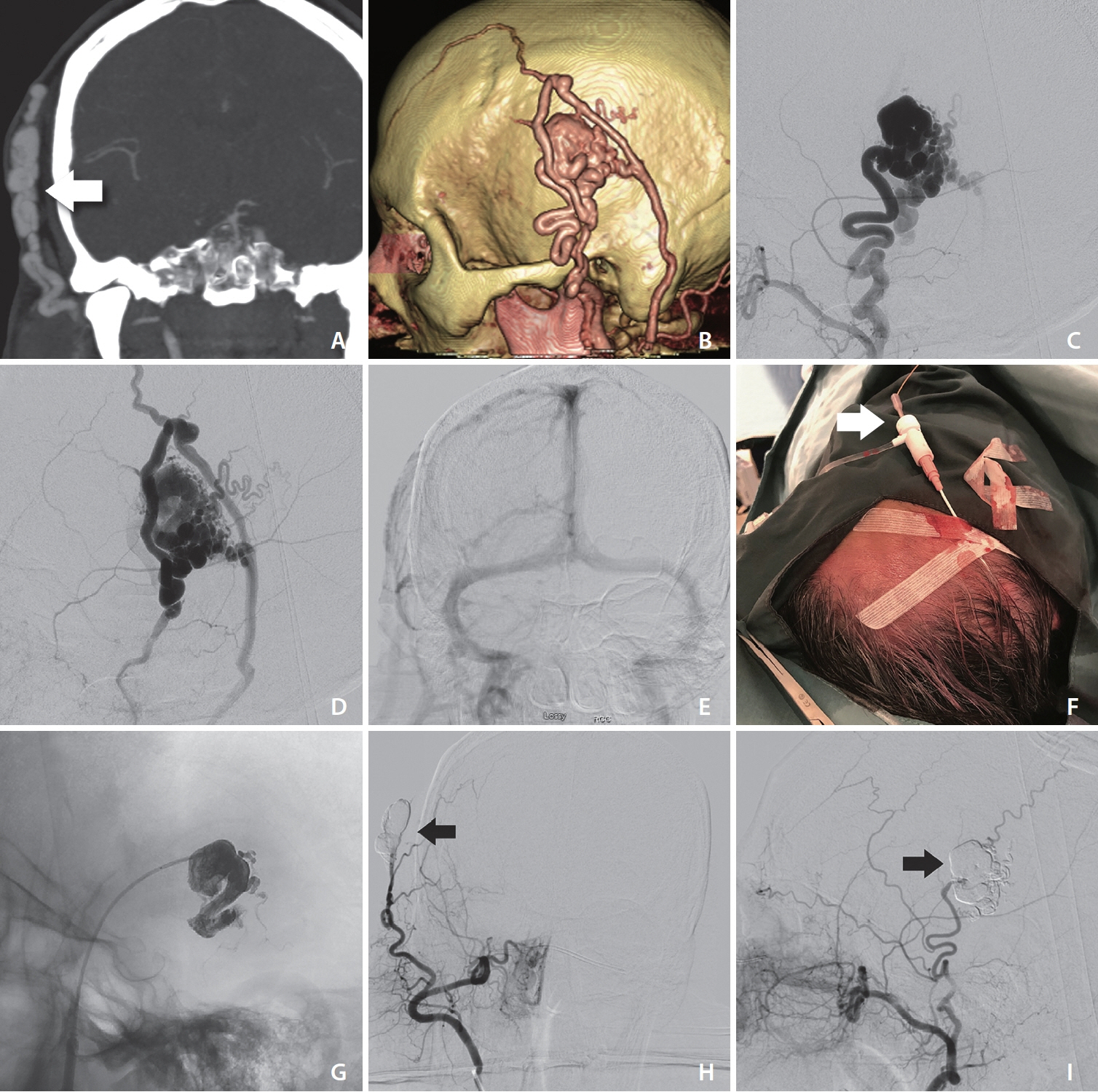
Direct Puncture of the Superficial Temporal Artery in Embolization of a Scalp Arteriovenous Fistula: A Case Report
- Affiliations
-
- 1Division of Interventional Neuroradiology, Department of Medical Imaging, The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada
- 2Division of Neurosurgery, Department of Surgery, The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada
- 3Division of Neurology, Department of Medicine, The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada
- 4Department of Anesthesiology, The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada
- 5Division of Radiology, Department of Medical Imaging, The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada
- 6Division of Neurosurgery, Department of Surgery, Royal Columbian Hospital, University of British Columbia, New Westminster, BC, Canada
- 7Division of Diagnostic and Therapeutic Neuroradiology, Department of Radiology, Vancouver General Hospital, University of British Columbia, Vancouver, BC, Canada
- KMID: 2539949
- DOI: http://doi.org/10.5469/neuroint.2022.00465
Abstract
- We describe a minimally invasive endovascular approach to treat an arteriovenous fistula of the scalp. We performed a direct puncture of the lesion through the patient’s scalp for liquid embolic agent injection along with external compression of the superficial temporal artery to perform a “manual pressure-cooker technique.” The combination of these minimally invasive techniques resulted in an excellent clinical and radiographic outcome.
Figure
Reference
-
1. Kojima D, Akamatsu Y, Fujimoto K, Oikawa K, Kashimura H, Kubo Y, et al. Utility of manual venous compression during transvenous Onyx injection for a scalp arteriovenous fistula: illustrative case. J Neurosurg Case Lessons. 2022; 4:CASE22317.
Article2. Gascón-Rubio MC, Merino-Bonilla JA, Guerra-Pérez H. Retroauricular arteriovenous fistula. Acta Otorrinolaringol Esp. 2012; 63:325–326.
Article3. Clarençon F, Shotar E, Pouvelle A, Mouyal S, Lenck S, Premat K, et al. Direct puncture of the superficial temporal artery for ethylene vinyl alcohol embolization of a type 3 arteriovenous fistula with a dual lumen balloon. J Neurointerv Surg. 2021; 13:493.
Article4. Gobin YP, Pasco A, Merland JJ, Aymard AA, Casasco A, Houdart E. Percutaneous puncture of the external carotid artery or its branches after surgical ligation. AJNR Am J Neuroradiol. 1994; 15:79–82.5. Oh JS, Yoon SM, Shim JJ, Bae HG. Transcranial direct middle meningeal artery puncture for the onyx embolization of dural arteriovenous fistula involving the superior sagittal sinus. J Korean Neurosurg Soc. 2015; 57:54–57.
Article6. Prashar A, Butt S, Shaida N. Introducing PHIL (precipitating hydrophobic injectable liquid) - a new embolic agent for the body interventional radiologist. Diagn Interv Radiol. 2020; 26:140–142.
Article7. Alawneh K, Al-Barbarawi M, Qawasmeh MA, Raffee LA, Al-Mistarehi AH. Successful use of neurovascular plug for embolization of scalp arteriovenous fistula: a novel technique. J Endovasc Ther. 2022; 29:827–834.
Article8. Koyanagi M, Mosimann PJ, Nordmeyer H, Heddier M, Krause J, Narata AP, et al. The transvenous retrograde pressure cooker technique for the curative embolization of high-grade brain arteriovenous malformations. J Neurointerv Surg. 2021; 13:637–641.
Article9. Sahu CD, Bhargava N. Intra-arterial onyx embolisation of sphenobasilar sinus fistula using pressure cooker technique: case report and review of the literature. Neuroradiol J. 2021; 34:131–134.
Article10. Zhang G, Zhu S, Wu P, Xu S, Shi H. The transvenous pressure cooker technique: a treatment for brain arteriovenous malformations. Interv Neuroradiol. 2017; 23:194–199.
Article11. Abud DG, de Castro-Afonso LH, Nakiri GS, Monsignore LM, Colli BO. Modified pressure cooker technique: an easier way to control onyx reflux. J Neuroradiol. 2016; 43:218–222.
Article12. Kamusella P, Scheer F, Lüdtke CW, Wiggermann P, Wissgott C, Andresen R. Interventional angiography: radiation protection for the examiner by using lead-free gloves. J Clin Diagn Res. 2017; 11:TC26–TC29.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of a Post-Traumatic Arteriovenous Fistula of the Superficial Temporal Artery and Vein
- Post-Traumatic Arteriovenous Fistula of the Scalp
- A Case of Traumatic Arteriovenous Fistula of the Superficial Temporal Artery
- Embolization of a Bleeding Maxillary Arteriovenous Malformation via the Superficial Temporal Artery after External Carotid Artery Ligation
- Direct Puncture Embolization of Scalp Arteriovenous Malformation in a Patient with Severe Hemophilia A: A Case Report